LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

When do you see results from GLP-1 medications? This is one of the most common questions patients ask when starting these therapies for type 2 diabetes or weight management. GLP-1 receptor agonists like semaglutide (Wegovy), tirzepatide (Zepbound), and liraglutide (Saxenda) work through multiple mechanisms to improve blood sugar control and promote weight loss. Results appear at different rates depending on what you're measuring—blood glucose improvements often begin within days to weeks, while noticeable weight loss typically emerges after 4–6 weeks. Understanding the expected timeline helps set realistic expectations and supports long-term adherence to therapy.
Quick Answer: Most patients see blood glucose improvements within 1–4 weeks of starting GLP-1 therapy, while noticeable weight loss typically becomes apparent after 4–6 weeks, with peak effects at 60–72 weeks.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management. Some are now FDA-approved for chronic weight management, including semaglutide 2.4 mg (Wegovy), tirzepatide (Zepbound), and liraglutide 3 mg (Saxenda). Tirzepatide (Mounjaro, Zepbound) is actually a dual GIP/GLP-1 receptor agonist. Other agents like dulaglutide (Trulicity) and liraglutide at lower doses (Victoza) are approved only for diabetes treatment. These medications work by mimicking the action of naturally occurring GLP-1, an incretin hormone released by the intestine in response to food intake.
The mechanism of action involves multiple physiological pathways that contribute to both glycemic control and weight reduction. GLP-1 receptor agonists enhance glucose-dependent insulin secretion from pancreatic beta cells, suppress inappropriate glucagon release from alpha cells, and slow gastric emptying. These effects collectively improve postprandial glucose excursions and reduce fasting blood glucose levels in patients with type 2 diabetes.
Beyond glycemic effects, GLP-1 medications act on appetite regulation centers in the hypothalamus, promoting satiety and reducing hunger signals. The delayed gastric emptying contributes to prolonged feelings of fullness after meals. Additionally, these agents may influence food reward pathways in the brain, potentially reducing cravings for high-calorie foods.
Understanding this multifaceted mechanism helps explain why results appear at different rates for different outcomes. Glycemic improvements often precede significant weight changes, and individual responses vary based on baseline metabolic status, dosing regimen, and adherence to lifestyle modifications.
Importantly, these medications carry a boxed warning for risk of thyroid C-cell tumors and are contraindicated in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). They are not indicated for type 1 diabetes or diabetic ketoacidosis.
The timeline for seeing results from GLP-1 medications varies depending on the specific outcome being measured and the individual patient. For glycemic control in type 2 diabetes, improvements in blood glucose levels typically begin within the first week of treatment, with fasting glucose reductions often noticeable within 2–4 weeks. Hemoglobin A1c (HbA1c) reductions, which reflect average glucose control over the preceding 2–3 months, become measurable at 12–16 weeks, with maximal effects generally achieved by 6 months of therapy. The American Diabetes Association recommends reassessing A1c approximately every 3 months during therapy changes.
Weight loss follows a more gradual trajectory. Most patients begin noticing appetite suppression and reduced hunger within the first 1–2 weeks of starting GLP-1 therapy. However, measurable weight loss on the scale typically becomes apparent after 4–6 weeks of treatment. Weight loss results vary significantly by specific medication and dose:
Semaglutide 2.4 mg (Wegovy): Clinical trials (STEP program) showed average weight reductions of 15–17% at 68 weeks
Tirzepatide (Zepbound): SURMOUNT trials demonstrated weight reductions of 15–22% at 72 weeks, with results varying between populations with and without diabetes
Liraglutide 3 mg (Saxenda): Typically produces 5–10% weight loss over 56 weeks
The rate of weight loss is not linear. Initial weight loss tends to be more rapid during the first 3–4 months, followed by a slower but continued decline. Peak weight loss effects are generally observed between 60–72 weeks of continuous treatment.
It is important to note that individual responses vary considerably. Some patients experience noticeable appetite suppression and early weight loss within weeks, while others require several months to see significant changes. Patients with diabetes should be aware that rapid improvement in blood glucose can temporarily worsen diabetic retinopathy in those with pre-existing retinopathy, necessitating appropriate eye care follow-up.
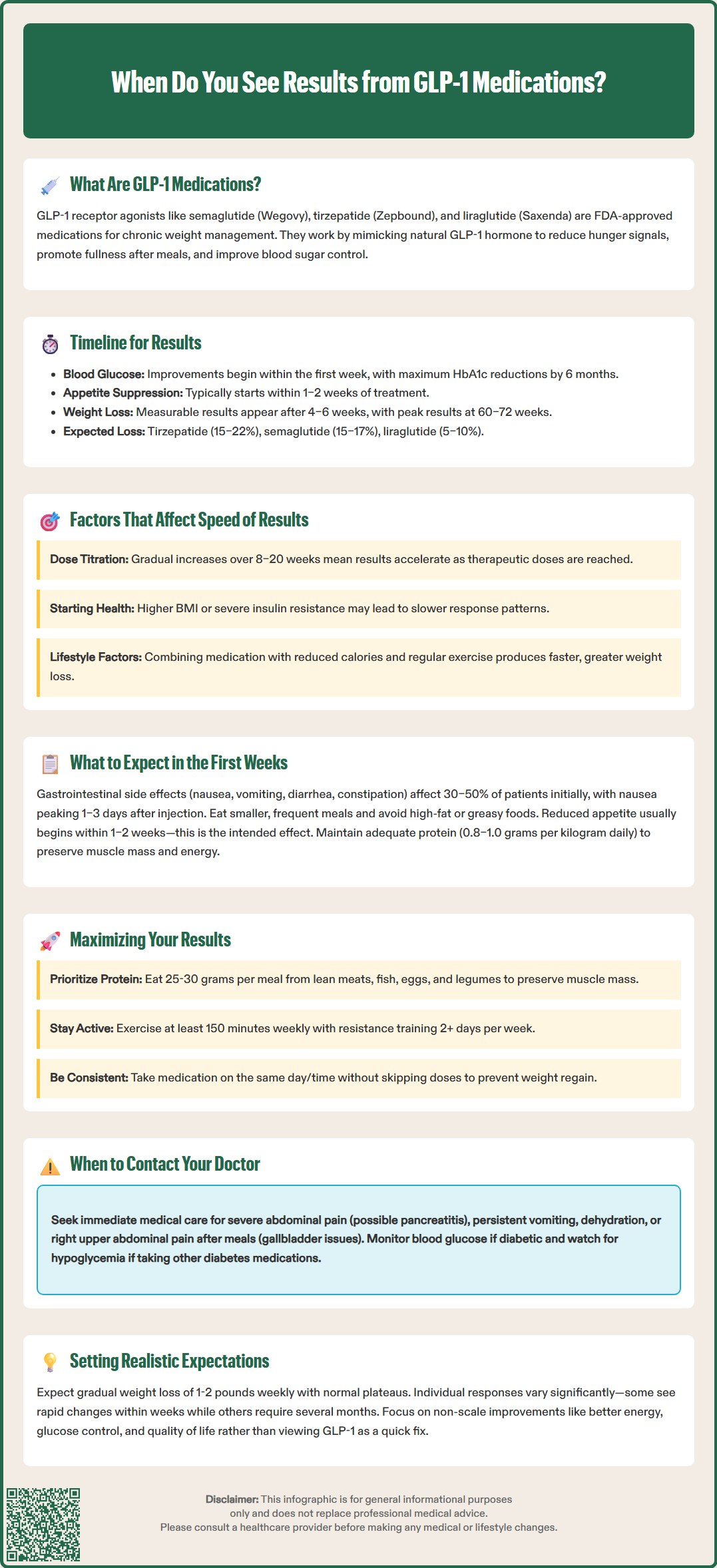
Multiple factors influence the speed and magnitude of response to GLP-1 medications. Dosing and titration schedule play a critical role. Most GLP-1 agents require gradual dose escalation to minimize gastrointestinal side effects, meaning patients start at lower-than-maintenance titration doses and increase incrementally over 8–20 weeks depending on the specific medication. Results accelerate as therapeutic doses are reached.
Baseline metabolic status significantly impacts response rates. Patients with higher baseline body mass index (BMI) or more severe insulin resistance may experience different response patterns compared to those with lower BMI or better preserved metabolic function. Similarly, individuals with longer duration of type 2 diabetes or more advanced beta-cell dysfunction may see slower glycemic improvements.
Adherence to lifestyle modifications substantially affects outcomes. GLP-1 medications work synergistically with dietary changes and physical activity. Patients who combine pharmacotherapy with reduced caloric intake and regular exercise typically achieve faster and more substantial weight loss compared to those relying on medication alone. The American Diabetes Association emphasizes that GLP-1 therapy should be integrated into comprehensive lifestyle management.
Medication-specific pharmacokinetics also matter. Once-weekly formulations like semaglutide reach steady-state concentrations after approximately 4–5 weeks, while dulaglutide typically reaches steady state in 2–4 weeks. Daily formulations like liraglutide achieve steady state more quickly. Tirzepatide, with its dual GIP/GLP-1 receptor mechanism, may produce more rapid weight loss in some patients.
Concurrent medications can significantly impact results. Insulin or sulfonylureas may increase hypoglycemia risk when combined with GLP-1 agents, often requiring dose adjustments. Some medications, such as certain antipsychotics or corticosteroids, may counteract weight loss effects. For women taking tirzepatide, reduced absorption of oral contraceptives during initiation and dose escalation may necessitate additional contraceptive methods for 4 weeks after dose changes.
The initial weeks of GLP-1 therapy represent an adjustment period as your body adapts to the medication. Gastrointestinal side effects are the most common early experiences, affecting 30–50% of patients to varying degrees. These typically include nausea, occasional vomiting, diarrhea, constipation, and abdominal discomfort. Nausea is usually most pronounced 1–3 days after injection and tends to improve over subsequent days, often diminishing significantly after 4–8 weeks as tolerance develops.
To minimize gastrointestinal symptoms, eat smaller, more frequent meals rather than large portions. Avoid high-fat, greasy, or heavily spiced foods initially. Stay well-hydrated, and consider eating slowly to allow your delayed gastric emptying to signal fullness appropriately. Maintaining adequate hydration is crucial, as severe vomiting or diarrhea can lead to dehydration and potential kidney problems.
Appetite changes often begin within the first 1–2 weeks. Many patients report feeling satisfied with smaller portions and experiencing reduced food cravings, particularly for sweets and high-calorie foods. Some describe a subtle but persistent feeling of fullness or lack of interest in eating. This is the intended therapeutic effect, but it can feel unusual initially. Listen to your body's satiety signals and avoid forcing yourself to eat if you're genuinely not hungry, while ensuring adequate nutrition and hydration.
Energy levels may fluctuate during the first month. Some patients report mild fatigue, which may relate to reduced caloric intake, adjustment to the medication, or changes in eating patterns. Others feel energized by early improvements in blood glucose stability. Maintaining adequate protein intake (0.8–1.0 grams per kilogram of body weight daily) helps preserve lean muscle mass and energy levels.
Monitoring and follow-up are essential during this initiation phase. Track your blood glucose if you have diabetes, watch for signs of hypoglycemia if you're taking other glucose-lowering medications, and report any severe or concerning symptoms to your healthcare provider. Seek immediate medical attention for severe abdominal pain (especially if radiating to the back, which may indicate pancreatitis), persistent vomiting, signs of dehydration, or symptoms of gallbladder problems (pain in the right upper abdomen, especially after meals).
Optimizing outcomes with GLP-1 medications requires a comprehensive approach that extends beyond simply taking the medication. Dietary strategies should focus on nutrient-dense, high-protein foods to maintain lean muscle mass during weight loss. Aim for 25–30 grams of protein per meal, emphasizing lean meats, fish, eggs, legumes, and low-fat dairy. Prioritize vegetables, whole grains, and healthy fats while limiting ultra-processed foods and added sugars. The reduced appetite from GLP-1 therapy makes it easier to adhere to these dietary patterns, but intentional meal planning ensures adequate nutrition. Consider consulting a registered dietitian for personalized guidance, especially if you have kidney disease or other conditions requiring dietary modifications.
Physical activity enhances both weight loss and metabolic improvements. The U.S. Department of Health and Human Services recommends 150–300 minutes of moderate-intensity aerobic activity weekly, plus muscle-strengthening activities on 2 or more days per week. The American Diabetes Association similarly recommends at least 150 minutes of moderate-intensity exercise weekly, spread over at least 3 days, with no more than 2 consecutive days without activity. Resistance exercise is particularly important during weight loss to preserve muscle mass and maintain metabolic rate. Even modest increases in daily movement—such as walking 7,000–10,000 steps daily—contribute meaningfully to outcomes.
Medication adherence is critical for sustained results. Take your GLP-1 medication on the same day each week (for weekly formulations) or at the same time daily (for daily formulations). Do not skip doses or discontinue therapy without medical guidance, as weight regain commonly occurs after stopping GLP-1 medications. Clinical trials show that patients typically regain significant weight after discontinuation. If you miss a dose, follow the specific instructions provided with your medication, which vary by agent.
Regular monitoring helps track progress and identify any concerns early. Schedule follow-up appointments as recommended by your healthcare provider, typically every 3–6 months once stable. Monitor for potential adverse effects including persistent gastrointestinal symptoms, signs of pancreatitis (severe abdominal pain radiating to the back), gallbladder disease (right upper quadrant pain, especially after meals), or changes in mood. Women taking tirzepatide should be aware that it may reduce the effectiveness of oral contraceptives during dose initiation and escalation; additional contraceptive methods are recommended for 4 weeks after starting or increasing doses.
Realistic expectations support long-term success. GLP-1 therapy is a tool for chronic disease management, not a quick fix. Weight loss of 1–2 pounds per week is appropriate and sustainable. Plateaus are normal and do not indicate treatment failure. Focus on non-scale victories such as improved energy, better glucose control, reduced medication burden, and enhanced quality of life. If results plateau despite adherence, discuss dose optimization or adjunctive strategies with your healthcare provider.
Blood glucose improvements typically begin within the first week of GLP-1 therapy, with fasting glucose reductions noticeable within 2–4 weeks. Hemoglobin A1c reductions become measurable at 12–16 weeks, with maximal effects generally achieved by 6 months.
Gastrointestinal side effects including nausea, vomiting, diarrhea, and constipation affect 30–50% of patients during the first weeks. These symptoms are usually most pronounced 1–3 days after injection and typically diminish significantly after 4–8 weeks as tolerance develops.
Yes, clinical trials show that patients typically regain significant weight after discontinuing GLP-1 medications. These agents are intended for chronic disease management, and sustained results require ongoing therapy combined with lifestyle modifications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.