LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) effectively manage type 2 diabetes and promote weight loss, but their gastrointestinal effects—including nausea, vomiting, and diarrhea—can disrupt fluid and electrolyte balance. These medications slow gastric emptying and suppress appetite, which may reduce oral intake while increasing losses of sodium, potassium, magnesium, and other essential minerals. Understanding why electrolytes are important on GLP-1 therapy helps patients and clinicians prevent complications ranging from muscle weakness to cardiac arrhythmias. Proactive hydration, nutritional strategies, and monitoring can maintain electrolyte balance and optimize treatment outcomes.
Quick Answer: Electrolytes are important on GLP-1 medications because gastrointestinal side effects like nausea, vomiting, and diarrhea can cause significant losses of sodium, potassium, and magnesium, while reduced appetite and fluid intake further compromise electrolyte balance.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—work by mimicking the incretin hormone GLP-1. Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist. These medications enhance insulin secretion in response to meals, suppress glucagon release, slow gastric emptying, and reduce appetite through central nervous system pathways. While these mechanisms effectively lower blood glucose and promote weight loss, they also create physiological changes that can impact fluid and electrolyte homeostasis.
The most clinically significant effect on electrolyte balance stems from gastrointestinal adverse effects. These medications commonly cause nausea, vomiting, and diarrhea, particularly during dose initiation and escalation. According to FDA prescribing information, nausea occurs in 15–44% of patients, vomiting affects 5–24%, and diarrhea 8–30%, with rates varying by specific agent and dose. These symptoms result from delayed gastric emptying and direct effects on the gastrointestinal tract.
When patients experience persistent vomiting or diarrhea, they lose not only fluid but also essential electrolytes—primarily sodium, potassium, chloride, and bicarbonate. The slowed gastric emptying may also reduce oral intake, as patients feel fuller longer and may struggle to consume adequate fluids. Additionally, the appetite suppression that contributes to weight loss can inadvertently lead to reduced electrolyte intake if patients significantly decrease their food and beverage consumption.
While GLP-1 medications have modest natriuretic effects in some studies, the primary concern is the secondary effects of reduced intake and increased gastrointestinal losses. FDA labels for these medications include warnings about the risk of dehydration and acute kidney injury, particularly during episodes of significant gastrointestinal illness. This creates a clinically relevant risk for electrolyte disturbances that requires monitoring and patient education.
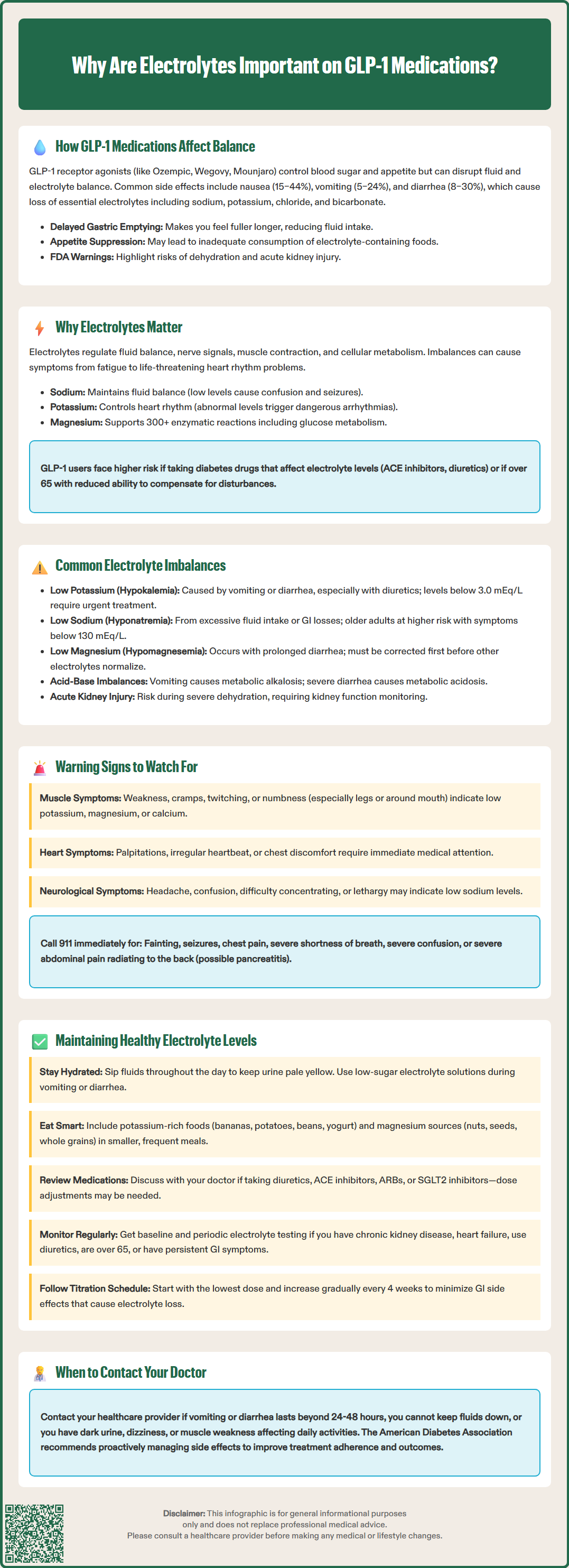
Electrolytes are minerals that carry electrical charges and perform critical functions throughout the body. The major electrolytes—sodium, potassium, chloride, magnesium, calcium, and phosphate—regulate fluid balance, maintain acid-base homeostasis, enable nerve signal transmission, facilitate muscle contraction, and support cellular metabolism. Even modest imbalances can produce symptoms ranging from mild fatigue to life-threatening cardiac arrhythmias.
Sodium maintains extracellular fluid volume and osmotic balance. Hyponatremia (low sodium) can cause confusion, headache, seizures, and in severe cases, cerebral edema. Potassium is essential for cardiac electrical activity and muscle function; both hypokalemia (low potassium) and hyperkalemia (high potassium) can trigger dangerous heart rhythm disturbances. Magnesium supports over 300 enzymatic reactions, including those involved in glucose metabolism and insulin sensitivity—particularly relevant for patients with type 2 diabetes using GLP-1 therapy.
For patients on GLP-1 medications, maintaining electrolyte balance becomes especially important for several reasons. First, many individuals prescribed these agents have type 2 diabetes and may already take medications that affect electrolytes. ACE inhibitors, ARBs, and potassium-sparing diuretics can increase potassium levels, while loop and thiazide diuretics can decrease potassium levels. This combination increases risk. Second, older adults, who represent a significant proportion of GLP-1 users, have reduced physiological reserve and are more vulnerable to electrolyte disturbances.
The American Diabetes Association Standards of Care emphasizes that medication-related adverse effects, including those affecting hydration and electrolytes, should be proactively managed to optimize treatment adherence and outcomes. The Standards also provide sick-day guidance that applies during episodes of dehydration. Electrolyte monitoring is not routinely required for all GLP-1 users, but becomes essential when patients experience persistent gastrointestinal symptoms or have additional risk factors such as chronic kidney disease, heart failure, age over 65, or concurrent diuretic use.
While there is no official direct link between GLP-1 receptor agonists and specific electrolyte disorders, clinical experience and case reports have identified patterns of imbalance associated with the gastrointestinal effects of these medications. Understanding these patterns helps clinicians anticipate and prevent complications.
Hypokalemia (low potassium) can occur when patients experience significant vomiting or diarrhea while on GLP-1 therapy. Gastrointestinal losses are particularly rich in potassium, and inadequate dietary replacement—common when appetite is suppressed—compounds the deficit. Normal serum potassium ranges from 3.5–5.0 mEq/L; levels below 3.0 mEq/L require urgent intervention due to cardiac arrhythmia risk. Patients taking loop or thiazide diuretics face substantially elevated risk.
Hyponatremia (low sodium) can develop through multiple mechanisms: excessive fluid intake relative to sodium (dilutional) or gastrointestinal sodium losses. Symptoms typically emerge when sodium falls below 130 mEq/L and become severe below 125 mEq/L. Older adults are particularly susceptible.
Hypomagnesemia (low magnesium) may occur with prolonged diarrhea or inadequate intake. Magnesium deficiency often coexists with hypokalemia and hypocalcemia, and can be difficult to correct without addressing magnesium first. Normal serum magnesium ranges from 1.7–2.2 mg/dL.
Metabolic alkalosis can result from persistent vomiting, which causes loss of gastric hydrochloric acid and hydrogen ions. This acid-base disturbance often accompanies hypokalemia and hypochloremia (low chloride). Less commonly, metabolic acidosis may develop with severe diarrhea due to bicarbonate losses.
Acute kidney injury (AKI) is a risk highlighted in FDA labels for these medications, particularly during episodes of severe dehydration from gastrointestinal symptoms. Monitoring renal function becomes important when patients experience persistent vomiting or diarrhea.
Patients with pre-existing chronic kidney disease face compounded risk, as impaired renal function limits the body's ability to compensate for electrolyte shifts. The combination of GLP-1 therapy and renal impairment warrants closer monitoring, though these medications are generally considered safe in moderate kidney disease and some agents have shown potential renal protective benefits in clinical trials.
Recognizing electrolyte imbalance early allows for prompt intervention before serious complications develop. Patients starting or escalating GLP-1 medications should be educated about warning signs that warrant medical evaluation.
Neuromuscular symptoms are often the first indicators of electrolyte disturbance. Muscle weakness, cramps, or spasms—particularly in the legs—suggest hypokalemia or hypomagnesemia. Muscle twitching, tingling, or numbness around the mouth and in the extremities may indicate hypocalcemia or hypomagnesemia. Severe weakness that impairs daily activities or causes difficulty standing requires urgent assessment.
Cardiac symptoms represent potentially life-threatening manifestations. Palpitations, irregular heartbeat, or chest discomfort may signal potassium or magnesium abnormalities affecting cardiac conduction. Patients should seek immediate medical attention for these symptoms, as both hypokalemia and hyperkalemia can precipitate ventricular arrhythmias.
Neurological changes often accompany sodium disturbances. Headache, confusion, difficulty concentrating, lethargy, or altered mental status may indicate hyponatremia. Severe hyponatremia can progress to seizures or coma. Older adults may present with falls or subtle cognitive changes that family members notice before the patient does.
Gastrointestinal symptoms themselves serve as risk markers. Persistent nausea lasting beyond the first few weeks of therapy, vomiting more than twice daily, or diarrhea occurring more than three times daily significantly increases electrolyte loss risk. Inability to maintain adequate oral fluid intake due to these symptoms constitutes a medical concern requiring provider contact.
Severe abdominal pain, especially if persistent or radiating to the back, requires immediate medical attention as it may indicate pancreatitis or gallbladder disease—rare but serious complications noted in FDA Medication Guides for these medications.
Kidney-related symptoms such as markedly reduced urine output, dark scant urine, or swelling in the legs may indicate acute kidney injury from dehydration and require urgent evaluation.
General symptoms such as persistent fatigue, dizziness (especially upon standing), excessive thirst, or decreased urine output may reflect dehydration and electrolyte depletion. Patients should monitor urine color; dark yellow or amber urine suggests inadequate hydration.
Clinicians should establish clear thresholds for patient contact. Reasonable triggers include: vomiting or diarrhea persisting beyond 24-48 hours, inability to keep down fluids, symptoms of dehydration, muscle weakness interfering with function, or mental status changes. Emergency symptoms warranting 911/ED evaluation include: syncope, seizures, chest pain, severe shortness of breath, or severe confusion. Patients with diabetes should also monitor blood glucose, as dehydration and illness can affect glycemic control.
Proactive strategies can minimize electrolyte disturbance risk and optimize outcomes for patients on GLP-1 therapy. A comprehensive approach addresses hydration, nutrition, medication management, and monitoring.
Hydration strategies form the foundation of electrolyte maintenance. Patients should aim for adequate fluid intake, individualized based on body size, activity level, and climate. The National Academy of Medicine provides guidance on total water intake, but a practical approach is to drink enough that urine remains pale yellow. The reduced appetite and early satiety from GLP-1 medications can make this challenging. Practical approaches include: sipping fluids throughout the day rather than drinking large volumes at once, choosing beverages with electrolytes when experiencing gastrointestinal symptoms, and setting reminders to drink regularly. Plain water remains appropriate for routine hydration, but low-sugar electrolyte solutions become important during active losses. People with diabetes should be cautious with sugary beverages like coconut water, which can affect blood glucose levels.
Nutritional considerations help maintain electrolyte balance through diet. Potassium-rich foods include bananas, oranges, potatoes, spinach, beans, and yogurt. Sodium needs are typically met through normal diet, though patients with persistent vomiting may benefit from salty broths or crackers. Magnesium sources include nuts, seeds, whole grains, and leafy greens. For patients struggling with reduced appetite, focusing on nutrient-dense foods and eating smaller, more frequent meals can help maintain adequate intake. Registered dietitian consultation may benefit patients with significant dietary challenges or rapid weight loss.
Medication review should occur regularly. Clinicians should assess the continued need for diuretics and consider dose adjustments if electrolyte issues emerge. Patients taking ACE inhibitors, ARBs, or potassium-sparing diuretics require careful potassium monitoring. SGLT2 inhibitors, increasingly used alongside GLP-1 therapy, can affect fluid balance and may require coordination. Antiemetic medications may help control nausea in selected patients with persistent symptoms, though this approach should be individualized.
Monitoring approaches should be individualized based on risk factors. Baseline electrolyte measurement before starting GLP-1 therapy may be appropriate for high-risk patients. Routine monitoring is not necessary for all patients, but should be considered for those with: chronic kidney disease, heart failure, concurrent diuretic use, age over 65, or persistent gastrointestinal symptoms.
Dose titration strategies can minimize gastrointestinal side effects and associated electrolyte risks. Following FDA-approved titration schedules for each specific medication is essential. For example, weekly GLP-1 agents often increase every 4 weeks, while daily liraglutide has weekly increments. Starting with the lowest dose and increasing gradually allows physiological adaptation. Some patients may benefit from slower titration or temporary dose reduction if side effects are problematic.
Patient education empowers individuals to participate in their care. Patients should understand: the importance of maintaining hydration despite reduced appetite, which symptoms warrant medical contact, how to use oral rehydration solutions if needed, and the value of keeping scheduled follow-up appointments. Written materials and teach-back methods ensure comprehension. For patients experiencing persistent issues, temporary treatment interruption may be necessary while electrolytes are corrected and hydration restored, followed by reinitiation at a lower dose with more gradual titration.
The most common electrolyte imbalances associated with GLP-1 therapy are hypokalemia (low potassium), hyponatremia (low sodium), and hypomagnesemia (low magnesium), typically resulting from gastrointestinal losses through vomiting or diarrhea combined with reduced oral intake.
Maintain adequate hydration by sipping fluids throughout the day, consume electrolyte-rich foods like bananas, leafy greens, and yogurt, follow your prescribed dose titration schedule, and contact your healthcare provider if you experience persistent vomiting or diarrhea lasting more than 24-48 hours.
Electrolyte monitoring is recommended if you have chronic kidney disease, heart failure, take diuretics, are over 65 years old, or experience persistent gastrointestinal symptoms. Routine monitoring is not necessary for all patients but should be individualized based on risk factors.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.