LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients taking semaglutide (Ozempic, Wegovy, or Rybelsus) wonder whether they can safely take antibiotics while on this medication. The good news is that antibiotics and semaglutide can generally be used together without direct drug interactions. Semaglutide is a GLP-1 receptor agonist used for type 2 diabetes management and weight loss, and no antibiotics are contraindicated in its FDA prescribing information. However, both medication classes can cause gastrointestinal side effects, and semaglutide's effect on gastric emptying may require timing considerations for oral medications. Understanding how to manage these medications together ensures safe, effective treatment when infections arise.
Quick Answer: You can generally take antibiotics while on semaglutide, as there are no known direct drug interactions between semaglutide and commonly prescribed antibiotics.
Yes, you can generally take antibiotics while on semaglutide. There are no known direct drug interactions between semaglutide and commonly prescribed antibiotics that would make their concurrent use unsafe. Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is a glucagon-like peptide-1 (GLP-1) receptor agonist used for type 2 diabetes management and weight loss. No antibiotics are contraindicated in the FDA prescribing information for semaglutide products, and routine dose adjustments are not generally required.
However, the combination may present practical considerations rather than pharmacological contraindications. Both medication classes can cause gastrointestinal side effects, and taking them together might intensify symptoms such as nausea, vomiting, or diarrhea. Additionally, semaglutide slows gastric emptying, which theoretically could affect the absorption timing of oral medications, though this has not been shown to significantly impact antibiotic effectiveness in clinical practice.
While the FDA prescribing information does not specifically address antibiotics with semaglutide, no clinically meaningful interactions have been identified to date. Individual patient factors—including the severity of infection, diabetes control, hydration status, and tolerance to gastrointestinal side effects—should guide clinical decision-making. If you develop severe vomiting or dehydration while taking both medications, contact your healthcare provider promptly, as they may recommend temporarily pausing semaglutide until you recover. Patients should always inform their healthcare providers about all medications they are taking, including semaglutide, before starting antibiotic therapy to ensure comprehensive care and monitoring.
Semaglutide is a long-acting GLP-1 receptor agonist that mimics the action of the naturally occurring incretin hormone GLP-1. Its mechanism of action includes stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. These combined effects result in improved glycemic control in patients with type 2 diabetes and significant weight loss in both diabetic and non-diabetic individuals.
The most clinically relevant pharmacological property affecting potential drug interactions is semaglutide's effect on gastric emptying. By delaying the rate at which food and medications leave the stomach, semaglutide can theoretically alter the absorption profile of orally administered drugs. Injectable semaglutide (Ozempic, Wegovy) has not shown clinically meaningful effects on the absorption of tested oral medications. However, oral semaglutide (Rybelsus) can increase exposure to levothyroxine, requiring appropriate monitoring and timing.
Semaglutide is metabolized through proteolytic degradation, similar to endogenous proteins, and does not rely on cytochrome P450 enzyme systems for elimination. This metabolic pathway means semaglutide does not compete with the vast majority of medications—including antibiotics—that are processed through hepatic enzyme systems, reducing the potential for metabolic drug interactions.
The primary drug interaction concern with semaglutide involves medications that require rapid absorption for effectiveness or those with narrow therapeutic windows. The FDA labeling notes that semaglutide may affect the absorption of oral medications, though specific studies with antibiotics are limited. No specific antibiotics are contraindicated for concurrent use with semaglutide in the FDA prescribing information.
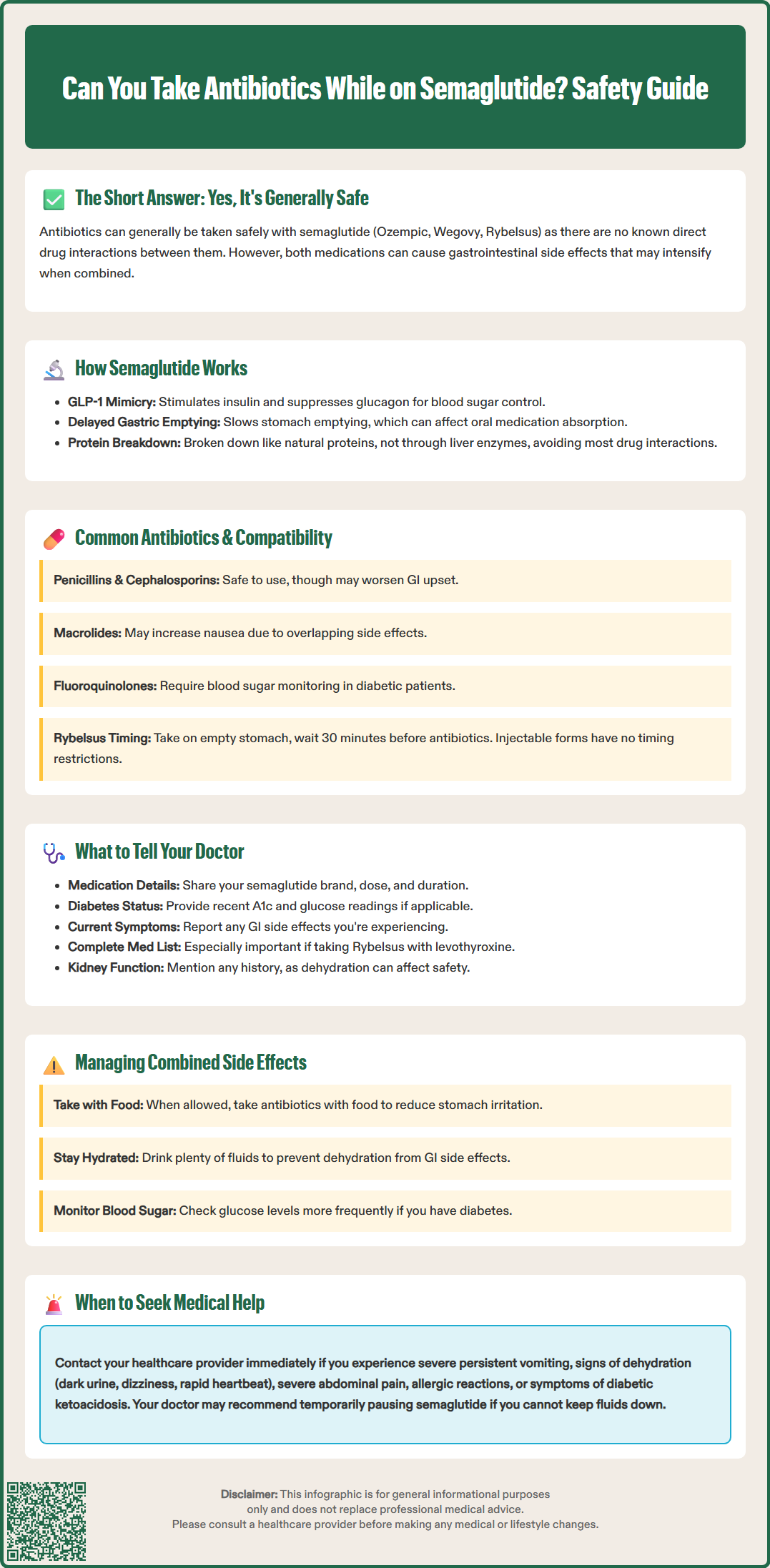
The most frequently prescribed antibiotic classes in the United States—including penicillins (amoxicillin, amoxicillin-clavulanate), cephalosporins (cephalexin, ceftriaxone), macrolides (azithromycin, clarithromycin), fluoroquinolones (ciprofloxacin, levofloxacin), and tetracyclines (doxycycline)—have no documented pharmacological interactions with semaglutide. These antibiotics can generally be prescribed to patients taking semaglutide without routine interaction-based dose adjustments, though dose adjustments may still be needed for patient-specific factors.
Penicillins and cephalosporins, which are among the most commonly used antibiotics for respiratory and skin infections, have well-established safety profiles when used with semaglutide. Their absorption is generally not significantly affected by delayed gastric emptying, and they do not share metabolic pathways with semaglutide. However, both antibiotic classes can cause gastrointestinal upset, which may be additive with semaglutide's GI side effects.
Macrolide antibiotics like azithromycin may increase the likelihood of nausea or abdominal discomfort when combined with semaglutide due to overlapping GI side effects. Fluoroquinolones require monitoring for both hypoglycemia and hyperglycemia, particularly in patients with diabetes, as noted in an FDA Drug Safety Communication. This concern exists independently of semaglutide use.
For patients taking oral semaglutide (Rybelsus), timing considerations are important. Rybelsus must be taken on an empty stomach with no more than 4 oz (120 mL) of plain water, and patients must wait at least 30 minutes before consuming food, beverages, or other oral medications. Some antibiotics have specific administration requirements (e.g., tetracyclines and fluoroquinolones should not be taken with products containing calcium, magnesium, or aluminum). Patients should consult their pharmacist about optimal timing to ensure both medications are absorbed effectively. Injectable semaglutide formulations (Ozempic, Wegovy) do not have these timing restrictions.
When you need antibiotics while taking semaglutide, providing your healthcare provider with comprehensive medication information is essential for safe and effective treatment. Always inform your doctor that you are taking semaglutide, specifying the brand name (Ozempic, Wegovy, or Rybelsus), dose, and how long you have been on the medication. This information helps your provider assess your current metabolic status and anticipate potential side effects.
Discuss your current diabetes control if you have type 2 diabetes. Infections can affect blood glucose levels independently of medications, often causing hyperglycemia due to stress hormones and inflammatory responses. Your doctor needs to know your recent hemoglobin A1c, typical glucose readings, and whether you have experienced any recent hypoglycemic episodes. Some antibiotics, particularly fluoroquinolones, can cause unpredictable glucose fluctuations that may require closer monitoring or temporary adjustment of diabetes medications.
Report any gastrointestinal symptoms you are currently experiencing from semaglutide. If you are already dealing with nausea, vomiting, or diarrhea, your doctor may choose an antibiotic less likely to worsen these symptoms or may recommend anti-nausea medications. Additionally, mention any history of antibiotic-associated complications, such as Clostridioides difficile infection or severe allergic reactions, as these factors influence antibiotic selection regardless of semaglutide use.
Provide a complete list of all medications, supplements, and over-the-counter products you take. If you take levothyroxine and Rybelsus, this is especially important to mention due to potential increased levothyroxine exposure. Also share your kidney function history, as dehydration from GI side effects can affect renal function. While antibiotics and semaglutide can be used together, other medications in your regimen might interact with either drug. Finally, discuss any upcoming procedures or significant life events, as these may affect treatment duration and monitoring requirements.
The primary challenge when taking antibiotics and semaglutide concurrently is managing overlapping gastrointestinal side effects. Both medication classes commonly cause nausea, and antibiotics frequently cause diarrhea, while semaglutide can cause either diarrhea or constipation. For antibiotics that can be taken with food, doing so may reduce stomach irritation—but always follow the specific instructions for your antibiotic, as some must be taken on an empty stomach. If you are taking oral semaglutide (Rybelsus), maintain the required 30-minute separation between Rybelsus and any food, beverages, or other medications.
Maintain adequate hydration, especially if you experience diarrhea or vomiting. Dehydration can worsen both medication side effects and may affect kidney function, which is particularly important if you are taking antibiotics that are renally cleared. If you have heart or kidney disease, ask your healthcare provider for specific hydration recommendations. Dehydration can also concentrate medications in the bloodstream, potentially intensifying side effects.
Monitor your blood glucose levels more frequently if you have diabetes. Infections typically raise blood sugar, but the combination of illness, antibiotics, reduced food intake due to nausea, and semaglutide's glucose-lowering effects can create unpredictable patterns. Check your glucose before meals and at bedtime, and contact your healthcare provider if readings are consistently above 250 mg/dL or below 70 mg/dL, or if you cannot eat or drink due to gastrointestinal symptoms. Your clinician may advise temporarily pausing semaglutide if you're unable to keep fluids down or are at risk of significant dehydration.
Know when to seek medical attention. Contact your healthcare provider if you experience severe or persistent vomiting that prevents you from taking medications or staying hydrated, signs of dehydration (dark urine, dizziness, rapid heartbeat), severe abdominal pain that differs from typical semaglutide-related discomfort, or signs of allergic reaction to the antibiotic (rash, difficulty breathing, swelling). Be alert for possible C. difficile infection (watery diarrhea three or more times daily, fever, abdominal cramps, or diarrhea persisting after antibiotics end). If you have diabetes and develop symptoms of diabetic ketoacidosis—including excessive thirst, frequent urination, confusion, or fruity-smelling breath—seek emergency care immediately, as infections can precipitate this serious complication regardless of medication use.
No, you typically do not need to stop semaglutide before taking antibiotics. There are no direct drug interactions that require discontinuation, though your healthcare provider may recommend temporarily pausing semaglutide if you develop severe vomiting or dehydration.
Antibiotics do not directly interfere with semaglutide's effectiveness for weight loss or diabetes management. However, infections themselves can raise blood glucose levels and may temporarily affect your overall metabolic control regardless of medication use.
Take antibiotics with food if permitted by the specific medication instructions, stay well-hydrated, and contact your healthcare provider if nausea becomes severe or prevents you from keeping down fluids. Your doctor may recommend anti-nausea medications or temporarily adjusting your treatment plan.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.