LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can semaglutide cause allodynia? This question arises as more patients use this GLP-1 receptor agonist for type 2 diabetes and weight management. Allodynia—pain from normally non-painful stimuli like light touch—is a concerning symptom that significantly impacts quality of life. While semaglutide is not currently listed as causing allodynia in FDA prescribing information, patients with diabetes may already be at risk for nerve pain from their underlying condition. Understanding the relationship between semaglutide therapy and neurological symptoms helps patients and clinicians distinguish medication effects from disease-related complications.
Quick Answer: Allodynia is not listed as an adverse effect in FDA-approved prescribing information for semaglutide products.
Allodynia is a symptom of neuropathic pain characterized by pain in response to stimuli that would not normally provoke discomfort. Patients experiencing allodynia may feel significant pain from light touch, gentle pressure, or even temperature changes that healthy individuals would find innocuous. This represents an abnormal processing of sensory information by the nervous system.
The development of allodynia typically involves sensitization of peripheral nerve fibers or alterations in central nervous system pain processing. Common underlying mechanisms include nerve damage (peripheral neuropathy), inflammatory processes affecting nerve tissue, or changes in neurotransmitter function within pain pathways. In metabolic conditions such as diabetes, prolonged hyperglycemia can damage small nerve fibers through multiple pathways including oxidative stress, accumulation of advanced glycation end products, and microvascular insufficiency affecting nerve blood supply.
Allodynia manifests in several forms: mechanical allodynia (pain from touch or pressure), thermal allodynia (pain from temperature changes), and dynamic allodynia (pain from movement across the skin). Beyond diabetes, allodynia commonly occurs in conditions such as postherpetic neuralgia, migraine, complex regional pain syndrome (CRPS), and fibromyalgia. The symptom significantly impacts quality of life, as routine activities like wearing clothing, showering, or light contact become sources of distress. Diagnosis requires careful clinical assessment, including detailed pain history, neurological examination, and sometimes specialized sensory testing to characterize the pain response patterns and identify underlying causes. Atypical presentations with asymmetry, motor deficits, or rapid progression may warrant neurological referral.
Currently, allodynia is not listed as an adverse effect in the FDA-approved prescribing information for semaglutide products (Ozempic, Wegovy, and Rybelsus). Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management, has been extensively studied in clinical trials. The most commonly reported adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, rather than neurological pain syndromes.
Patients with diabetes who initiate semaglutide therapy may already be at risk for diabetic peripheral neuropathy, a common complication of prolonged hyperglycemia that can present with various pain syndromes including allodynia. The temporal association between starting semaglutide and experiencing nerve pain does not necessarily indicate causation, as the underlying diabetes itself remains the more likely etiology.
It is important to note that rapid improvement in glycemic control with any diabetes medication, including semaglutide, can occasionally trigger a condition called treatment-induced neuropathy of diabetes. This presents as acute painful neuropathy following substantial A1c reduction and typically improves over time. This phenomenon relates to the rapid change in glucose levels rather than a direct medication toxicity.
Any new or worsening neurological symptoms warrant thorough clinical evaluation to distinguish between medication effects, disease progression, or unrelated conditions. Patients who suspect they may be experiencing a medication-related adverse effect should report this to their healthcare provider and consider reporting to the FDA MedWatch program.
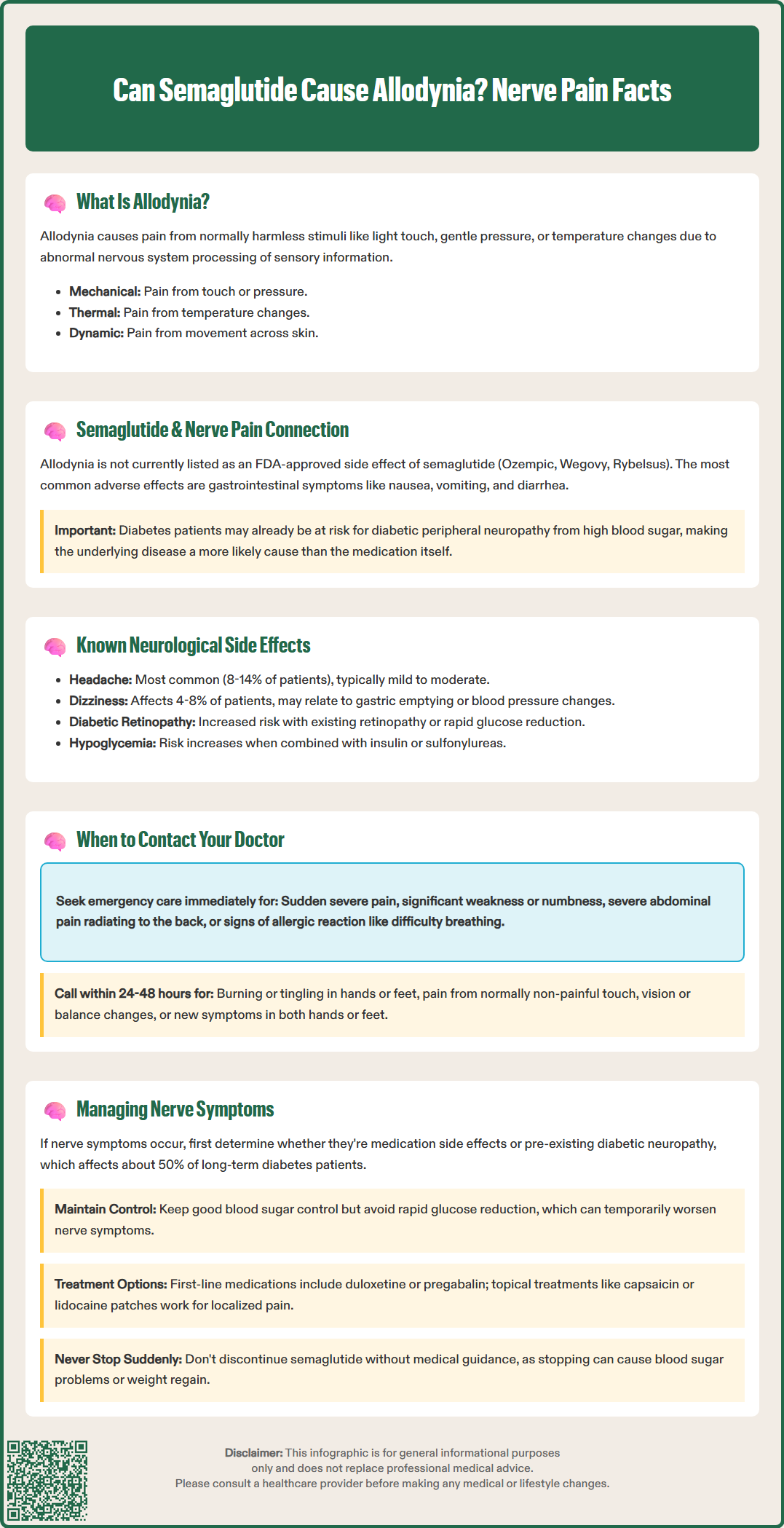
Dizziness has been reported in clinical studies, affecting approximately 6-8% of patients receiving Wegovy and 4% of patients receiving Ozempic. This symptom may relate to the medication's effects on gastric emptying, changes in blood pressure, or glucose fluctuations. Hypoglycemia risk increases when semaglutide is used in combination with insulin or sulfonylureas. Dizziness episodes are generally transient and do not necessitate treatment discontinuation in most cases.
The SUSTAIN-6 cardiovascular outcomes trial identified a statistically significant increase in diabetic retinopathy complications among semaglutide-treated patients, particularly those with pre-existing retinopathy and rapid glucose reduction. This finding led to a warning in the prescribing information recommending appropriate monitoring in patients with diabetic retinopathy. Patients with a history of diabetic retinopathy should be monitored by an ophthalmologist during semaglutide treatment.
Other neurological symptoms such as peripheral neuropathy, paresthesias, or allodynia have not been consistently reported as adverse effects attributable to semaglutide in controlled trials. The American Diabetes Association guidelines emphasize that neuropathic symptoms in diabetic patients are far more commonly related to glycemic control history and diabetes duration than to specific glucose-lowering medications.
Patients experiencing new or unusual pain symptoms while taking semaglutide should contact their healthcare provider for evaluation, particularly if the pain is severe, progressive, or significantly impacts daily functioning. Specific warning signs warrant different levels of medical attention:
Seek emergency care (call 911 or go to the emergency department) for:
Sudden onset of severe pain that differs from previous experiences
Pain accompanied by significant weakness, numbness, or loss of sensation
Severe abdominal pain, especially if radiating to the back (possible pancreatitis)
Severe right upper quadrant abdominal pain (possible gallbladder disease)
Signs of severe allergic reaction (difficulty breathing, severe rash, swelling)
Contact your doctor promptly (within 24-48 hours) for:
Burning, tingling, or electric shock-like sensations in hands or feet
Pain triggered by normally non-painful stimuli (potential allodynia)
Pain associated with changes in vision, balance problems, or coordination difficulties
New symmetrical symptoms in both hands or feet
Patients should provide their physician with detailed information about pain characteristics, including onset timing relative to semaglutide initiation, location, quality (burning, stabbing, aching), severity on a 0-10 scale, aggravating and relieving factors, and any associated symptoms.
It is particularly important not to discontinue semaglutide without medical guidance, as abrupt cessation may lead to deterioration in glycemic control or weight regain. Healthcare providers can assess whether symptoms represent a true adverse drug reaction, progression of underlying diabetic neuropathy, or an alternative diagnosis requiring specific investigation. Patients and healthcare providers are encouraged to report suspected adverse effects to the FDA MedWatch program.
If nerve-related symptoms develop during semaglutide therapy, a systematic approach to evaluation and management is essential. The first priority involves determining whether symptoms represent true medication-related adverse effects or reflect underlying diabetic neuropathy, which affects approximately 50% of patients with long-standing diabetes.
Diagnostic evaluation may include:
Detailed neurological examination assessing sensation, reflexes, and motor function
Hemoglobin A1c measurement to evaluate recent glycemic control
Vitamin B12 levels and methylmalonic acid (if B12 is borderline)
Serum protein electrophoresis (SPEP) and immunofixation to screen for paraproteinemia
Thyroid function tests, as hypothyroidism can contribute to neuropathic symptoms
Comprehensive metabolic panel to assess renal and hepatic function
Nerve conduction studies in selected cases with atypical features
Management strategies focus on optimizing glycemic control, which remains the most evidence-based intervention for preventing and potentially improving diabetic neuropathy. The American Diabetes Association recommends maintaining individualized A1c targets while avoiding rapid glucose reduction, which may temporarily worsen neuropathic symptoms. Gradual glucose normalization over several months is generally better tolerated than abrupt changes.
For symptom management of neuropathic pain, the American Academy of Neurology and American Diabetes Association guidelines recommend:
First-line: Duloxetine or pregabalin (with appropriate renal dose adjustments)
Alternative options: Gabapentin (with renal dose adjustments) or tricyclic antidepressants (with caution in older adults and cardiac disease)
Topical treatments: Capsaicin 8% patch or lidocaine 5% patch for localized symptoms
Avoid chronic opioid therapy due to limited evidence and safety concerns
Non-pharmacological approaches including physical therapy, proper foot care, and pain psychology techniques provide additional benefit. Neurology referral should be considered for atypical presentations (asymmetry, motor involvement, rapid progression, prominent autonomic features) or treatment-refractory cases. If symptoms are temporally related to semaglutide and persist despite optimization of other factors, healthcare providers may consider dose reduction, temporary treatment interruption, or transition to alternative glucose-lowering therapies.
The most common neurological side effects are headache (8-14% of patients) and dizziness (4-8% of patients), which are typically mild to moderate and often resolve with continued treatment.
Contact your doctor promptly if you experience burning, tingling, or pain triggered by normally non-painful stimuli, especially if symptoms are severe, progressive, or significantly impact daily functioning.
Yes, rapid improvement in glycemic control with any diabetes medication can occasionally trigger treatment-induced neuropathy of diabetes, which presents as acute painful neuropathy and typically improves over time.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.