LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro) is a dual GIP/GLP-1 receptor agonist approved by the FDA for type 2 diabetes, offering substantial HbA1c reductions of 1.9% to 2.6%. While effective glucose control protects against diabetic retinopathy long-term, rapid blood sugar improvements can paradoxically cause temporary retinopathy worsening in susceptible patients. Understanding tirzepatide diabetic retinopathy risk requires balancing the medication's proven glycemic benefits against the need for appropriate ophthalmologic monitoring, particularly in patients with pre-existing eye disease. Clinical trials have not identified retinopathy as a significant safety concern with tirzepatide, but prudent surveillance remains essential for all patients with diabetes.
Quick Answer: Clinical trials have not identified tirzepatide as causing increased diabetic retinopathy risk compared to placebo or other diabetes medications, though rapid glucose reduction can temporarily worsen pre-existing retinopathy in susceptible patients.
Tirzepatide is a novel glucose-lowering medication approved by the FDA in May 2022 for the treatment of type 2 diabetes mellitus in adults. Marketed under the brand name Mounjaro, tirzepatide represents a significant advancement in diabetes pharmacotherapy as the first dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The medication works through a unique dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, meaning insulin release occurs primarily when blood glucose levels are elevated. This mechanism reduces the risk of hypoglycemia compared to some other diabetes medications. Additionally, tirzepatide suppresses glucagon secretion, slows gastric emptying, and promotes satiety, which contributes to weight loss—a beneficial effect for many patients with type 2 diabetes.
Clinical trials (SURPASS program) have demonstrated that tirzepatide produces substantial reductions in hemoglobin A1c (HbA1c), with decreases ranging from 1.9% to 2.6% depending on the dose used. The medication is administered once weekly via subcutaneous injection and is available in doses of 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg. Treatment typically begins at 2.5 mg weekly (an initiation dose not intended for glycemic control), with gradual dose escalation every four weeks to minimize gastrointestinal side effects.
Tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). It is not indicated for use in type 1 diabetes.
The most common adverse effects include nausea, diarrhea, vomiting, constipation, and abdominal discomfort. These gastrointestinal symptoms are generally mild to moderate and tend to diminish over time. Additional warnings include risk of pancreatitis, gallbladder disease, acute kidney injury, hypersensitivity reactions, and caution in patients with severe gastrointestinal disease including gastroparesis. Hypoglycemia risk increases when used with insulin or insulin secretagogues, and dose reductions of these medications should be considered when initiating tirzepatide.
Importantly, tirzepatide may reduce the effectiveness of oral hormonal contraceptives due to delayed gastric emptying. Patients using oral contraceptives should consider using an additional non-hormonal method for 4 weeks after initiating tirzepatide and after each dose increase.
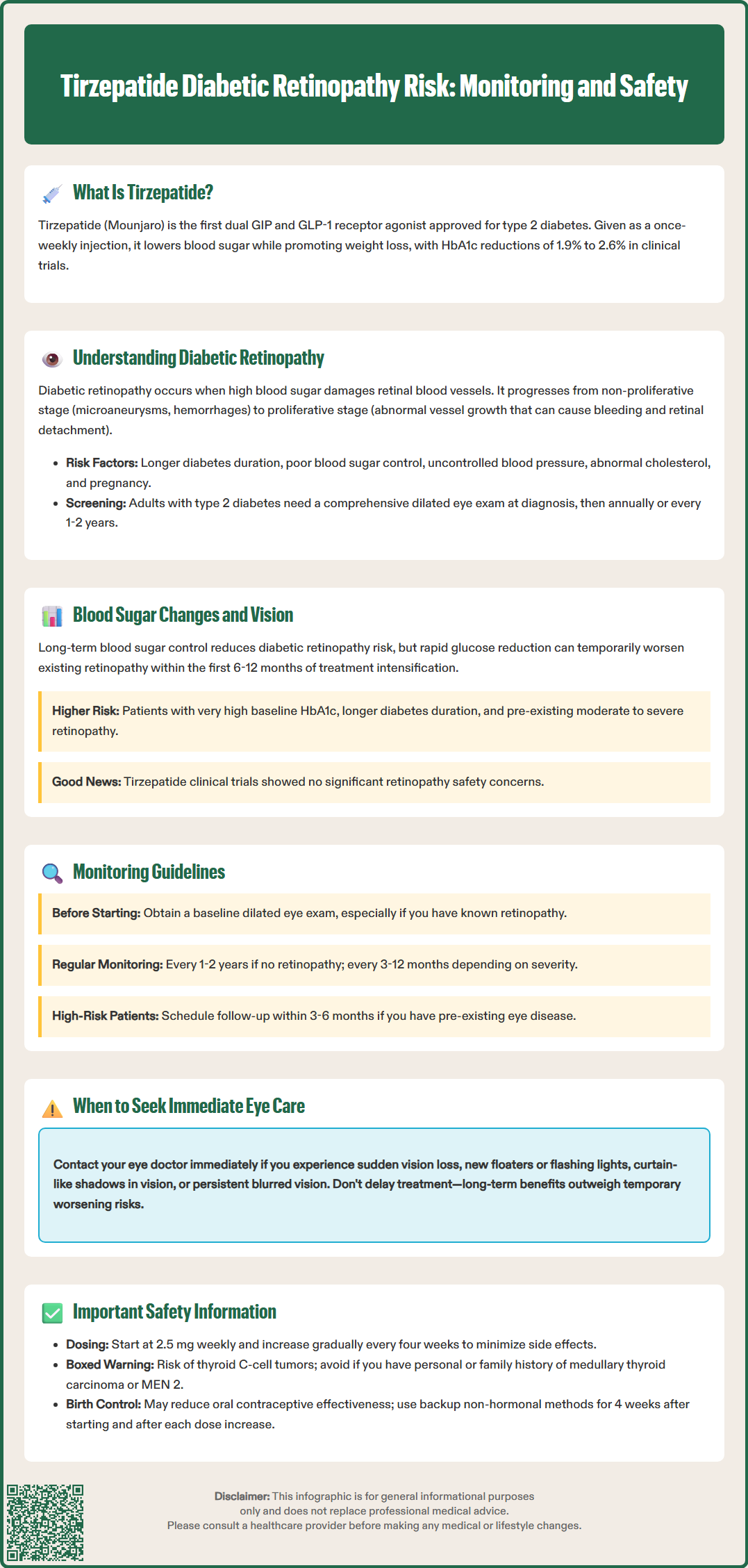
Diabetic retinopathy is a microvascular complication of diabetes that affects the blood vessels of the retina and represents a leading cause of new cases of vision loss among working-age adults in the United States. The condition develops when chronically elevated blood glucose levels damage the small blood vessels in the retina, leading to vascular leakage, ischemia, and potentially vision-threatening complications.
Diabetic retinopathy progresses through distinct stages. Non-proliferative diabetic retinopathy (NPDR) is characterized by microaneurysms, retinal hemorrhages, hard exudates, and cotton-wool spots. As the disease advances to proliferative diabetic retinopathy (PDR), abnormal new blood vessels grow on the retinal surface in response to ischemia. These fragile vessels can bleed into the vitreous cavity, causing sudden vision loss, and may lead to tractional retinal detachment. Diabetic macular edema (DME) can occur at any stage and involves fluid accumulation in the macula, the central area responsible for sharp vision.
Several established risk factors increase the likelihood of developing or worsening diabetic retinopathy:
Duration of diabetes: Longer disease duration significantly increases risk
Poor glycemic control: Elevated HbA1c levels accelerate retinopathy progression
Hypertension: Uncontrolled blood pressure compounds vascular damage
Dyslipidemia: Abnormal lipid levels contribute to retinal exudates
Pregnancy: Gestational changes can accelerate retinopathy
Rapid glycemic improvement: Paradoxically, very rapid reduction in blood glucose can temporarily worsen retinopathy
The American Diabetes Association recommends that adults with type 2 diabetes receive a comprehensive dilated eye examination at the time of diagnosis. Thereafter, exams should be performed annually, or every 1-2 years if there is no evidence of retinopathy and glucose control is good. For women with preexisting diabetes who become pregnant, an eye examination is recommended in the first trimester with close follow-up throughout pregnancy and postpartum. Validated retinal photography with remote interpretation by experts may serve as a screening tool where appropriate. Early detection through regular screening enables timely intervention with laser photocoagulation, intravitreal anti-VEGF injections, or vitrectomy surgery when indicated.
The relationship between glucose-lowering therapy and diabetic retinopathy is complex and requires careful clinical consideration. While long-term glycemic control unequivocally reduces the risk of developing and progressing diabetic retinopathy (as demonstrated in the DCCT and UKPDS trials), rapid reduction in blood glucose levels can paradoxically cause temporary worsening of existing retinopathy—a phenomenon termed "early worsening" or "acute progression."
This phenomenon was first documented in the Diabetes Control and Complications Trial (DCCT) and has been observed with intensive insulin therapy and other glucose-lowering interventions. The proposed mechanism involves rapid normalization of blood glucose leading to altered retinal blood flow, increased vascular permeability, and accelerated progression of pre-existing retinal changes. This early worsening typically occurs within the first 6 to 12 months of treatment intensification and is more likely in patients with poor baseline glycemic control (very high HbA1c), longer diabetes duration, and pre-existing moderate to severe retinopathy.
With tirzepatide specifically, the SURPASS clinical trial program, which evaluated tirzepatide across multiple studies, did not identify retinopathy as a significant safety concern compared to placebo or active comparators. However, it is important to note that these trials generally excluded patients with unstable or rapidly progressing retinopathy, and the observation periods may not have been sufficient to detect rare events.
Practical strategies to minimize retinopathy risk during treatment initiation include:
Gradual dose escalation following FDA-approved titration schedules
Baseline ophthalmologic assessment before starting therapy in patients with known retinopathy
More frequent monitoring during the first year of treatment in high-risk patients
Coordinated care between endocrinology and ophthalmology specialists
Patient education about vision changes requiring urgent evaluation
Consider proactive reduction in insulin or sulfonylurea doses to reduce hypoglycemia risk during treatment intensification
Patients should be counseled that while effective glucose control is essential for long-term eye health, any sudden vision changes—including blurred vision, floaters, flashing lights, or vision loss—warrant immediate ophthalmologic evaluation regardless of recent medication changes. Treatment intensification should generally proceed with appropriate eye monitoring rather than be delayed, as the long-term benefits of improved glycemic control substantially outweigh the risk of early worsening in most patients.
Comprehensive eye care monitoring is essential for all patients with diabetes, and this remains true for those initiating tirzepatide therapy. While there is no official link establishing tirzepatide as a direct cause of diabetic retinopathy, prudent clinical practice dictates systematic ophthalmologic surveillance, particularly given the medication's potent glucose-lowering effects.
The American Diabetes Association and American Academy of Ophthalmology recommend that adults with type 2 diabetes undergo a comprehensive dilated eye examination performed by an ophthalmologist or optometrist at the time of diabetes diagnosis. For patients with no evidence of retinopathy and good glycemic control, screening every 1-2 years may be sufficient. However, patients with any degree of diabetic retinopathy require more frequent examinations based on severity—typically every 6 to 12 months for mild NPDR, every 3 to 6 months for moderate NPDR, and every 3 to 4 months for severe NPDR, while PDR requires follow-up as directed by a retina specialist.
For patients initiating tirzepatide, the following monitoring approach is recommended:
Obtain baseline dilated eye examination before starting therapy, particularly in patients with known retinopathy
Schedule follow-up ophthalmologic evaluation within 3 to 6 months of treatment initiation for patients with pre-existing retinopathy
Maintain appropriate screening intervals (annual or every 1-2 years) for patients without baseline retinopathy based on glycemic control
For pregnant women with preexisting diabetes, obtain an eye examination in the first trimester with close follow-up throughout pregnancy
Coordinate care between primary care, endocrinology, and ophthalmology providers
Patients should be instructed to seek immediate ophthalmologic evaluation (same-day or next-day) if they experience:
Sudden vision loss or significant vision changes
New floaters or flashing lights
Curtain-like shadow across the visual field
Persistent blurred vision not explained by refractive changes
Healthcare providers should document baseline retinopathy status, communicate treatment plans with eye care specialists, and maintain awareness that optimal long-term glycemic control—achieved through medications like tirzepatide—remains the most effective strategy for preventing vision-threatening diabetic eye disease. The benefits of improved glucose control substantially outweigh theoretical concerns about early worsening in the vast majority of patients, provided appropriate monitoring is in place.
Clinical trials have not identified tirzepatide as a direct cause of diabetic retinopathy. However, rapid glucose reduction with any diabetes medication can temporarily worsen pre-existing retinopathy in susceptible patients, particularly those with poor baseline control or moderate-to-severe retinopathy at treatment initiation.
Patients without retinopathy should have dilated eye exams annually or every 1-2 years based on glycemic control. Those with pre-existing retinopathy should obtain a baseline examination before starting tirzepatide and follow-up within 3-6 months, with subsequent monitoring intervals determined by retinopathy severity and ophthalmologist recommendations.
Seek same-day or next-day ophthalmologic evaluation for sudden vision loss, new floaters or flashing lights, curtain-like shadows across your visual field, or persistent blurred vision not explained by refractive changes. These symptoms may indicate serious retinal complications requiring urgent intervention.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.