LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
What to eat when on weight loss injections is a critical question for anyone starting GLP-1 medications like semaglutide (Wegovy, Ozempic) or dual GIP/GLP-1 agonists like tirzepatide (Zepbound, Mounjaro). These medications significantly alter appetite and digestion by slowing gastric emptying and reducing hunger signals, making strategic food choices essential for maximizing benefits while minimizing side effects. With reduced appetite and smaller portion sizes, every meal must deliver optimal nutrition to support muscle preservation, prevent deficiencies, and manage common gastrointestinal symptoms. This guide provides evidence-based dietary recommendations to help you navigate eating patterns during weight loss injection therapy, ensuring both therapeutic success and long-term sustainability.
Quick Answer: When taking weight loss injections, prioritize lean proteins, high-fiber vegetables, complex carbohydrates in moderate portions, and adequate hydration while avoiding high-fat foods, ultra-processed items, and large meals that can worsen gastrointestinal side effects.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections work through different mechanisms depending on the medication. Semaglutide (Wegovy, Ozempic) is a glucagon-like peptide-1 (GLP-1) receptor agonist, while tirzepatide (Zepbound, Mounjaro) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. Importantly, while Wegovy and Zepbound are FDA-approved for chronic weight management, Ozempic and Mounjaro are approved only for type 2 diabetes management (though they may be prescribed off-label for weight loss).
These medications work by binding to receptors in the brain, pancreas, and gastrointestinal tract, creating multiple physiological effects that support weight reduction. They slow gastric emptying (keeping food in your stomach longer) and act on appetite centers in the brain to decrease hunger signals, food cravings, and the reward response associated with eating. Clinical trials show that semaglutide can produce approximately 15% weight loss over 68 weeks, while tirzepatide demonstrates 15-21% weight loss over 72 weeks when combined with lifestyle modifications, though individual results vary significantly.
Digestive changes are common and often most pronounced during the initial weeks of therapy or after dose escalations. The slowed gastric motility can lead to early satiety, meaning you feel full after consuming smaller portions than previously. Some people report altered taste preferences. These medications may also affect the absorption of certain oral medications, particularly with tirzepatide, which can reduce the effectiveness of oral contraceptives during initiation and dose increases.
Important safety note: These medications carry a boxed warning about the risk of thyroid C-cell tumors and are contraindicated in people with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). They should not be used during pregnancy and require discontinuation at least 2 months (semaglutide) or 1 month (tirzepatide) before a planned pregnancy.
Prioritizing nutrient-dense foods becomes particularly important when taking weight loss injections, as your reduced appetite and smaller portion sizes mean every bite must contribute meaningful nutritional value. Lean proteins should form the foundation of your diet, as they support muscle preservation during weight loss and promote satiety. Excellent choices include skinless poultry, fish (especially fatty fish like salmon for omega-3 fatty acids), eggs, Greek yogurt, cottage cheese, and plant-based options such as tofu and legumes. Aim for 1.2-1.6 grams of protein per kilogram of body weight daily to maintain lean body mass, which typically translates to 20-30 grams per meal for most adults.
High-fiber vegetables are essential for digestive health and provide volume without excessive calories. Focus on non-starchy vegetables including leafy greens (spinach, kale, arugula), cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), peppers, zucchini, and tomatoes. These foods help prevent constipation—a common side effect of these medications—while delivering vital micronutrients. Aim for 25-30 grams of fiber daily, but increase intake gradually to avoid worsening bloating or gas, especially during the first few weeks of treatment.
Complex carbohydrates in moderate portions provide sustained energy without causing rapid blood sugar spikes. Choose whole grains like quinoa, brown rice, oats, and whole wheat products. Sweet potatoes, beans, and lentils offer both complex carbohydrates and additional protein. Healthy fats in controlled amounts support hormone production and nutrient absorption; incorporate avocados, nuts, seeds, and olive oil in small quantities.
Hydration deserves special attention. Most people should drink enough fluids to maintain light-colored urine, typically 6-8 cups daily for most adults, but individual needs vary. Sip throughout the day rather than consuming large volumes at once. If you have kidney disease or heart failure, consult your healthcare provider for personalized fluid recommendations. Consider herbal teas, infused water, or diluted broths as alternatives if plain water becomes monotonous. If experiencing vomiting or diarrhea, electrolyte-containing fluids may be beneficial.
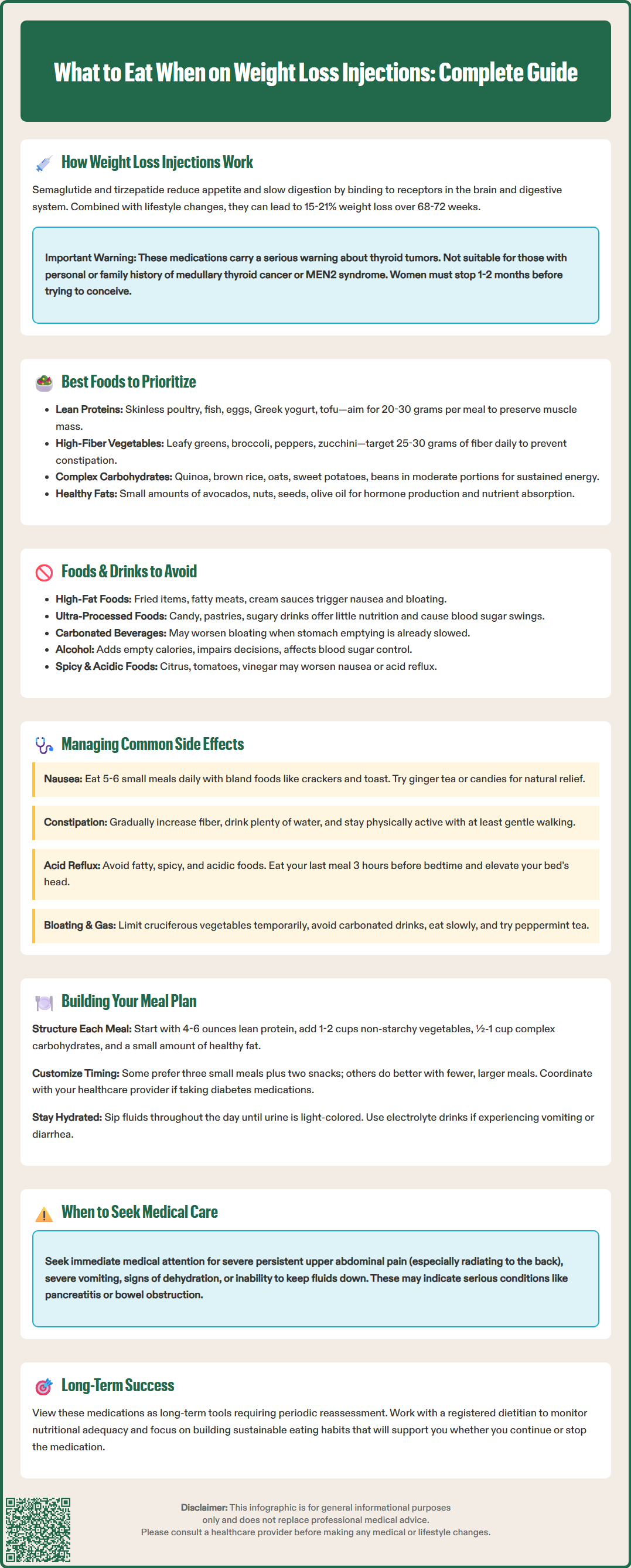
Certain foods can exacerbate the gastrointestinal side effects associated with weight loss injections or undermine your therapeutic goals. High-fat foods are particularly problematic because they delay gastric emptying even further when combined with these medications. Fried foods, fatty cuts of meat, full-fat dairy products, heavy cream sauces, and fast food can trigger nausea, bloating, and abdominal discomfort. This is especially true during the medication initiation and dose escalation periods. Very large meals of any type may also worsen gastrointestinal symptoms.
Ultra-processed foods and added sugars should be minimized for multiple reasons. These items provide minimal nutritional value while occupying limited stomach capacity, potentially leading to nutrient deficiencies. Candy, pastries, sugary cereals, and sweetened beverages can cause blood sugar fluctuations and may intensify cravings. Additionally, some patients report that their tolerance for very sweet foods decreases while on these medications, with previously enjoyed treats now tasting overly sweet or causing nausea.
Carbonated beverages may increase bloating and gastric distension in some people, which can be uncomfortable when gastric emptying is already delayed. If you notice worsening symptoms, choose non-carbonated alternatives. Alcohol warrants particular caution; it provides empty calories, can impair judgment around food choices, and may interact with blood sugar regulation. People with diabetes, especially those taking insulin or sulfonylureas, face increased hypoglycemia risk when consuming alcohol. Those with a history of pancreatitis should avoid alcohol entirely. If you choose to drink, limit intake to one serving occasionally and always consume with food.
Spicy foods and acidic items (citrus fruits, tomato-based products, vinegar-heavy dressings) may aggravate nausea or acid reflux, which can be heightened during treatment. While individual tolerance varies, it's prudent to introduce these foods cautiously and monitor your response.
Gastrointestinal side effects affect approximately 60-70% of patients initiating GLP-1 receptor agonist or dual GIP/GLP-1 therapy, though most symptoms improve within 4-8 weeks as the body adapts. Strategic dietary modifications can significantly reduce discomfort and improve treatment adherence.
For nausea, the most frequently reported side effect, several approaches prove helpful. Eat smaller, more frequent meals (5-6 times daily) rather than three large meals, as overfilling the stomach triggers discomfort. Choose bland, easily digestible foods during symptomatic periods: plain crackers, toast, rice, bananas, and applesauce (the BRAT diet components). Ginger has natural anti-nausea properties; try ginger tea, ginger candies, or fresh ginger added to meals. Avoid lying down immediately after eating, and identify personal trigger foods through careful observation. Cold or room-temperature foods may be better tolerated than hot meals, as they produce less aroma that can trigger nausea.
Constipation affects many patients due to slowed gastrointestinal motility. Gradually increase fiber intake through vegetables, fruits, whole grains, and legumes, but do so slowly to prevent gas and bloating. Prunes, flaxseeds, and chia seeds are particularly effective. Adequate hydration is critical—dehydration worsens constipation significantly. Regular physical activity, even gentle walking, stimulates bowel motility. If dietary measures prove insufficient after one week, consult your healthcare provider about appropriate laxatives; polyethylene glycol (Miralax) is often recommended as a first-line option.
Acid reflux and heartburn can be managed by avoiding trigger foods (fatty, spicy, acidic items), eating at least 3 hours before bedtime, and elevating the head of your bed. Smaller meal portions reduce gastric pressure. Bloating and gas respond well to limiting cruciferous vegetables temporarily, avoiding carbonated drinks, eating slowly, and chewing thoroughly. Peppermint tea may provide relief, though it can worsen reflux in some individuals.
Seek immediate medical attention for severe persistent upper abdominal pain (especially if radiating to the back), right upper quadrant pain with fever or jaundice, severe vomiting, signs of dehydration (extreme thirst, dizziness, dark urine), or inability to keep fluids down—these may indicate serious conditions like pancreatitis, gallbladder disease, or bowel obstruction. Your provider may temporarily pause or slow dose escalation to improve tolerability. For women taking tirzepatide with oral contraceptives, use backup contraception for 4 weeks after starting or increasing your dose.
Developing a structured yet flexible meal plan optimizes the benefits of weight loss injections while establishing habits that support long-term weight maintenance. The most successful approaches balance nutritional adequacy with practical sustainability, recognizing that these medications are tools within a comprehensive lifestyle modification program.
Start with protein-forward planning. Structure each meal around a lean protein source (4-6 ounces), then add non-starchy vegetables (1-2 cups), a moderate portion of complex carbohydrates (1/2-1 cup), and a small amount of healthy fat. A sample day might include: breakfast of Greek yogurt with berries and a tablespoon of almonds; lunch featuring grilled chicken breast over mixed greens with quinoa and olive oil dressing; an afternoon snack of hummus with vegetable sticks; and dinner of baked salmon with roasted broccoli and sweet potato. This framework ensures adequate protein while providing essential nutrients.
Meal timing and frequency require individualization. Some patients thrive on three small meals plus two snacks, while others prefer fewer, more substantial meals. If you have diabetes and take insulin or sulfonylureas, work with your healthcare provider to adjust medication timing and dosing to prevent hypoglycemia. Many find that eating their largest meal at midday rather than evening reduces nighttime discomfort.
Practical preparation strategies support adherence. Batch-cook proteins on weekends, pre-portion snacks into containers, and keep emergency options available (canned tuna, hard-boiled eggs, frozen vegetables). Restaurant dining requires planning: review menus in advance, request modifications without hesitation, and don't feel obligated to finish portions—take leftovers home.
Nutritional monitoring becomes essential with reduced caloric intake. Calorie needs vary significantly based on sex, age, weight, height, and activity level—there is no one-size-fits-all recommendation. Consider working with a registered dietitian to ensure adequacy of protein, vitamins, and minerals. Some medications may affect the absorption of certain drugs, including levothyroxine and oral contraceptives; discuss medication timing with your healthcare provider.
Long-term perspective is crucial. These medications are often continued for extended periods with periodic reassessment of benefits, risks, and coverage. Focus on developing a positive relationship with food, practicing mindful eating, and building skills that will serve you whether you continue medication or eventually discontinue it. For complex cases or persistent issues, ask about referrals to specialists in obesity medicine, endocrinology, or gastroenterology as needed.
Aim for 1.2-1.6 grams of protein per kilogram of body weight daily, typically 20-30 grams per meal for most adults. This helps preserve muscle mass during weight loss and promotes satiety with reduced caloric intake.
High-fat foods delay gastric emptying even further when combined with these medications, which can trigger or worsen nausea, bloating, and abdominal discomfort, especially during medication initiation and dose increases.
Eat smaller, more frequent meals throughout the day, choose bland foods like crackers and toast during symptomatic periods, try ginger tea or candies, and avoid lying down immediately after eating. Most nausea improves within 4-8 weeks as your body adapts.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.