LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) represents a breakthrough in type 2 diabetes and weight management as the first dual GIP/GLP-1 receptor agonist approved by the FDA. While clinical trials demonstrate significant efficacy, some patients experience suboptimal results or apparent treatment failure. Understanding why tirzepatide may not work effectively requires examining multiple factors including medication adherence, dosing adequacy, underlying medical conditions, and realistic expectations. This article explores the physiological mechanisms, common barriers to success, and evidence-based strategies to optimize treatment outcomes for patients not achieving expected results with tirzepatide therapy.
Quick Answer: Tirzepatide may not work effectively due to inadequate dosing, poor medication adherence, advanced beta-cell dysfunction, severe insulin resistance, improper injection technique, or unrealistic expectations about treatment timelines and outcomes.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This novel mechanism distinguishes it from single-receptor GLP-1 agonists by targeting two complementary pathways involved in glucose homeostasis and appetite regulation.
The medication works primarily by enhancing glucose-dependent insulin secretion from pancreatic beta cells, meaning insulin release occurs only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to insulin or sulfonylureas, though the risk increases when used with these medications. Simultaneously, tirzepatide suppresses inappropriate glucagon secretion from pancreatic alpha cells, which helps prevent excessive hepatic glucose production. The GLP-1 component slows gastric emptying, prolonging satiety and reducing postprandial glucose excursions.
Beyond glycemic control, tirzepatide acts on hypothalamic appetite centers to reduce hunger and increase feelings of fullness. The dual agonism appears to produce synergistic effects on weight loss, with clinical trials demonstrating up to ~21% body weight reduction at the 15 mg dose in people without diabetes, while weight loss is typically less in type 2 diabetes. The medication may also improve several cardiometabolic parameters including blood pressure, lipid profiles, and markers of hepatic steatosis, though these are not FDA-approved indications.
Tirzepatide is administered once weekly via subcutaneous injection, with a gradual dose escalation protocol to minimize gastrointestinal side effects. Peak plasma concentrations occur approximately 24-48 hours post-injection, with a half-life of approximately five days allowing for steady-state concentrations after four weeks. Understanding this pharmacology is essential when evaluating treatment response, as the full therapeutic effect may not be apparent during the initial titration period.
Importantly, tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
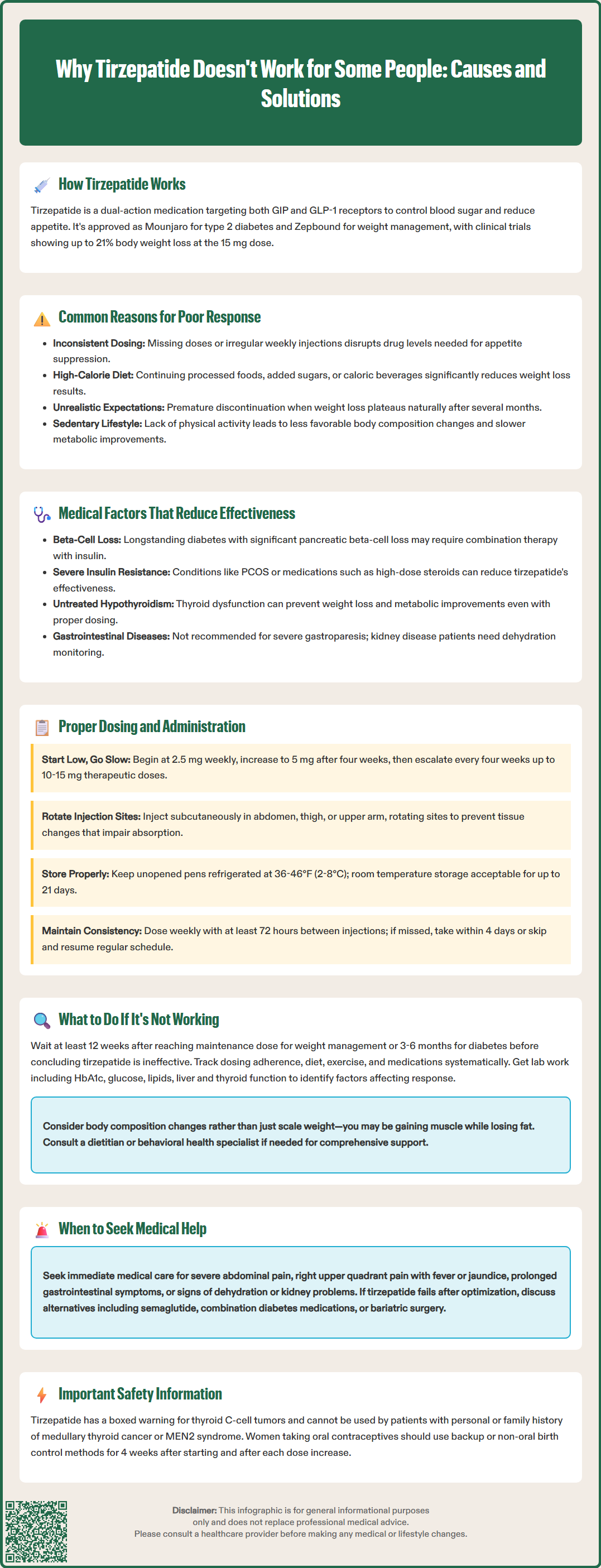
Several non-medical factors can significantly impact tirzepatide's effectiveness, with adherence being the most fundamental consideration. Missing doses or inconsistent administration disrupts the steady-state drug levels necessary for optimal glucose control and appetite suppression. Unlike daily medications where a single missed dose has limited impact, weekly injections require consistent scheduling to maintain therapeutic concentrations. According to FDA guidance, doses should be spaced at least 72 hours apart, and missed doses may be taken within 4 days (96 hours) of the scheduled time. Patients who frequently delay or skip injections may experience suboptimal results and attribute this to medication failure rather than adherence issues.
Dietary habits represent another critical variable in treatment response. While tirzepatide reduces appetite and promotes satiety, it does not eliminate the ability to consume calorie-dense foods. Patients who continue high-calorie diets, particularly those rich in processed foods, added sugars, or caloric beverages (including alcohol), may experience blunted weight loss despite adequate glycemic improvement. The medication enhances physiological satiety signals, but behavioral patterns and food choices remain important determinants of overall success. Some individuals may also compensate for reduced appetite at meals by increasing snacking or consuming caloric beverages.
Unrealistic expectations can lead to perceived treatment failure when outcomes are actually within the expected range. Clinical trial data show considerable individual variation in response, with some patients losing substantially more weight than the average while others experience more modest results. A patient expecting universal dramatic weight loss may discontinue treatment prematurely if their response falls in the lower range of normal. Additionally, weight loss typically plateaus after several months of treatment, and patients may interpret this natural stabilization as medication failure.
Physical activity levels also modulate treatment outcomes. While tirzepatide produces weight loss independent of exercise, sedentary patients generally achieve less favorable body composition changes and may experience slower metabolic improvements. The medication works synergistically with lifestyle modifications rather than replacing them entirely.
Advanced beta-cell dysfunction represents a significant physiological barrier to tirzepatide efficacy. The medication's glucose-lowering mechanism depends on functional pancreatic beta cells capable of responding to incretin stimulation. Patients with longstanding type 2 diabetes often have substantial beta-cell loss, which can vary among individuals, potentially limiting their capacity to increase insulin secretion even with dual GIP/GLP-1 receptor stimulation. In such cases, tirzepatide may produce modest glycemic improvement but fall short of achieving target HbA1c levels. These patients may require combination therapy with basal insulin or other agents targeting different pathophysiological mechanisms.
Severe insulin resistance, particularly in patients with significant visceral adiposity or conditions like polycystic ovary syndrome, can attenuate tirzepatide's effectiveness. While the medication addresses multiple aspects of metabolic dysfunction, extremely insulin-resistant individuals may require higher doses or longer treatment duration to achieve comparable results. Concurrent use of medications that promote insulin resistance—such as high-dose glucocorticoids, certain antipsychotics (olanzapine, clozapine), or immunosuppressants—can directly counteract tirzepatide's benefits and should be identified during treatment evaluation.
Genetic variations in incretin receptor expression and signaling pathways may contribute to variable treatment response, though this remains an area of active research. Preliminary pharmacogenomic studies suggest that polymorphisms in GLP-1 receptor genes could influence both efficacy and tolerability, but clinical genetic testing is not currently recommended for routine practice. Thyroid dysfunction, particularly untreated hypothyroidism, can impair weight loss and metabolic improvement despite adequate tirzepatide dosing.
Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. While no dose adjustment is required for chronic kidney disease, patients should be monitored for volume depletion due to gastrointestinal adverse effects and potential acute kidney injury risk.
Women using oral contraceptives should be aware that tirzepatide may reduce contraceptive effectiveness due to delayed gastric emptying. Non-oral contraception or backup methods are advised for 4 weeks after initiation and after each dose escalation.
Inadequate dose escalation is a frequent cause of suboptimal response to tirzepatide therapy. The FDA-approved titration schedule begins at 2.5 mg weekly for four weeks, primarily as a tolerability dose rather than a therapeutic dose. Many patients experience limited efficacy at this starting dose, which is expected and appropriate. The dose should be increased to 5 mg after four weeks, with subsequent increases to 7.5 mg, 10 mg, 12.5 mg, and finally 15 mg at four-week intervals based on individual response and tolerability. Some patients and clinicians prematurely conclude the medication is ineffective before reaching therapeutic doses of 10-15 mg weekly.
Improper injection technique can compromise drug delivery and therapeutic effect. Tirzepatide should be administered subcutaneously in the abdomen, thigh, or upper arm, with site rotation to prevent lipohypertrophy or lipoatrophy that can impair absorption. Injecting into areas of lipodystrophy, scar tissue, or inflamed skin may result in erratic absorption and unpredictable drug levels. Patients should be educated on proper technique, including allowing the medication to reach room temperature before injection and following the specific instructions for their device as detailed in the manufacturer's Instructions for Use (IFU).
Storage conditions significantly affect medication stability and potency. Tirzepatide must be refrigerated at 36-46°F (2-8°C) and protected from light. Unopened pens may be stored at room temperature (up to 86°F/30°C) for up to 21 days. Pens that have been frozen, exposed to excessive heat, or stored beyond their expiration date may have reduced potency. Traveling patients should use insulated cooling cases to maintain appropriate temperatures, following manufacturer guidance.
Timing inconsistencies can impact steady-state levels. According to FDA labeling, doses should be spaced at least 72 hours apart. If a dose is missed, it can be administered within 4 days (96 hours) of the scheduled time. If more than 4 days have passed, the missed dose should be skipped and the next dose administered on the regularly scheduled day. Establishing a consistent weekly schedule helps maintain appropriate drug concentrations.
If tirzepatide appears ineffective after an adequate trial period, systematic evaluation should precede any treatment changes. For weight management, guidelines recommend reassessment approximately 12 weeks after reaching a maintenance dose to determine whether to continue therapy, though weight loss may continue beyond this timeframe in some patients. For diabetes management, glycemic response should be evaluated after 3-6 months on a stable dose. Patients should maintain detailed records of dosing adherence, dietary intake, physical activity, and concurrent medications to identify potential contributing factors. Premature discontinuation before reaching therapeutic doses or adequate treatment duration is a common error that prevents patients from experiencing the medication's full benefits.
Clinicians should reassess baseline factors and treatment goals during follow-up visits. Laboratory evaluation should include HbA1c, fasting glucose, lipid panel, liver function tests, and thyroid function to identify any underlying metabolic issues affecting response. A comprehensive medication review is essential to identify potential drug interactions or counteractive agents. For diabetes management, if HbA1c remains above target despite maximal tirzepatide dosing, combination therapy with metformin, SGLT2 inhibitors, or basal insulin should be considered based on individual patient factors and contraindications.
For weight management, reassessment should include evaluation of body composition changes rather than scale weight alone, as patients may be gaining muscle mass while losing fat, particularly if they have increased physical activity. Referral to a registered dietitian for medical nutrition therapy can help identify dietary patterns that may be limiting weight loss. Behavioral health evaluation may be appropriate for patients with emotional eating, binge eating disorder, or other psychological factors affecting treatment response.
Patients should be aware of important safety considerations and seek immediate medical attention for persistent severe abdominal pain (with or without vomiting) suggestive of pancreatitis, right upper quadrant pain/fever/jaundice (gallbladder disease), severe or prolonged gastrointestinal symptoms, or signs of dehydration/acute kidney injury.
If tirzepatide remains ineffective despite optimization of all modifiable factors, alternative GLP-1 receptor agonists or other weight management medications may be considered. There is limited evidence that patients who fail to respond to tirzepatide will necessarily respond better to other incretin-based therapies, but individual variation may result in differential responses. Switching to semaglutide (another GLP-1 agonist) represents a reasonable next step. For patients with type 2 diabetes and significant beta-cell dysfunction, intensification with insulin therapy may be necessary. Bariatric surgery consultation should be considered for patients with BMI ≥35 kg/m² with obesity-related complications or ≥40 kg/m² without complications (per ASMBS/IFSO 2022 guidelines), though insurance coverage in the US often requires BMI ≥35 kg/m² with comorbidities or ≥40 kg/m² without.
Tirzepatide reaches steady-state concentrations after approximately four weeks at each dose level. Full therapeutic effects for weight management should be evaluated after 12 weeks at a maintenance dose (typically 10-15 mg weekly), while glycemic response for diabetes is assessed after 3-6 months on a stable dose.
Inadequate dose escalation is the most frequent cause of apparent treatment failure. Many patients remain on the 2.5 mg or 5 mg starting doses, which are primarily for tolerability rather than therapeutic effect, and do not reach the 10-15 mg weekly doses where maximal efficacy typically occurs.
Yes, if tirzepatide remains ineffective after optimization of dose, adherence, and lifestyle factors, switching to alternative GLP-1 receptor agonists like semaglutide or adding complementary diabetes medications may be appropriate. For weight management, other FDA-approved obesity medications or bariatric surgery referral should be considered based on individual patient factors.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.