LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Anti-tirzepatide antibody reactions occur when the immune system produces proteins in response to tirzepatide (Mounjaro, Zepbound), a dual GIP and GLP-1 receptor agonist used for type 2 diabetes and weight management. According to FDA prescribing information, approximately 4-5% of patients develop these antibodies during treatment, though most cases involve low antibody levels that don't significantly affect medication efficacy or safety. Understanding antibody formation helps patients and clinicians distinguish between normal immune responses and clinically significant reactions requiring intervention. This article examines the development, symptoms, diagnosis, and management of anti-tirzepatide antibodies in clinical practice.
Quick Answer: Anti-tirzepatide antibodies develop in approximately 4-5% of patients but rarely cause clinically significant problems, with most patients maintaining therapeutic benefit without treatment changes.
Anti-tirzepatide antibodies are immune proteins that the body may produce in response to tirzepatide (Mounjaro, Zepbound), a synthetic peptide drug that acts as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. These antibodies develop when the immune system recognizes tirzepatide as a foreign substance, despite the medication being designed to mimic naturally occurring hormones involved in glucose regulation and appetite control.
Tirzepatide is administered by subcutaneous injection for the treatment of type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with weight-related comorbidities. Like other injectable peptide medications, tirzepatide has the potential to trigger an immune response. The formation of anti-drug antibodies is a recognized phenomenon with many injectable therapies and does not necessarily indicate a serious adverse reaction.
Two types of antibodies may form: binding antibodies, which simply attach to the medication, and neutralizing antibodies, which can potentially interfere with the drug's activity. According to FDA prescribing information, most detected antibodies in clinical trials did not impact the efficacy or safety of tirzepatide.
When anti-tirzepatide antibodies form, they may bind to the medication, but in most cases, antibody formation occurs at low levels and does not significantly impact clinical outcomes. Understanding this immune response is important for both patients and healthcare providers to ensure optimal treatment outcomes and appropriate monitoring during therapy.
The development of these antibodies represents a normal immunologic response rather than a true allergic reaction in most instances, though the clinical significance varies among individuals and requires careful assessment during treatment.
The clinical presentation of anti-tirzepatide antibody reactions varies considerably, and many patients with detectable antibodies remain entirely asymptomatic. When symptoms do occur, they typically fall into two categories: local injection site reactions and systemic manifestations that may suggest reduced medication efficacy.
Local injection site reactions may include:
Persistent redness, swelling, or induration at injection sites
Itching or burning sensation that extends beyond typical injection discomfort
Delayed reactions occurring hours to days after administration
Nodule formation or skin changes at injection sites
These local reactions differ from common injection site responses, which typically resolve within days and occur as expected medication effects rather than antibody-mediated responses. According to the FDA prescribing information, injection site reactions occur in approximately 1.7-5.2% of patients receiving tirzepatide, depending on the dose.
Systemic manifestations potentially suggesting reduced efficacy may include:
Unexplained loss of glycemic control in patients with type 2 diabetes, evidenced by rising hemoglobin A1c or fasting glucose levels
Diminished appetite suppression or return of hunger despite continued treatment
Weight loss plateau or weight regain without changes in diet or activity
Reduced gastrointestinal effects that were previously present
It's important to note that these systemic signs are non-specific and may reflect medication storage issues, injection technique problems, treatment adaptation, or disease progression rather than antibody formation.
True hypersensitivity reactions—including urticaria, angioedema, bronchospasm, or anaphylaxis—are extremely rare with tirzepatide but represent serious adverse events requiring immediate medical attention and reporting to the FDA MedWatch program. These reactions differ from antibody-mediated responses and typically occur within minutes to hours of injection. Most patients with detectable anti-tirzepatide antibodies continue to experience therapeutic benefit without any noticeable symptoms, and the presence of antibodies does not automatically necessitate treatment discontinuation.
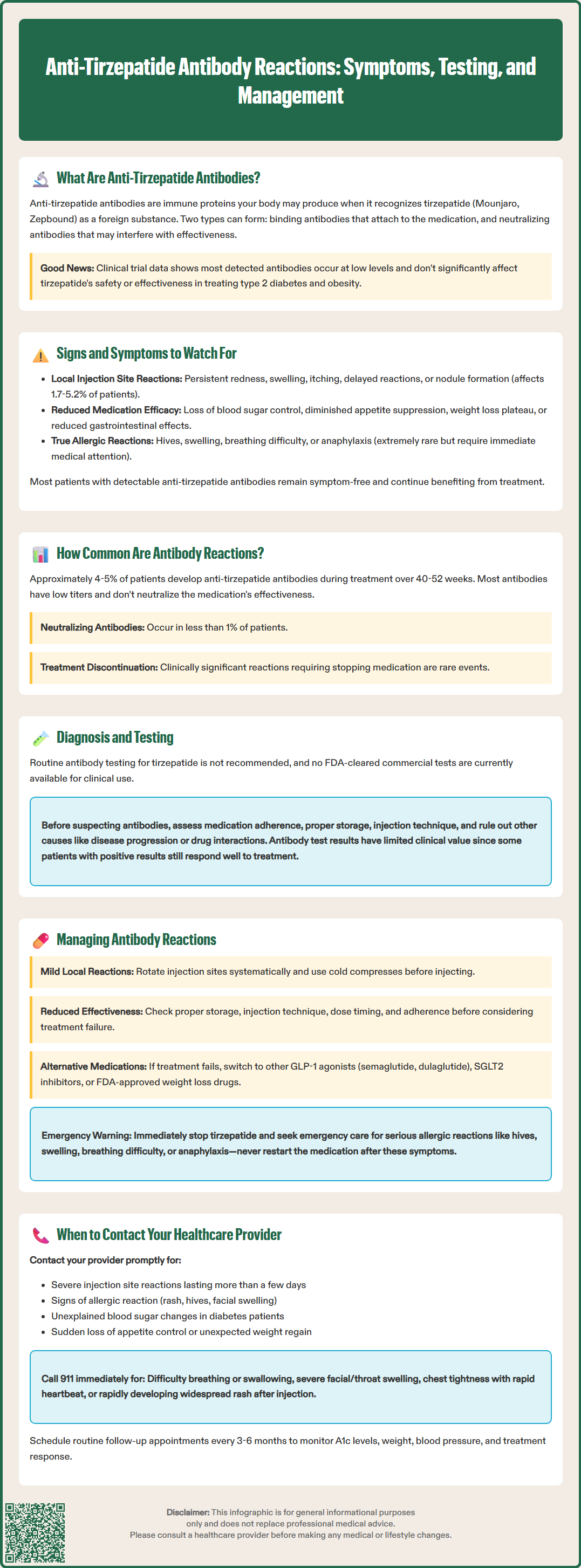
According to FDA prescribing information, anti-tirzepatide antibodies develop in a minority of patients receiving the medication. In the pivotal SURPASS clinical trial program evaluating tirzepatide for type 2 diabetes, approximately 4-5% of patients developed anti-tirzepatide antibodies during the study periods, which ranged from 40 to 52 weeks. Among patients receiving tirzepatide for chronic weight management in the SURMOUNT trials, similar rates of antibody formation were observed.
Importantly, the presence of antibodies did not correlate with increased adverse events or significant loss of efficacy in the majority of cases. Among those who developed antibodies, most had low antibody titers that did not appear to neutralize the medication's therapeutic effects. Neutralizing antibodies—those capable of blocking tirzepatide's action at GIP and GLP-1 receptors—were detected in less than 1% of treated patients across clinical trials.
It should be noted that immunogenicity assay results are highly dependent on the sensitivity and specificity of the particular test used. The FDA emphasizes that immunogenicity data are product- and assay-specific and should not be compared across different medications, as different testing methods can yield varying results.
Clinically significant antibody reactions—those resulting in treatment failure, serious hypersensitivity, or medication discontinuation—remain rare events. Most patients who develop antibodies continue treatment successfully without intervention. However, individual patient responses vary, and ongoing monitoring remains appropriate for all patients receiving tirzepatide therapy, particularly those experiencing unexpected changes in treatment response or unusual injection site reactions.
Routine testing for anti-tirzepatide antibodies is not recommended for all patients receiving the medication. Currently, no FDA-cleared clinical tests for anti-tirzepatide antibodies are commercially available. Immunogenicity assays are typically research tools or manufacturer-specific tests not routinely accessible to clinicians outside of clinical trials.
Indications for considering clinical evaluation include:
Unexplained loss of glycemic control after initial treatment response in patients with type 2 diabetes
Significant reduction in weight loss velocity or weight regain without identifiable behavioral or dietary causes
Persistent or severe injection site reactions that differ from typical responses
Suspected hypersensitivity reactions requiring investigation
When antibody-related issues are suspected, the initial focus should be on clinical evaluation rather than antibody testing. This includes assessing medication adherence, proper storage conditions, injection technique, and ruling out other causes of treatment failure such as disease progression or medication interactions.
For patients with suspected hypersensitivity reactions or unusual treatment responses, referral to an endocrinologist, allergist, or immunologist may be appropriate. These specialists can provide comprehensive evaluation and determine if further investigation is warranted.
If antibody testing is pursued in specialized settings, it involves immunoassays that detect and quantify anti-tirzepatide antibodies in serum samples. These assays typically use enzyme-linked immunosorbent assay (ELISA) or electrochemiluminescence techniques. If antibodies are detected, additional testing may determine whether they are neutralizing antibodies capable of blocking tirzepatide's pharmacologic action.
It is important to recognize that antibody testing has limitations. The clinical significance of positive results remains uncertain in many cases, as some patients with detectable antibodies maintain excellent treatment responses. Conversely, treatment failure may occur without detectable antibodies due to other factors such as injection technique issues, medication storage problems, or disease progression. Therefore, clinical assessment remains the cornerstone of evaluation rather than relying solely on antibody testing.
Management of suspected or confirmed anti-tirzepatide antibody reactions requires individualized assessment based on the severity of symptoms, impact on treatment efficacy, and patient preferences. There is no standardized protocol, as clinical experience with this specific scenario remains limited given the medication's relatively recent approval and low incidence of clinically significant antibody formation.
For local injection site reactions potentially related to antibodies:
Rotate injection sites systematically among recommended areas (abdomen, thigh, upper arm)
Apply cold compresses before injection and warm compresses afterward if tolerated
Consult with your healthcare provider before using any topical treatments, including corticosteroids, which should only be used short-term if recommended
Ensure proper injection technique and medication storage
Monitor for progression or systemic symptoms
Mild local reactions that do not worsen over time may be managed conservatively with continued treatment and observation. However, progressive or severe local reactions warrant medical evaluation.
For suspected loss of efficacy:
Verify medication storage, handling, and injection technique
Review adherence patterns and timing of doses
Assess for other factors affecting treatment response (dietary changes, new medications, intercurrent illness)
Consider dose optimization within approved ranges if not already at maximum dose
Evaluate alternative explanations for treatment failure
If treatment failure persists despite addressing these factors, options include:
Switching to an alternative GLP-1 receptor agonist (semaglutide, dulaglutide) or other therapy
For diabetes management: considering ADA-recommended alternatives such as metformin optimization, SGLT2 inhibitors, or basal insulin
For weight management: exploring other FDA-approved anti-obesity medications
Intensifying lifestyle interventions and behavioral support
For suspected hypersensitivity reactions: Immediate discontinuation of tirzepatide is warranted for any signs of serious hypersensitivity, including urticaria, angioedema, difficulty breathing, or anaphylaxis. These patients should not be rechallenged with tirzepatide under any circumstances, as stated in the FDA prescribing information. Referral to an allergist or immunologist is recommended, and alternative therapeutic options should be pursued.
Most patients with detectable antibodies continue treatment successfully without specific interventions. Close communication between patients and healthcare providers ensures appropriate monitoring and timely adjustments when needed.
Patients receiving tirzepatide should maintain regular follow-up with their healthcare providers, but certain situations warrant prompt contact outside of scheduled appointments. Understanding when to seek medical advice helps ensure patient safety and optimal treatment outcomes.
Contact your healthcare provider promptly if you experience:
Severe or worsening injection site reactions including extensive redness, swelling, warmth, or pain that spreads beyond the immediate injection area, or reactions that persist for more than a few days
Signs of possible allergic reaction such as widespread rash, hives, itching, facial swelling, difficulty breathing, rapid heartbeat, or dizziness
Unexplained changes in blood glucose control if you have diabetes, particularly if home glucose monitoring shows consistently elevated readings despite medication adherence
Sudden loss of appetite suppression or return of intense hunger after previously experiencing good control
Unexpected weight regain without changes in diet or physical activity
New or unusual symptoms that concern you or differ from your previous experience with the medication
Seek emergency medical attention immediately (call 911) for:
Difficulty breathing or swallowing
Severe swelling of the face, lips, tongue, or throat
Rapid heartbeat with chest tightness
Severe dizziness or fainting
Widespread hives or rash developing rapidly after injection
These symptoms may indicate anaphylaxis or serious hypersensitivity, which require urgent evaluation and treatment regardless of antibody status.
Routine follow-up should include: Regular monitoring of hemoglobin A1c (for diabetes patients), weight, blood pressure, and assessment of treatment response and tolerability. According to American Diabetes Association guidelines, patients with diabetes should have A1c tested at least every 3 months if not at goal or if therapy has changed, and at least twice yearly if stable at goal. Most patients should have follow-up appointments every 3-6 months during tirzepatide therapy, with more frequent visits during dose titration or if concerns arise. Open communication with your healthcare team about your treatment experience, including both benefits and side effects, enables appropriate adjustments and ensures the best possible outcomes with tirzepatide therapy.
No, most patients with detectable anti-tirzepatide antibodies continue treatment successfully without discontinuation. Only severe hypersensitivity reactions such as anaphylaxis require immediate medication cessation and alternative therapy.
No FDA-cleared clinical tests for anti-tirzepatide antibodies are commercially available. Testing is typically limited to research settings or manufacturer-specific assays not routinely accessible to clinicians outside clinical trials.
First verify proper medication storage, injection technique, and adherence. Discuss with your healthcare provider to rule out other causes such as dietary changes, new medications, or disease progression before attributing reduced efficacy to antibody formation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.