LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Choosing the best protein while on semaglutide is essential for preserving muscle mass during weight loss. Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management, significantly reduces appetite and caloric intake. While this promotes fat loss, it can also lead to lean muscle loss without adequate protein consumption. High-quality protein sources—including lean poultry, fish, eggs, Greek yogurt, and plant-based options like legumes—help maintain metabolic health and functional capacity. Most patients require 1.2–1.6 grams of protein per kilogram of adjusted body weight daily, distributed across multiple meals. Strategic protein prioritization becomes critical when appetite suppression limits overall food intake.
Quick Answer: The best proteins while on semaglutide are high-quality, easily digestible sources like lean poultry, fish, eggs, Greek yogurt, and legumes, consumed at 1.2–1.6 grams per kilogram of adjusted body weight daily to preserve muscle mass during weight loss.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). By mimicking endogenous GLP-1, semaglutide enhances glucose-dependent insulin secretion, suppresses glucagon release, and significantly reduces appetite through central nervous system pathways. While these mechanisms facilitate weight loss and glycemic control, they also create nutritional challenges that require careful attention.
Adequate protein intake becomes particularly critical during semaglutide therapy because the medication-induced caloric deficit can lead to loss of both adipose tissue and lean body mass. Clinical trials show that while fat mass reduction predominates during semaglutide treatment, some lean mass loss does occur. Without sufficient dietary protein and resistance exercise, this muscle loss may be more pronounced, potentially compromising metabolic health, reducing functional capacity, and diminishing the long-term benefits of weight reduction.
Protein serves multiple essential functions during weight loss: it promotes satiety, supports muscle protein synthesis, maintains metabolic rate, and facilitates tissue repair. For patients taking semaglutide, who often experience appetite suppression and early satiety, prioritizing protein-rich foods becomes a strategic approach to preserving muscle mass while achieving therapeutic weight loss goals. The American Diabetes Association's Standards of Care emphasizes that nutritional adequacy must accompany pharmacologic weight management interventions.
Healthcare providers should counsel patients initiating semaglutide about the importance of protein prioritization, as this nutritional strategy can optimize body composition outcomes and support sustained metabolic improvements throughout treatment. For patients with chronic kidney disease, protein intake should be individualized with guidance from a healthcare provider and registered dietitian.
Semaglutide exerts its appetite-suppressing effects through multiple mechanisms. The medication slows gastric emptying, prolonging the sensation of fullness after meals. It also acts on appetite-regulating centers in the hypothalamus, reducing hunger signals and food cravings. Clinical trials demonstrate that patients taking semaglutide typically experience significant appetite reduction, contributing to the medication's weight loss efficacy.
However, this profound appetite suppression creates a nutritional paradox. While patients consume fewer total calories—a desired outcome for weight management—they may inadvertently reduce intake of essential nutrients, including protein, vitamins, and minerals. Many patients report feeling satisfied after consuming very small portions, which facilitates weight loss but raises concerns about nutritional adequacy and the preservation of lean tissue.
The altered eating patterns associated with semaglutide may lead patients to choose foods based on tolerability rather than nutritional value. Gastrointestinal side effects—including nausea, vomiting, and changes in food preferences—can further limit food choices and reduce protein consumption. Body composition studies from the STEP clinical trials have shown that while fat mass loss is the primary outcome, some lean mass reduction does occur during GLP-1 receptor agonist therapy.
Understanding these medication-specific challenges allows healthcare providers to implement proactive nutritional strategies. Patients should receive guidance on protein prioritization before appetite suppression becomes pronounced, establishing eating patterns that emphasize nutrient-dense, protein-rich foods even when overall food volume decreases. If caloric intake falls below 1,000 calories per day consistently, medical supervision is essential to prevent nutritional deficiencies and excessive lean mass loss.
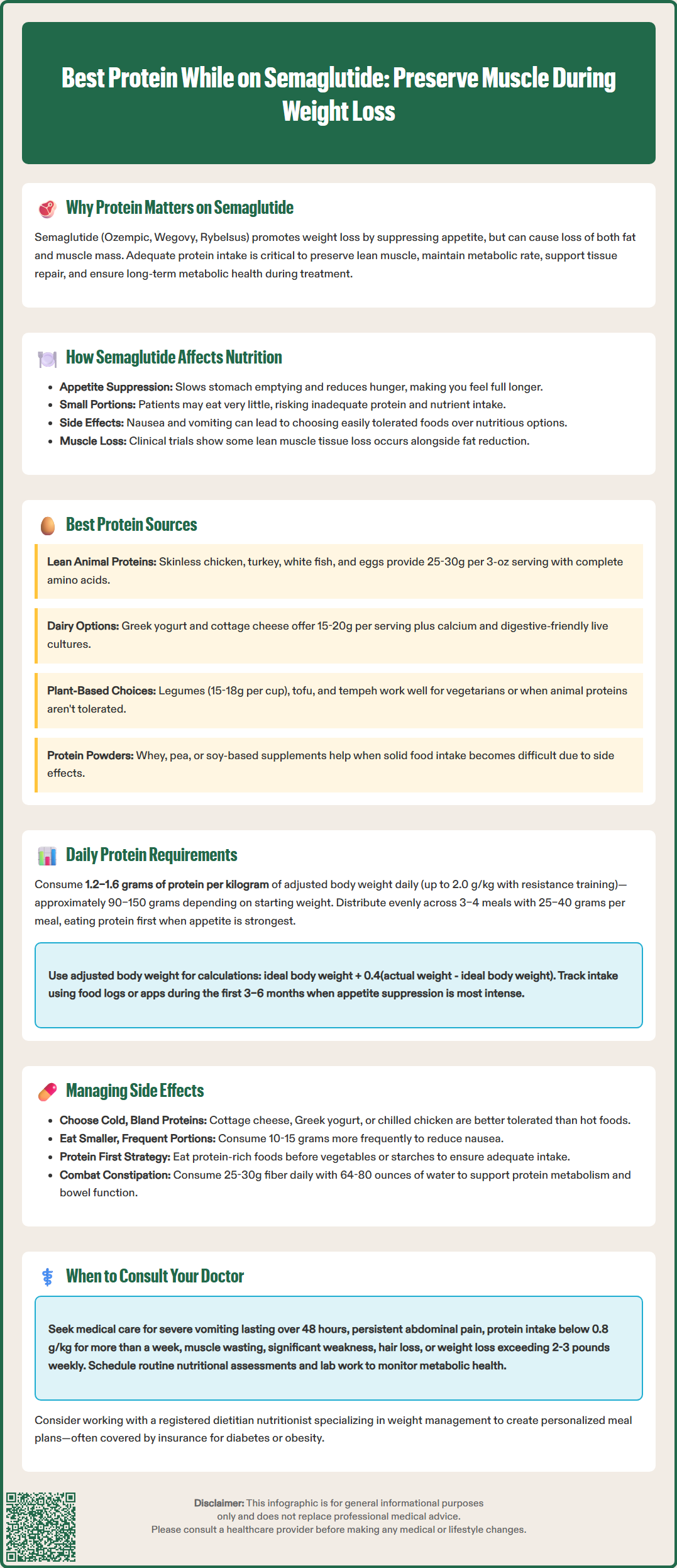
Selecting appropriate protein sources requires consideration of both nutritional density and tolerability during semaglutide treatment. High-quality complete proteins—those containing all essential amino acids—should form the foundation of dietary planning. Lean animal proteins typically offer the highest bioavailability and amino acid profiles for muscle preservation.
Optimal animal-based protein sources include:
Poultry: Skinless chicken breast and turkey provide 25–30 grams of protein per 3-ounce serving with minimal fat, making them easily digestible for patients experiencing gastrointestinal sensitivity.
Fish and seafood: Salmon, cod, tuna, and shrimp offer high-quality protein along with omega-3 fatty acids. White fish varieties are particularly well-tolerated by patients with nausea.
Eggs: Whole eggs or egg whites deliver complete protein in easily adjustable portions, with one large egg providing approximately 6 grams of protein.
Low-fat dairy: Greek yogurt (15–20 grams per 6-ounce serving), cottage cheese, and skim milk provide protein along with calcium. Some patients find that yogurt with live cultures may help with digestive comfort, though evidence for managing semaglutide-specific GI symptoms is limited.
Lean red meat: Sirloin, tenderloin, and 93% lean ground beef offer protein and bioavailable iron, though some patients find these harder to tolerate initially.
Plant-based protein options serve as valuable alternatives or supplements, particularly for patients following vegetarian or vegan diets:
Legumes (lentils, chickpeas, black beans) provide 15–18 grams per cooked cup
Tofu and tempeh offer 10–20 grams per serving with good digestibility
Quinoa and other whole grains contribute complementary protein
Protein powders (whey, casein, pea, or soy-based) can help patients meet targets when solid food intake is limited
Patients should experiment with various protein sources to identify those best tolerated during different treatment phases, recognizing that preferences may shift as side effects evolve.
Determining appropriate protein intake for patients taking semaglutide requires consideration of multiple factors, including baseline body weight, weight loss goals, activity level, and individual tolerance. Standard dietary reference intakes suggest 0.8 grams of protein per kilogram of body weight for sedentary adults, but this baseline recommendation proves insufficient during active weight loss.
For patients undergoing semaglutide-assisted weight reduction, current evidence supports higher protein targets: 1.2–1.6 grams per kilogram of ideal or adjusted body weight daily. Some obesity medicine specialists recommend even higher intakes—up to 2.0 grams per kilogram—particularly for patients engaging in resistance training or those at high risk for sarcopenia. These elevated targets help counteract the catabolic effects of caloric restriction and preserve lean body mass during weight loss.
Calculating adjusted body weight: For individuals with obesity, adjusted body weight = ideal body weight + 0.4(actual weight - ideal body weight)
Practical protein targets using adjusted body weight:
For a 200-pound (91 kg) individual with adjusted weight of 75 kg: 90–120 grams daily
For a 250-pound (114 kg) individual with adjusted weight of 85 kg: 100–135 grams daily
For a 300-pound (136 kg) individual with adjusted weight of 95 kg: 115–150 grams daily
Distributing protein intake across multiple meals optimizes muscle protein synthesis. Research suggests consuming 25–40 grams of protein per meal, spread across three to four eating occasions, provides superior muscle preservation compared to uneven distribution patterns. For semaglutide users with reduced appetite, this may mean prioritizing protein at the beginning of each meal when hunger signals are strongest.
Patients should work with registered dietitians familiar with GLP-1 receptor agonist therapy to establish individualized protein targets. Those with chronic kidney disease require specialized guidance, as high protein intake may not be appropriate. Regular monitoring of dietary intake through food logs or mobile applications can help ensure adequacy, particularly during the first three to six months of treatment when appetite suppression is most pronounced.
Gastrointestinal adverse effects represent the most common tolerability challenges with semaglutide, affecting approximately 40–50% of patients according to FDA prescribing information. Nausea, vomiting, diarrhea, constipation, and abdominal discomfort can significantly impact dietary choices and protein consumption. Strategic protein selection and meal timing can help mitigate these symptoms while maintaining nutritional adequacy.
Nausea management strategies include choosing bland, easily digestible protein sources during symptomatic periods. Cold proteins (such as cottage cheese, Greek yogurt, or chilled chicken) are often better tolerated than hot, aromatic foods. Consuming smaller, more frequent protein portions—10–15 grams per eating occasion rather than large meals—reduces gastric distension and may minimize nausea. Protein shakes or smoothies can provide nutrition when solid foods are poorly tolerated, though patients should sip slowly to avoid overwhelming the delayed gastric emptying.
For patients experiencing early satiety, protein prioritization becomes essential. Eating protein-rich foods first, before consuming vegetables or starches, ensures adequate intake before fullness occurs. This "protein-first" approach, adapted from bariatric nutrition principles, may help maintain lean mass during weight loss interventions. Avoiding excessive fluid intake immediately before or during meals can preserve limited gastric capacity for nutrient-dense foods.
Constipation, another frequent side effect, requires balanced attention to both protein and fiber intake. While increasing dietary fiber through vegetables, fruits, and whole grains helps promote regularity (aiming for 25-30g daily per US Dietary Guidelines), patients should maintain adequate hydration to support both protein metabolism and bowel function. Hydration needs should be individualized, with most adults requiring 64–80 ounces of water daily unless medically restricted. Some patients benefit from incorporating plant-based proteins with inherent fiber content, such as legumes, to address both nutritional needs simultaneously.
Patients experiencing persistent gastrointestinal symptoms that limit protein intake for more than one week should consult their healthcare provider, as dose adjustments or additional supportive interventions may be warranted.
While dietary modifications can often address nutritional challenges during semaglutide therapy, certain situations require professional medical evaluation and intervention. Patients should maintain open communication with their healthcare team regarding dietary tolerance and nutritional adequacy throughout treatment.
Immediate consultation is warranted for:
Severe or persistent nausea and vomiting lasting more than 48 hours or preventing any oral intake, as this may indicate gastroparesis or require medication adjustment
Severe, persistent abdominal pain, which could indicate pancreatitis (a rare but serious adverse effect of GLP-1 medications)
Right upper quadrant pain, fever, or yellowing of skin/eyes, which may suggest gallbladder disease (more common during rapid weight loss)
Unintentional protein intake below 0.8 grams per kilogram of body weight for more than one week, suggesting inadequate nutritional support
Signs of muscle wasting including significant weakness, difficulty with previously manageable physical activities, or visible muscle loss
Symptoms of dehydration such as dark urine, dizziness, or decreased urination, particularly when combined with poor protein intake
Hair loss, brittle nails, or skin changes that may indicate protein-calorie malnutrition
Unexpectedly rapid weight loss exceeding 2–3 pounds per week consistently, which increases risk of lean mass depletion
Routine nutritional assessment should occur at regular intervals during semaglutide treatment. The American Diabetes Association's Standards of Care recommends that patients undergoing significant weight loss receive periodic evaluation of nutritional status, including assessment of dietary adequacy and body composition when possible. Targeted laboratory monitoring based on individual risk factors may include comprehensive metabolic panel, complete blood count, iron studies, vitamin B12 (especially if also taking metformin), and vitamin D.
Referral to a registered dietitian nutritionist (RDN) specializing in weight management or diabetes care provides valuable support for most patients taking semaglutide. These specialists can develop individualized meal plans, provide practical strategies for meeting protein targets despite appetite suppression, and monitor nutritional adequacy throughout treatment. Insurance coverage for medical nutrition therapy is often available for patients with diabetes or obesity-related conditions.
Patients should view nutritional optimization as an integral component of semaglutide therapy rather than an optional consideration, recognizing that medication efficacy and long-term health outcomes depend substantially on maintaining adequate protein and overall nutrient intake during weight loss.
Most patients taking semaglutide should consume 1.2–1.6 grams of protein per kilogram of adjusted body weight daily, distributed across 3–4 meals. This higher intake helps preserve lean muscle mass during caloric restriction and weight loss.
Cold or bland proteins like Greek yogurt, cottage cheese, eggs, white fish, and chilled chicken are typically best tolerated during semaglutide treatment. Protein shakes can also help when nausea makes solid foods difficult to consume.
Yes, protein powders (whey, casein, pea, or soy-based) are valuable options when appetite suppression or nausea limits solid food intake. Sip protein shakes slowly to avoid overwhelming delayed gastric emptying and worsening gastrointestinal symptoms.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.