LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Why do GLP-1 medications cause headaches? This common concern affects many patients starting glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), or dulaglutide (Trulicity) for type 2 diabetes or weight management. Headaches occur in approximately 4-14% of patients depending on the specific medication and dose. While the exact mechanism isn't fully understood, headaches likely result from dehydration due to gastrointestinal side effects, blood glucose fluctuations, or metabolic changes during treatment initiation. Understanding why these headaches occur and how to manage them effectively helps patients continue beneficial therapy while minimizing discomfort.
Quick Answer: GLP-1 medications cause headaches primarily through dehydration from gastrointestinal side effects, blood glucose fluctuations, and metabolic changes during treatment.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), among others. Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist that works through similar but expanded mechanisms. These medications work by mimicking the action of naturally occurring GLP-1, an incretin hormone produced in the intestines in response to food intake.
The mechanism of action involves several physiological pathways. GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion while suppressing inappropriate glucagon release. This dual action helps regulate blood glucose levels without causing significant hypoglycemia when used as monotherapy (though risk increases when combined with insulin or sulfonylureas). Additionally, these medications slow gastric emptying, which contributes to improved postprandial glucose control and promotes satiety.
Beyond glycemic effects, GLP-1 receptor agonists act on receptors in the central nervous system, particularly in areas regulating appetite and food intake. This central action contributes to weight loss by reducing hunger and caloric intake. Some of these medications have demonstrated cardiovascular benefits in specific populations. Liraglutide, injectable semaglutide, and dulaglutide have FDA-recognized cardiovascular risk reduction in patients with established cardiovascular disease, while Wegovy is indicated for cardiovascular risk reduction in adults with established cardiovascular disease and either overweight or obesity.
While GLP-1 receptor agonists offer significant therapeutic benefits, they can produce various side effects. Understanding how these medications work throughout the body helps explain why certain adverse effects, including headaches, may occur during treatment. The widespread distribution of GLP-1 receptors means these medications can affect multiple organ systems simultaneously.
Headaches are a recognized adverse effect of GLP-1 receptor agonist therapy, though they vary in frequency across different medications, doses, and patient populations. According to FDA prescribing information, headache incidence differs by product and indication. For example, in clinical trials of semaglutide (Ozempic) for type 2 diabetes, headaches were reported in approximately 4-8% of patients depending on dose. For semaglutide (Wegovy) used for weight management, headache rates ranged from 8-14% across different doses. Liraglutide showed similar patterns, while tirzepatide trials documented headaches in approximately 5-7% of patients receiving therapeutic doses for diabetes.
The exact mechanism by which these medications cause headaches is not fully established, but several plausible theories exist. First, these medications significantly alter gastrointestinal function by slowing gastric emptying, which can lead to nausea, vomiting, and dehydration—all potential headache triggers. Dehydration from gastrointestinal side effects, as noted in FDA Medication Guides, may contribute substantially to headache development, especially during the initial treatment period when these effects are most pronounced.
Another consideration involves the medications' effects on blood glucose regulation. While GLP-1 receptor agonists typically have a low risk of hypoglycemia when used alone, fluctuations in glucose levels—particularly when combined with insulin or sulfonylureas—may trigger headaches in susceptible individuals. Additionally, rapid weight loss associated with these medications might sometimes precipitate headaches through various metabolic changes, though this mechanism requires further study.
Headaches associated with GLP-1 therapy are typically most common during the initial weeks of treatment or following dose escalation. Most patients experience improvement as their bodies adjust to the medication. The headaches are generally mild to moderate in intensity and often resolve spontaneously. However, persistent or severe headaches warrant medical evaluation to exclude other causes and ensure appropriate management. Individual responses vary considerably, and some patients may require treatment adjustments if headaches persist or significantly affect quality of life.
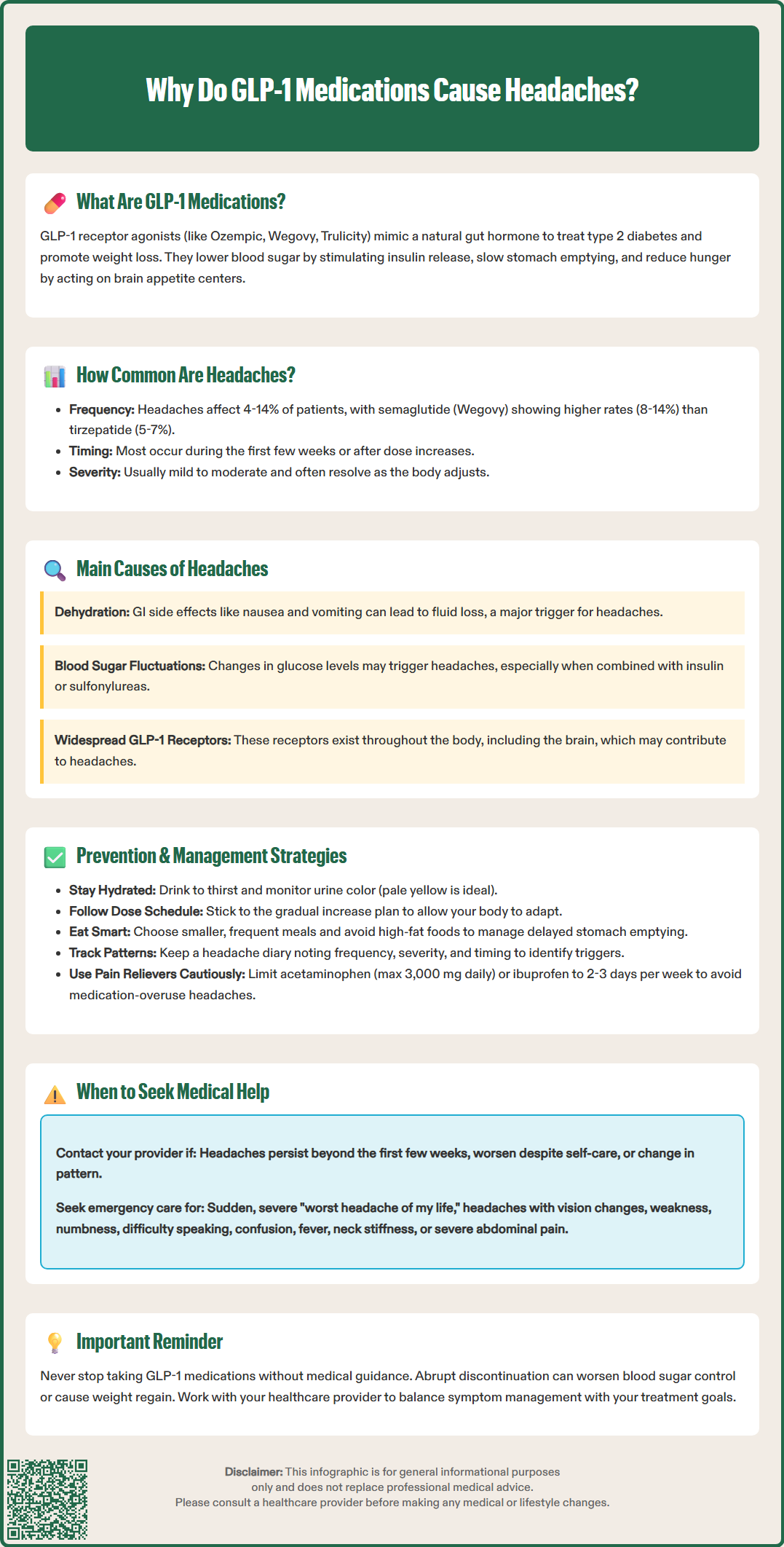
Effective management of GLP-1-related headaches begins with preventive strategies and supportive care measures. Adequate hydration represents an important intervention. Patients should maintain appropriate fluid intake based on individual needs, drinking to thirst and monitoring urine color (pale yellow indicates adequate hydration). Patients with kidney disease or heart failure should follow their healthcare provider's specific fluid recommendations. Increased fluid intake may be needed if experiencing nausea, vomiting, or diarrhea, as dehydration frequently underlies headaches in patients taking these medications.
Gradual dose titration helps minimize adverse effects, including headaches. Healthcare providers typically prescribe GLP-1 medications using a step-wise approach, starting with lower doses and increasing gradually over several weeks. This allows the body to adapt to the medication's effects. Patients should never accelerate the titration schedule without medical guidance, as this may worsen side effects without improving therapeutic outcomes.
Dietary modifications can reduce headache frequency. Eating smaller, more frequent meals helps manage the delayed gastric emptying caused by GLP-1 medications. Avoiding trigger foods—particularly those high in fat, which further slow gastric emptying—may decrease nausea and associated headaches. Maintaining consistent meal timing helps stabilize blood glucose levels, potentially reducing headache occurrence.
Over-the-counter pain relief may be appropriate for managing acute headaches. Acetaminophen (Tylenol) can provide symptomatic relief but should not exceed 3,000 mg daily. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are alternatives but should be used cautiously in patients with cardiovascular disease, kidney impairment, history of GI ulcers, or those taking anticoagulants. To prevent medication-overuse headache, limit analgesic use to no more than 2-3 days per week.
Additional supportive measures include:
Rest and stress management: Adequate sleep and stress reduction techniques may decrease headache frequency
Cold or warm compresses: Applied to the forehead or neck for symptomatic relief
Caffeine moderation: Maintaining consistent caffeine intake, as both excess and withdrawal can trigger headaches
Blood glucose monitoring: Ensuring glucose levels remain stable, particularly when combining GLP-1 medications with insulin or sulfonylureas; treat hypoglycemia (glucose <70 mg/dL) promptly using the rule of 15 (15g carbohydrate, wait 15 minutes, recheck)
Patients should maintain a headache diary documenting frequency, severity, timing, and associated symptoms. This information helps healthcare providers identify patterns and optimize management strategies.
While most GLP-1-related headaches are mild and self-limiting, certain presentations require prompt medical evaluation. Patients should contact their healthcare provider if headaches persist beyond the first few weeks of treatment or worsen despite supportive measures. Persistent headaches may indicate the need for dose adjustment, additional interventions, or investigation of alternative causes.
Severe or sudden-onset headaches warrant immediate medical attention. A headache described as "the worst headache of my life" or one that reaches maximum intensity within seconds to minutes requires emergency evaluation to exclude serious conditions such as intracranial hemorrhage or other neurological emergencies. While there is no established link between GLP-1 medications and such conditions, new severe headaches always require thorough assessment.
Patients should seek medical advice if headaches are accompanied by:
Neurological symptoms: Vision changes, weakness, numbness, difficulty speaking, confusion, or loss of consciousness
Severe nausea and vomiting: Particularly if unable to maintain adequate hydration or take medications for more than 24 hours
Signs of dehydration: Markedly decreased urination, dark urine, dizziness, rapid heartbeat, or dry mucous membranes
Fever or neck stiffness: Which may suggest infection requiring evaluation
Changes in headache pattern: New characteristics in patients with pre-existing headache disorders
New onset after age 50: Headaches beginning later in life require evaluation
Severe, persistent abdominal pain with or without vomiting: May indicate pancreatitis, a rare but serious side effect of GLP-1 medications requiring immediate medical attention
Healthcare providers may recommend several approaches when evaluating persistent headaches. Initial assessment typically includes reviewing medication adherence, hydration status, dietary habits, and concurrent medications. Blood glucose monitoring helps identify hypoglycemia or significant fluctuations. Laboratory testing may assess electrolyte balance and kidney function, particularly if dehydration is suspected.
Dose modification represents a common management strategy. Temporarily reducing the GLP-1 medication dose or extending the titration schedule may allow better tolerance while maintaining therapeutic benefits. In cases where headaches significantly impact quality of life despite optimization efforts, switching to an alternative agent or considering different therapeutic approaches may be necessary.
Patients should never discontinue GLP-1 medications without medical guidance, as abrupt cessation may lead to worsening glycemic control or weight regain. Healthcare providers can develop individualized plans balancing symptom management with therapeutic goals, ensuring optimal outcomes while minimizing adverse effects.
Most GLP-1-related headaches are temporary and improve within the first few weeks of treatment as the body adjusts to the medication. Headaches may recur briefly after dose increases but typically resolve with continued use and supportive measures like adequate hydration.
Yes, over-the-counter pain relievers like acetaminophen or ibuprofen are generally safe for managing GLP-1-related headaches. However, limit use to 2-3 days per week to prevent medication-overuse headaches, and consult your healthcare provider if you have kidney disease, cardiovascular conditions, or take anticoagulants.
Do not discontinue GLP-1 medications without medical guidance, as this may worsen blood glucose control or cause weight regain. Most headaches improve with hydration, dietary adjustments, and time. Contact your healthcare provider if headaches are severe, persistent, or accompanied by neurological symptoms for appropriate evaluation and management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.