LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

A GLP-1 journey encompasses the complete treatment experience with glucagon-like peptide-1 receptor agonists—medications FDA-approved for type 2 diabetes and chronic weight management. This journey includes initial prescription, gradual dose escalation, ongoing monitoring, and long-term maintenance. Understanding each phase helps patients and clinicians optimize therapeutic outcomes while managing side effects. GLP-1 medications work by mimicking natural hormones that regulate blood sugar, reduce appetite, and slow digestion. With proper medical guidance, lifestyle modifications, and realistic expectations, patients can navigate this journey successfully to achieve meaningful improvements in metabolic health.
Quick Answer: A GLP-1 journey is the comprehensive treatment experience with glucagon-like peptide-1 receptor agonist medications, involving gradual dose escalation, ongoing monitoring, and typically long-term therapy for type 2 diabetes or chronic weight management.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
A GLP-1 journey refers to the comprehensive treatment experience with glucagon-like peptide-1 receptor agonists, a class of medications originally developed for type 2 diabetes and now widely prescribed for chronic weight management. This journey encompasses the entire treatment timeline—from initial prescription through dose titration, ongoing monitoring, and long-term maintenance. Understanding what to expect can help patients and clinicians optimize outcomes while minimizing adverse effects.
GLP-1 receptor agonists work by mimicking the action of endogenous GLP-1, an incretin hormone released from intestinal L-cells in response to food intake. These medications bind to GLP-1 receptors in multiple tissues, producing several therapeutic effects. In the pancreas, they enhance glucose-dependent insulin secretion and suppress glucagon release, improving glycemic control without significant hypoglycemia risk. In the brain, particularly the hypothalamus and brainstem, they reduce appetite and increase satiety signals. Additionally, GLP-1 agonists slow gastric emptying, which contributes to prolonged fullness after meals.
Currently available GLP-1 receptor agonists include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist, not a GLP-1 receptor agonist. Most of these medications are administered via subcutaneous injection, with dosing frequencies ranging from daily to once weekly depending on the specific agent. Semaglutide is also available as an oral formulation (Rybelsus) for type 2 diabetes. The FDA has approved specific GLP-1 medications for type 2 diabetes management and, in higher doses, certain agents (semaglutide 2.4 mg, liraglutide 3 mg, tirzepatide) for chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. Some agents (Wegovy, Saxenda) are also approved for weight management in adolescents aged 12 and older. These medications are not indicated for type 1 diabetes.
The typical GLP-1 journey involves gradual dose escalation over several months to minimize gastrointestinal side effects while achieving therapeutic benefit. Treatment duration varies based on individual response, tolerability, and treatment goals, though many patients require long-term or indefinite therapy to maintain benefits.
Initiating GLP-1 therapy requires careful patient selection and thorough counseling about realistic expectations. Before prescribing, clinicians should confirm appropriate indications—either inadequately controlled type 2 diabetes or obesity with BMI ≥30 kg/m² (or ≥27 kg/m² with weight-related comorbidities such as hypertension or dyslipidemia). A comprehensive medical history is essential to identify contraindications, including personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, as GLP-1 agonists carry a boxed warning regarding thyroid C-cell tumors observed in rodent studies.
Patients should undergo baseline assessments including hemoglobin A1c (for diabetes patients), renal function tests, and lipid panel. Baseline weight, blood pressure, and heart rate should be documented. Clinicians should screen for history of pancreatitis, severe gastrointestinal disease (particularly severe gastroparesis), diabetic retinopathy (particularly if intensifying glycemic control rapidly), and gallbladder disease, as these conditions may influence treatment decisions or require closer monitoring.
The initial prescription typically starts at the lowest available dose to allow physiologic adaptation. For semaglutide, this means 0.25 mg weekly for the first four weeks; for liraglutide, 0.6 mg daily for one week. Patients should receive comprehensive injection technique training, including proper subcutaneous administration in the abdomen, thigh, or upper arm, with site rotation to prevent lipohypertrophy. Storage instructions are critical—unused pens require refrigeration, while in-use pens may be kept at room temperature for specified periods.
During the first month, patients commonly experience mild to moderate nausea, which typically improves with continued use. Setting realistic expectations is crucial: weight loss is gradual, with clinical trials showing approximately 15% weight reduction with semaglutide 2.4 mg at 68 weeks and up to 21% with tirzepatide at 72 weeks, though individual responses vary considerably. For diabetes management, glycemic improvements often appear within the first few weeks. Patients should be advised to maintain adequate hydration and report severe or persistent symptoms promptly.
Patients should be counseled that these medications are not recommended during pregnancy or lactation. Women of childbearing potential should use effective contraception during treatment. For semaglutide, discontinuation at least 2 months before a planned pregnancy is recommended. With tirzepatide, decreased exposure to oral contraceptives may occur during initiation and dose escalation; backup contraception is recommended for 4 weeks after starting treatment and after each dose increase.
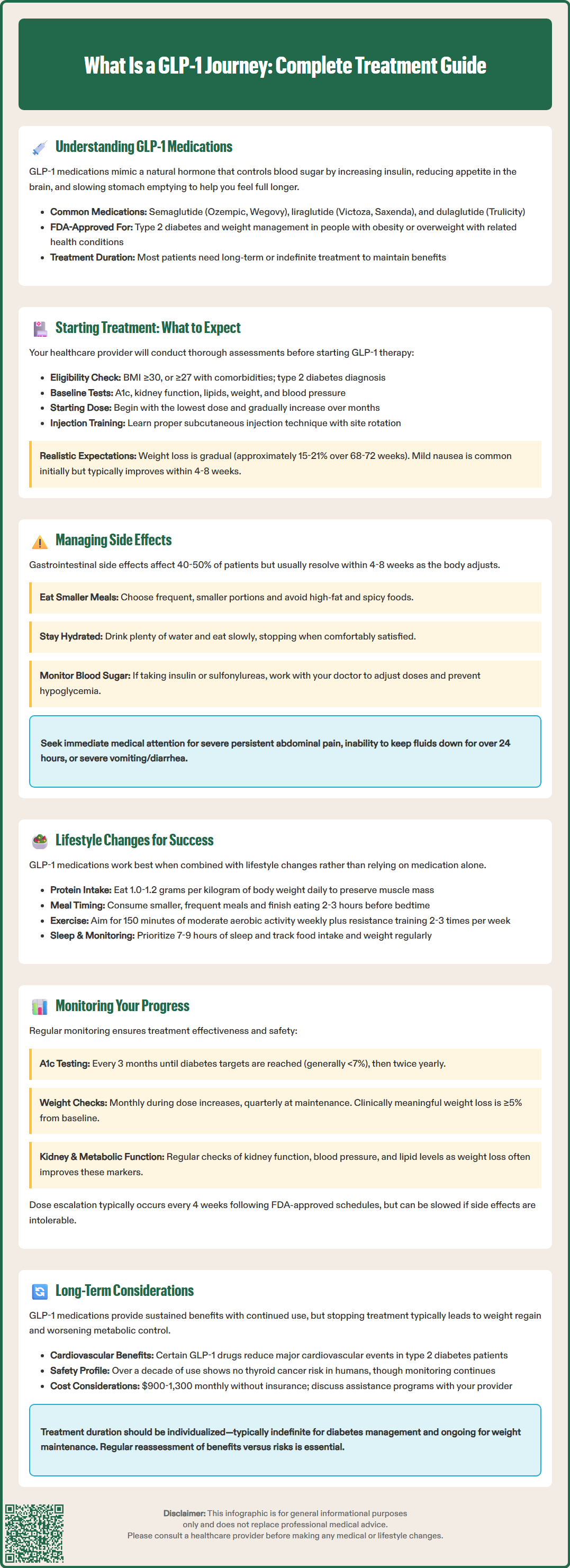
Gastrointestinal adverse effects represent the most frequent challenge during GLP-1 therapy, affecting up to 40-50% of patients to varying degrees. Nausea is the predominant symptom, particularly during dose escalation phases, followed by vomiting, diarrhea, constipation, and abdominal discomfort. These effects result from delayed gastric emptying and direct effects on the gastrointestinal tract. Most symptoms are mild to moderate, transient, and resolve within 4-8 weeks as physiologic tolerance develops.
Practical management strategies can significantly improve tolerability. Patients should eat smaller, more frequent meals rather than large portions, avoiding high-fat and heavily spiced foods that may exacerbate nausea. Eating slowly and stopping when comfortably satisfied—rather than completely full—helps accommodate delayed gastric emptying. Staying well-hydrated is essential, particularly if experiencing vomiting or diarrhea. For persistent nausea, temporary dose reduction or extending the time at a lower dose before escalation may be necessary. Patients should consult their healthcare provider before using antiemetic medications for symptom management.
Beyond gastrointestinal effects, clinicians should monitor for several less common but clinically significant adverse events. Injection site reactions—including erythema, pruritus, or induration—occur in approximately 2-5% of patients and typically resolve spontaneously. Hypoglycemia risk increases when GLP-1 agonists are combined with insulin or sulfonylureas; dose adjustments of these concomitant medications may be required. There have been postmarketing reports of acute pancreatitis, though causality remains uncertain. Patients should be counseled to seek immediate medical attention for severe, persistent abdominal pain radiating to the back, especially if accompanied by vomiting.
Gallbladder-related events, including cholelithiasis and cholecystitis, occur more frequently with GLP-1 therapy, likely related to rapid weight loss rather than direct drug effects. Patients should report right upper quadrant pain, particularly after meals. Additionally, there have been reports of worsening diabetic retinopathy in patients with pre-existing disease, possibly related to rapid glycemic improvement. Regular ophthalmologic monitoring is advisable for patients with established retinopathy.
Patients should seek urgent medical attention for red flag symptoms including severe or persistent vomiting, inability to keep fluids down for more than 24 hours, progressive abdominal distension, inability to pass stool or gas, or severe abdominal pain. These may indicate rare but serious complications such as ileus or bowel obstruction. Significant vomiting or diarrhea can lead to dehydration and acute kidney injury; early contact with healthcare providers is essential if these symptoms occur.
While GLP-1 receptor agonists produce significant metabolic benefits independently, combining pharmacotherapy with comprehensive lifestyle modification enhances outcomes and promotes sustainable health improvements. The American Diabetes Association and American College of Physicians emphasize that medication should complement—not replace—foundational lifestyle interventions including nutrition optimization, physical activity, and behavioral strategies.
Nutritional modifications are particularly important given the appetite-suppressing effects of GLP-1 therapy. Patients often experience reduced hunger and early satiety, creating risk for inadequate protein and micronutrient intake if dietary quality is poor. Clinicians should encourage nutrient-dense food choices, emphasizing lean proteins (1.0-1.2 g/kg body weight daily during active weight loss to preserve lean mass), vegetables, fruits, whole grains, and healthy fats. Adequate protein intake is crucial for maintaining muscle mass during weight reduction. Patients should avoid empty calories from sugar-sweetened beverages and ultra-processed foods, which provide minimal nutritional value.
Given delayed gastric emptying, meal timing and composition require adjustment. Smaller, more frequent meals are better tolerated than large portions. Patients should avoid lying down immediately after eating and finish meals at least 2-3 hours before bedtime to minimize reflux symptoms. Adequate hydration is important, with intake individualized based on activity level, climate, and medical conditions. Increasing dietary fiber gradually can help manage constipation, a common side effect.
Physical activity enhances weight loss, improves glycemic control, and preserves lean body mass. Current guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, plus resistance training 2-3 times per week. For patients new to exercise, gradual progression is essential. Even modest increases in daily movement—such as walking 10-15 minutes after meals—improve postprandial glucose excursions and support cardiovascular health.
Behavioral strategies including self-monitoring (food logs, weight tracking), stress management, adequate sleep (7-9 hours nightly), and social support significantly influence long-term success. Patients may benefit from referral to registered dietitians, Certified Diabetes Care and Education Specialists (CDCES), or behavioral health specialists for comprehensive support. Addressing emotional eating patterns, developing coping strategies beyond food, and building sustainable habits are essential components of the GLP-1 journey.
Systematic monitoring throughout the GLP-1 journey enables clinicians to assess therapeutic response, identify adverse effects early, and make evidence-based adjustments to optimize outcomes. The monitoring schedule should be individualized based on treatment indication, baseline comorbidities, and patient-specific factors, though general frameworks provide useful guidance.
For patients with type 2 diabetes, hemoglobin A1c should be measured at baseline and approximately every 3 months until glycemic targets are achieved, then at least twice yearly if stable. Self-monitoring of blood glucose is particularly important for patients on concomitant insulin or sulfonylureas, as GLP-1 therapy may necessitate dose reductions of these medications to prevent hypoglycemia. Target A1c is generally <7% for most adults, though individualized goals may be appropriate based on age, comorbidities, and hypoglycemia risk.
Weight should be monitored at each clinical encounter, typically monthly during active dose titration and quarterly once maintenance dose is achieved. Clinically meaningful weight loss is generally defined as ≥5% reduction from baseline, with many patients achieving 10-15% or greater reduction over 6-12 months. If weight loss plateaus or is less than expected after 3-4 months at the maintenance dose, clinicians should reassess adherence, evaluate for medication interactions, and reinforce lifestyle modifications. In some cases, switching to a different GLP-1 agonist or considering FDA-approved combination therapy under specialist guidance may be appropriate.
Renal function monitoring is important, particularly during episodes of dehydration from gastrointestinal side effects. Baseline serum creatinine and estimated glomerular filtration rate should be documented, with repeat testing if patients experience significant vomiting or diarrhea. Most GLP-1 agonists do not require dose adjustment for mild to moderate renal impairment, though specific agents have varying recommendations for severe impairment.
Lipid panels and blood pressure should be reassessed periodically, as weight loss and improved glycemic control often lead to favorable changes in these cardiovascular risk factors. Dose adjustments of antihypertensive or lipid-lowering medications may be necessary. For patients with pre-existing diabetic retinopathy, ophthalmologic follow-up is recommended, particularly during periods of rapid glycemic improvement.
Dose escalation should proceed according to FDA-approved titration schedules, typically every 4 weeks, though individual tolerance may necessitate slower progression. If patients experience intolerable side effects at a given dose, maintaining the current dose for an additional 4 weeks or temporarily reducing the dose may improve tolerance before attempting further escalation.
As GLP-1 receptor agonists transition from short-term interventions to long-term or indefinite therapy for many patients, understanding the implications of extended use becomes increasingly important. Current evidence suggests that benefits—both glycemic control and weight reduction—are maintained with continued treatment, but discontinuation frequently results in weight regain and worsening of metabolic parameters. This has led to conceptualizing obesity as a chronic disease requiring ongoing management rather than a condition amenable to short-term cure.
Cardiovascular outcomes trials have demonstrated significant benefits of certain GLP-1 agonists beyond glycemic control. Semaglutide, liraglutide, and dulaglutide have shown reductions in major adverse cardiovascular events (MACE) in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors. In 2024, semaglutide 2.4 mg (Wegovy) received FDA approval for cardiovascular risk reduction in adults with established cardiovascular disease and either overweight or obesity, based on the SELECT trial. According to current American Diabetes Association guidelines, GLP-1 receptor agonists are preferred agents for patients with atherosclerotic cardiovascular disease, while SGLT2 inhibitors are preferred for heart failure or chronic kidney disease. The mechanisms potentially contributing to cardiovascular protection may include effects on weight, glycemic control, blood pressure, and possibly direct effects on vascular inflammation and lipid metabolism, though these mechanisms remain under investigation.
Long-term safety data, while accumulating, remain somewhat limited compared to older diabetes medications. The theoretical thyroid cancer risk based on rodent studies has not materialized in human populations after over a decade of clinical use, though ongoing pharmacovigilance continues. For patients with weight-management indications, monitoring for suicidality is recommended, as these medications carry warnings about suicidal thoughts and behaviors. Bone health should be considered during significant weight loss, particularly in older adults or those with osteoporosis risk factors. Ensuring adequate calcium, vitamin D, and protein intake, along with weight-bearing exercise, helps preserve bone health during weight reduction.
Cost and access represent significant practical considerations for long-term therapy. GLP-1 agonists are expensive, with monthly costs often exceeding $900-1,300 without insurance coverage. Insurance authorization requirements, prior authorization denials, and coverage limitations create barriers to initiation and continuation. Patients should be counseled about potential out-of-pocket costs and available manufacturer assistance programs before starting therapy. Supply shortages have also periodically affected availability, requiring contingency planning.
The question of treatment duration remains incompletely answered. For diabetes management, indefinite therapy is generally appropriate as long as benefits persist and the medication is tolerated. For weight management, some patients may attempt discontinuation after achieving goals, though most will require ongoing treatment to maintain weight loss. Gradual dose reduction rather than abrupt cessation may minimize rebound effects, though optimal discontinuation strategies require further study. Ultimately, the decision to continue or discontinue GLP-1 therapy should be individualized, considering treatment response, tolerability, patient preferences, cost, and overall health status. Regular reassessment of the risk-benefit balance ensures that therapy remains appropriate as patients' clinical circumstances evolve.
Most patients require long-term or indefinite GLP-1 therapy to maintain benefits, as discontinuation typically results in weight regain and worsening metabolic parameters. Treatment duration is individualized based on response, tolerability, and clinical goals.
Gastrointestinal effects—particularly nausea, vomiting, diarrhea, and constipation—affect 40-50% of patients, especially during dose escalation. These symptoms are typically mild to moderate and resolve within 4-8 weeks as tolerance develops.
Most patients experience weight regain after discontinuing GLP-1 therapy, as obesity is a chronic condition requiring ongoing management. The decision to continue or discontinue should be individualized with your healthcare provider based on treatment response, tolerability, and overall health status.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.