LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
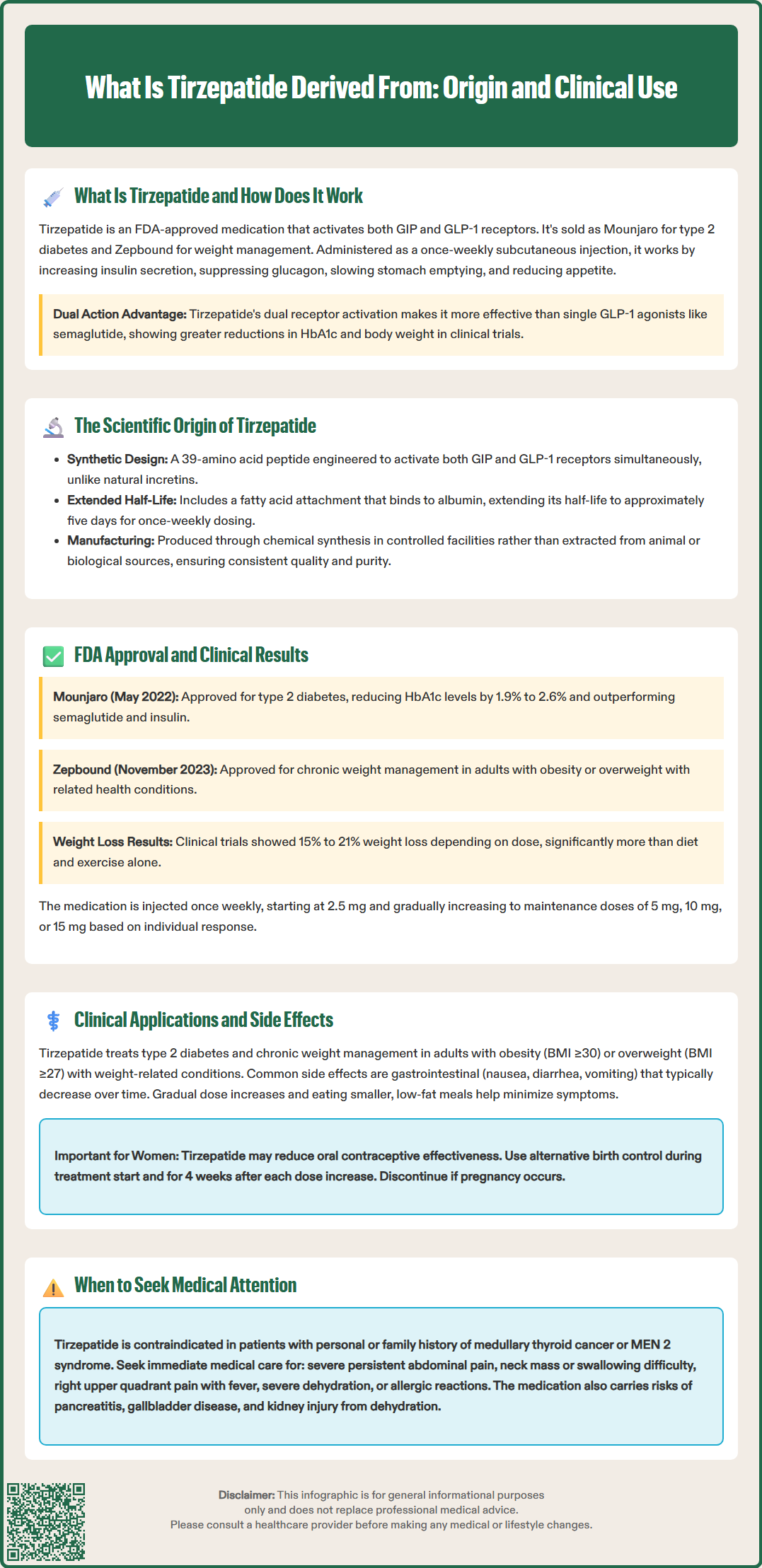
Tirzepatide is a synthetic peptide medication derived from the structure of human gastric inhibitory polypeptide (GIP), engineered to activate both GIP and glucagon-like peptide-1 (GLP-1) receptors. Unlike naturally occurring incretins, tirzepatide was created through rational drug design to produce dual receptor activation for enhanced metabolic effects. Approved by the FDA as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, this once-weekly injectable represents a significant advancement in treating metabolic disease. Understanding tirzepatide's synthetic origin and mechanism helps clinicians optimize its use in appropriate patient populations.
Quick Answer: Tirzepatide is derived from the structure of human gastric inhibitory polypeptide (GIP) and is a synthetic peptide engineered to activate both GIP and GLP-1 receptors.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a significant advancement in metabolic disease therapy through its dual incretin receptor activation.
The medication works by mimicking the action of two naturally occurring incretin hormones that play crucial roles in glucose homeostasis and appetite regulation. When administered subcutaneously once weekly, tirzepatide binds to both GIP and GLP-1 receptors, triggering multiple physiological responses. These include glucose-dependent insulin secretion from pancreatic beta cells, suppression of inappropriately elevated glucagon secretion, delayed gastric emptying, and reduced appetite through central nervous system pathways.
The dual agonist mechanism distinguishes tirzepatide from earlier GLP-1 receptor agonists such as semaglutide or dulaglutide. In the SURPASS-2 trial, tirzepatide demonstrated greater HbA1c reduction and weight loss compared to semaglutide 1 mg in type 2 diabetes. By activating GIP receptors in addition to GLP-1 receptors, tirzepatide may potentially enhance metabolic effects, though the precise contribution of GIP receptor activation to clinical outcomes continues to be investigated.
The glucose-dependent nature of tirzepatide's insulin secretion mechanism means that hypoglycemia risk remains relatively low when used as monotherapy, though caution is warranted when combined with insulin or sulfonylureas. Importantly, tirzepatide is not indicated for the treatment of type 1 diabetes or diabetic ketoacidosis.
Tirzepatide is a synthetic peptide derived from the structure of human gastric inhibitory polypeptide (GIP), also known as glucose-dependent insulinotropic polypeptide. The molecule was engineered through rational drug design to create a single peptide capable of activating both GIP and GLP-1 receptors with therapeutic potency. This represents a departure from naturally occurring incretins, which are selective for their respective receptors.
The development of tirzepatide involved modifying the native 42-amino acid GIP sequence to incorporate structural elements that confer GLP-1 receptor activity while maintaining GIP receptor agonism. The resulting 39-amino acid peptide includes a C20 fatty diacid moiety attached via a linker to a lysine residue, which enables albumin binding and extends the medication's half-life to approximately five days. This pharmacokinetic modification allows for once-weekly subcutaneous administration, improving patient adherence compared to shorter-acting agents.
The scientific rationale for dual incretin receptor activation emerged from physiological research demonstrating that GIP and GLP-1 have complementary but distinct roles in metabolic regulation. While GLP-1 primarily mediates glucose-dependent insulin secretion and appetite suppression, GIP influences insulin secretion and, based on preclinical studies, may affect lipid metabolism and other metabolic pathways. Preclinical research suggested that simultaneous activation of both pathways might produce complementary metabolic benefits.
Tirzepatide is not derived from animal sources or extracted from biological tissues. It is produced through chemical peptide synthesis methods in controlled manufacturing environments. This synthetic origin ensures consistency, purity, and scalability for pharmaceutical production. Like other peptide therapeutics, anti-drug antibodies have been observed in clinical studies, though their clinical significance continues to be evaluated.
Tirzepatide was developed by Eli Lilly and Company through an extensive research program investigating dual incretin receptor agonism. The clinical development program included multiple phase 1, 2, and 3 trials evaluating safety, efficacy, and optimal dosing strategies in diverse patient populations. The pivotal SURPASS clinical trial program for type 2 diabetes enrolled over 10,000 participants across multiple international sites, demonstrating tirzepatide's efficacy across a range of baseline characteristics and disease severities.
The FDA approved tirzepatide under the brand name Mounjaro in May 2022 for improving glycemic control in adults with type 2 diabetes mellitus as an adjunct to diet and exercise. This approval was based on data from the SURPASS trials showing superior HbA1c reduction compared to placebo, semaglutide 1 mg, and insulin glargine. Across the program, tirzepatide demonstrated dose-dependent HbA1c reductions of 1.9% to 2.6% from baseline, with many participants achieving HbA1c targets below 7.0% and even below 5.7%.
In November 2023, the FDA granted approval for tirzepatide under the brand name Zepbound for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity. This approval followed the SURMOUNT clinical trial program, which demonstrated mean weight reductions of 15% to 21% depending on dose, significantly exceeding results seen with lifestyle intervention alone.
The approved dosing for both indications involves subcutaneous injection once weekly, with gradual dose escalation from 2.5 mg to maintenance doses of 5 mg, 10 mg, or 15 mg based on individual response and tolerability. The FDA label includes specific guidance on dose titration schedules to minimize gastrointestinal adverse effects during initiation. While metabolic outcomes are robust, dedicated cardiovascular outcomes trials for tirzepatide are still ongoing.
Tirzepatide has established clinical utility in two primary therapeutic areas: type 2 diabetes mellitus and chronic weight management. For diabetes management, tirzepatide is indicated as an adjunct to diet and exercise to improve glycemic control in adults. Clinical evidence supports its use across the spectrum of disease severity, from newly diagnosed patients to those with longstanding diabetes inadequately controlled on multiple oral agents or basal insulin. The American Diabetes Association's Standards of Care recognize GLP-1 receptor agonists with proven cardiovascular benefit as preferred agents for patients with established atherosclerotic cardiovascular disease or indicators of high cardiovascular risk. Dedicated cardiovascular outcomes trials for tirzepatide are ongoing.
In weight management, tirzepatide (Zepbound) addresses a significant need for effective pharmacotherapy in obesity treatment. It is indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity such as hypertension, dyslipidemia, obstructive sleep apnea, or cardiovascular disease. In the SURMOUNT-1 trial, participants achieved mean weight reductions of 15% to 21% from baseline depending on dose.
The most common adverse effects are gastrointestinal in nature, including nausea, diarrhea, vomiting, constipation, and abdominal discomfort. These effects are typically mild to moderate, occur most frequently during dose escalation, and tend to diminish over time. Gradual dose titration as specified in the prescribing information helps minimize these symptoms. Patients should be counseled about potential gastrointestinal effects and strategies to manage them, including eating smaller meals and avoiding high-fat foods.
Important safety considerations include:
Contraindications: Personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Pancreatitis risk: Patients should be monitored for persistent severe abdominal pain and tirzepatide discontinued if pancreatitis is suspected
Hypoglycemia: Increased risk when combined with insulin or insulin secretagogues; dose reduction of concomitant medications may be necessary
Diabetic retinopathy: Rapid improvement in glycemic control has been associated with temporary worsening of diabetic retinopathy in some diabetes trials
Acute kidney injury: Cases have been reported, often in the setting of volume depletion from gastrointestinal adverse effects
Gallbladder disease: Risk of cholelithiasis and cholecystitis may be increased
Hypersensitivity reactions: Including anaphylaxis and angioedema have been reported
Not recommended: In patients with severe gastrointestinal disease, including severe gastroparesis
Additional important counseling points:
Pregnancy: Zepbound should not be used for weight management during pregnancy; discontinue if pregnancy is recognized
Oral contraceptives: Tirzepatide may reduce the effectiveness of oral contraceptives; use alternative contraceptive methods during treatment initiation and for 4 weeks after each dose escalation
Concomitant medications: Avoid coadministration with other GLP-1 receptor agonists for weight management
Patients should be advised to seek medical attention for:
Severe, persistent abdominal pain that may radiate to the back (potential pancreatitis)
Signs of thyroid tumors including neck mass, dysphagia, dyspnea, or persistent hoarseness
Symptoms of acute gallbladder disease (right upper quadrant pain, fever, jaundice)
Severe gastrointestinal symptoms leading to dehydration
Changes in vision or signs of hypoglycemia
Signs of hypersensitivity reactions including rash, itching, or difficulty breathing
Clinicians should conduct a thorough medical history before initiating tirzepatide, including assessment for personal or family history of medullary thyroid carcinoma or MEN 2, history of pancreatitis, severe gastrointestinal disease, and diabetic retinopathy. Baseline laboratory evaluation should include HbA1c (for diabetes indication), renal function, and lipid panel. Ongoing monitoring should include assessment of glycemic control, weight, gastrointestinal tolerability, and renal function, particularly during dose escalation or in patients experiencing significant gastrointestinal adverse effects.
Referral to endocrinology may be appropriate for patients with complex diabetes requiring multiple medication adjustments, those with a history of severe hypoglycemia, or individuals with diabetic complications requiring specialized management. Referral to bariatric surgery programs should be considered for patients with BMI ≥40 kg/m² or ≥35 kg/m² with obesity-related comorbidities who may benefit from surgical intervention, either as an alternative or adjunct to pharmacotherapy.
No, tirzepatide is not derived from animal sources or extracted from biological tissues. It is a synthetic peptide produced through chemical peptide synthesis methods in controlled manufacturing environments, ensuring consistency, purity, and scalability.
Tirzepatide is a modified 39-amino acid peptide engineered from the native 42-amino acid GIP sequence. It includes structural modifications that enable GLP-1 receptor activation and a fatty acid moiety that extends its half-life to approximately five days, allowing once-weekly dosing.
Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. It should not be used during pregnancy for weight management and is not recommended in patients with severe gastrointestinal disease.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.