LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients taking GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) report feeling unusually cold during treatment. While not listed as an official side effect in FDA labeling, this sensation is a common physiological response to the significant weight loss these medications produce. As your body composition changes—particularly with loss of insulating adipose tissue and reduced caloric intake—your ability to generate and retain heat is affected. Understanding why this happens and when it warrants medical attention can help you manage this temporary but uncomfortable experience while continuing your treatment safely.
Quick Answer: Feeling cold on GLP-1 medications results from physiological changes during weight loss, including reduced insulating fat tissue, decreased caloric intake lowering heat production, and metabolic adaptations that make the body more energy-efficient.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Feeling cold while taking GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound)—the latter being a dual GIP/GLP-1 receptor agonist—is something many patients report anecdotally, though it is not listed as an official adverse effect in FDA-approved labeling for these medications. This sensation typically relates to the physiological changes that occur during significant weight loss rather than a direct pharmacological effect of the medication itself.
These incretin-based medications work by mimicking naturally occurring hormones that enhance insulin secretion, suppress glucagon release, slow gastric emptying, and reduce appetite through central nervous system pathways. These mechanisms lead to reduced caloric intake and subsequent weight loss in most patients. As body composition changes—particularly with loss of adipose tissue—thermoregulation is affected because fat serves primarily as insulation, while heat generation comes largely from metabolically active lean tissue.
Additionally, the caloric deficit created by reduced food intake means less energy is available for thermogenesis, the process by which the body produces heat. Patients may notice increased cold sensitivity in their extremities, a general feeling of being chilly even in comfortable environments, or difficulty staying warm compared to before starting treatment. For patients also taking insulin or sulfonylureas, it's important to check blood glucose levels when feeling cold, as hypoglycemia can present with cold, clammy sensations. While uncomfortable, increased cold sensitivity is generally a physiological adaptation to weight loss rather than a concerning adverse reaction.
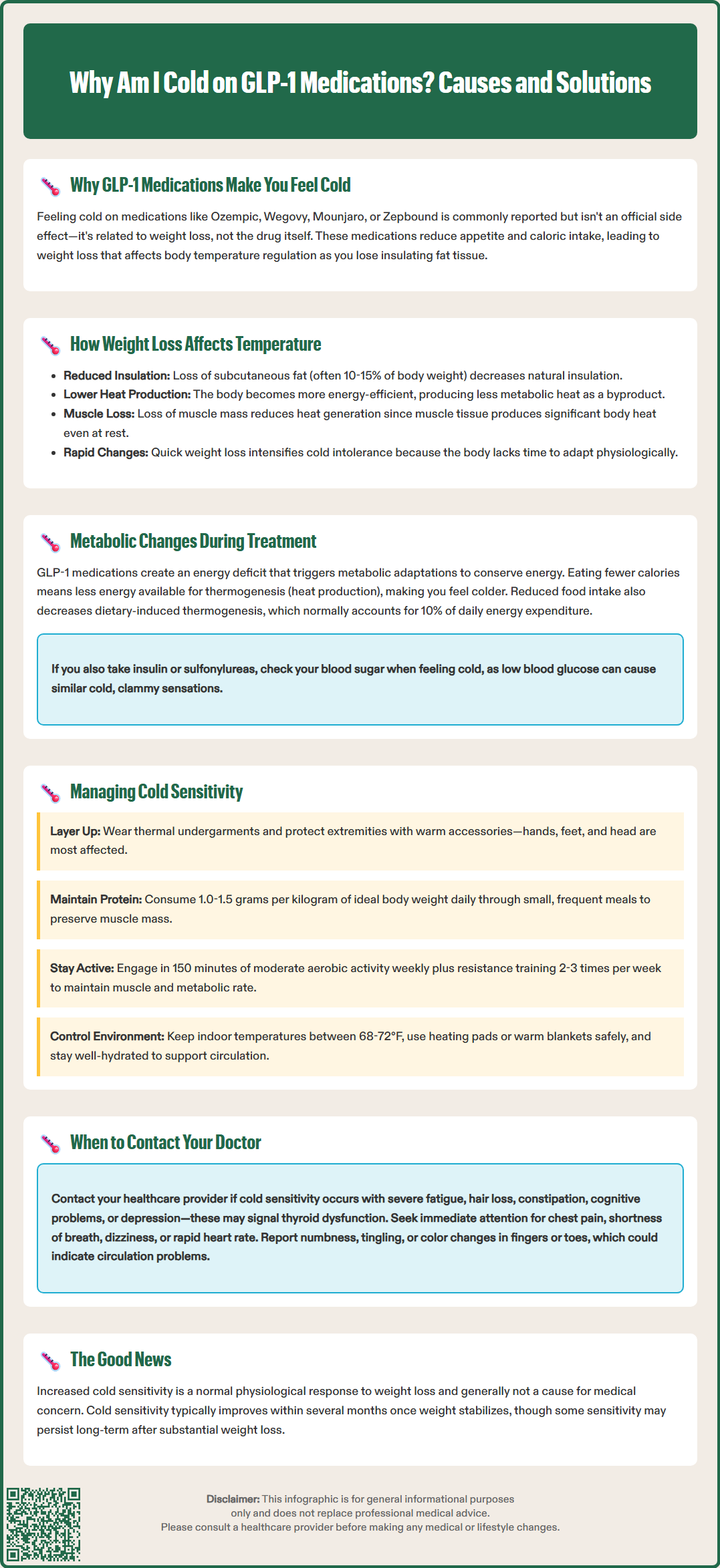
Weight loss, regardless of the method achieved, fundamentally alters how the body regulates temperature. Adipose tissue functions as both insulation and an endocrine organ that influences metabolic rate. When patients lose significant weight on incretin-based therapies—often 10-15% or more of initial body weight in clinical trials such as the STEP program (semaglutide) and SURMOUNT trials (tirzepatide)—the reduction in subcutaneous fat decreases the body's natural insulation layer, making environmental temperatures feel colder than before.
Beyond insulation, the body's total energy expenditure typically declines with weight loss, which includes a reduction in heat production as a metabolic byproduct. Research on adaptive thermogenesis shows that individuals who lose substantial weight experience metabolic adaptations where the body becomes more energy-efficient and generates less heat relative to body size. This adaptation, while energy-conserving, manifests as increased cold sensitivity.
The rate of weight loss may also influence the degree of cold intolerance, though this observation is primarily based on clinical experience rather than controlled studies. Rapid weight reduction—common in the first months of treatment with these medications—may not allow sufficient time for physiological adaptation. Furthermore, loss of lean muscle mass, which can occur alongside fat loss if protein intake and resistance exercise are inadequate, further reduces metabolic heat production since muscle tissue is metabolically active and generates significant body heat even at rest.
These thermoregulatory changes are typically temporary and may improve as weight stabilizes and the body adapts to its new composition. However, some degree of increased cold sensitivity may persist, particularly in individuals who achieve substantial weight loss.
Incretin-based medications induce several metabolic changes beyond weight loss that may contribute to altered temperature perception. The medications' effect on gastric emptying and reduced caloric intake creates a sustained energy deficit, which triggers metabolic adaptations aimed at conserving energy. With significant caloric restriction, studies show the body may reduce conversion of thyroid hormone T4 to the more active T3 form and alter sympathetic nervous system activity, both of which can influence heat production.
The reduction in food intake means less dietary-induced thermogenesis, the heat generated during digestion and nutrient processing. This thermic effect of food typically accounts for approximately 10% of total daily energy expenditure according to NIDDK resources. With smaller meal sizes and potentially reduced meal frequency, this heat-generating process is diminished, potentially contributing to overall cold sensation.
Some patients may also experience changes in blood glucose regulation that could affect temperature perception. While GLP-1 medications improve glycemic control in patients with type 2 diabetes, lower blood glucose levels—particularly if they drop too quickly—can sometimes be associated with feeling cold. This is especially relevant for patients also taking insulin or sulfonylureas, who should monitor for hypoglycemia symptoms.
It is important to note that these metabolic adaptations are generally physiological responses to weight loss rather than pathological changes. However, clinicians should remain vigilant for signs of excessive metabolic suppression or thyroid dysfunction, particularly in patients with pre-existing thyroid conditions or those experiencing symptoms beyond cold intolerance, such as severe fatigue, hair loss, or cognitive changes that might suggest thyroid hormone imbalance requiring investigation.
While mild cold sensitivity is a common and generally benign experience during treatment with incretin-based medications, certain symptoms warrant medical evaluation to rule out underlying conditions or complications. Patients should contact their healthcare provider if cold intolerance is accompanied by severe fatigue, hair thinning or loss, persistent constipation, cognitive impairment, or depression, as these may indicate thyroid dysfunction requiring laboratory assessment.
Thyroid function testing, including thyroid-stimulating hormone (TSH) and free thyroxine (T4) levels, should be considered if cold intolerance is severe or accompanied by other hypothyroid symptoms. While these medications do not directly cause hypothyroidism, significant weight loss can sometimes unmask subclinical thyroid disease or necessitate adjustment of thyroid hormone replacement in patients with pre-existing hypothyroidism.
Patients should also seek evaluation if they experience numbness, tingling, or color changes in fingers and toes (particularly white, blue, or red discoloration), which could indicate peripheral vascular issues or Raynaud's phenomenon rather than simple cold sensitivity. Additionally, if cold intolerance is accompanied by chest pain, shortness of breath, dizziness, or rapid heart rate, immediate medical attention is warranted to exclude cardiovascular complications.
Other reasons to contact your provider include:
Weight loss that significantly exceeds your prescribed treatment plan
Cold sensations accompanied by sweating, tremor, or confusion (possible hypoglycemia, especially if taking insulin or sulfonylureas)
Persistent fatigue with pallor or weakness (possible anemia)
Severe or persistent symptoms that significantly impact quality of life or do not improve with conservative measures
Your healthcare provider can assess whether symptoms represent expected physiological adaptation, require investigation for alternative causes (including blood tests for thyroid function, complete blood count, iron studies, or vitamin B12 levels), or indicate a need for medication adjustment.
Several practical strategies can help patients manage cold sensitivity while continuing incretin-based therapy. Layered clothing is the most effective immediate intervention, allowing adjustment to varying environmental temperatures throughout the day. Focus on insulating core body temperature with thermal undergarments, and protect extremities with warm socks, gloves, and hats, as these areas are most susceptible to cold sensation due to peripheral vasoconstriction.
Maintaining adequate nutrition despite reduced appetite is crucial for supporting metabolic heat production. Patients should prioritize protein intake (1.0-1.5 grams per kilogram of ideal body weight daily) to preserve lean muscle mass during weight loss, which helps maintain metabolic rate and heat generation. Consulting with a registered dietitian can provide personalized nutrition guidance. Consuming warm beverages and foods can provide temporary comfort and contribute to overall caloric intake. Small, frequent meals may be better tolerated than larger portions given the gastric effects of these medications.
Regular physical activity, particularly resistance training, helps maintain muscle mass and metabolic rate, both of which support heat production. The U.S. Department of Health and Human Services Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, plus muscle-strengthening activities 2-3 days per week for overall health and weight management.
Environmental modifications include maintaining comfortable indoor temperatures (68-72°F), using heating pads or warm blankets, and taking warm baths or showers. When using heating devices, avoid prolonged application, never sleep with heating pads, and use caution if you have reduced sensation or neuropathy to prevent burns. Staying well-hydrated supports circulation and metabolic function. Patients should avoid extreme temperature changes when possible and be particularly cautious in cold weather, as reduced cold tolerance may increase risk of hypothermia during prolonged exposure.
If conservative measures are insufficient and cold intolerance significantly impacts quality of life, discuss with your healthcare provider whether medication adjustment, additional metabolic assessment, or consultation with an endocrinologist might be beneficial. In most cases, symptoms improve as weight stabilizes and the body adapts to its new metabolic state, typically within several months of reaching a stable weight.
Mild cold sensitivity is generally a benign physiological response to weight loss rather than a dangerous side effect. However, contact your healthcare provider if cold intolerance is accompanied by severe fatigue, hair loss, cognitive changes, or other symptoms that might indicate thyroid dysfunction or other medical conditions requiring evaluation.
Cold sensitivity typically improves as your weight stabilizes and your body adapts to its new metabolic state, usually within several months of reaching a stable weight. Some degree of increased cold sensitivity may persist in individuals who achieve substantial weight loss due to reduced insulating adipose tissue.
Yes, practical strategies include wearing layered clothing, maintaining adequate protein intake (1.0-1.5 grams per kilogram of ideal body weight daily) to preserve muscle mass, engaging in regular resistance training, consuming warm beverages and foods, and maintaining comfortable indoor temperatures. These measures support metabolic heat production and provide immediate comfort.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.