LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can semaglutide cause colitis? This question concerns patients and clinicians as semaglutide (Ozempic, Wegovy) becomes increasingly prescribed for type 2 diabetes and weight management. While gastrointestinal side effects like nausea and diarrhea are common with this GLP-1 receptor agonist, colitis—inflammation of the colon—has not been established as a recognized adverse effect in FDA labeling or major clinical trials. However, isolated post-marketing reports and theoretical concerns about altered gut motility warrant careful attention. Understanding the distinction between typical medication side effects and potential inflammatory conditions helps patients recognize warning signs requiring medical evaluation.
Quick Answer: Semaglutide has not been established as a cause of colitis in FDA labeling or major clinical trials, though isolated post-marketing reports exist.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes (under the brand name Ozempic) and chronic weight management (as Wegovy). This medication works by mimicking the naturally occurring GLP-1 hormone, which stimulates insulin secretion, suppresses glucagon release, and slows gastric emptying. These mechanisms help lower blood glucose levels and promote satiety, contributing to weight loss.
Gastrointestinal side effects are among the most commonly reported adverse reactions with semaglutide therapy. According to the FDA prescribing information for both Ozempic and Wegovy, nausea, vomiting, diarrhea, abdominal pain, and constipation occur in a significant proportion of patients, particularly during dose escalation. These effects result primarily from the medication's action on GLP-1 receptors throughout the gastrointestinal tract, which influence gut motility and digestive processes.
The delayed gastric emptying caused by semaglutide can lead to feelings of fullness, bloating, and discomfort. While these gastrointestinal symptoms are generally mild to moderate and tend to diminish over time as the body adjusts to treatment, they can occasionally be severe enough to warrant dose adjustment or discontinuation. It's worth noting that semaglutide has not been extensively studied in patients with severe gastrointestinal disease such as severe gastroparesis, and postmarketing reports have included cases of ileus.
The prevalence of gastrointestinal adverse events underscores the importance of patient education before initiating semaglutide therapy, including strategies for minimizing discomfort and recognizing warning signs that merit medical attention.
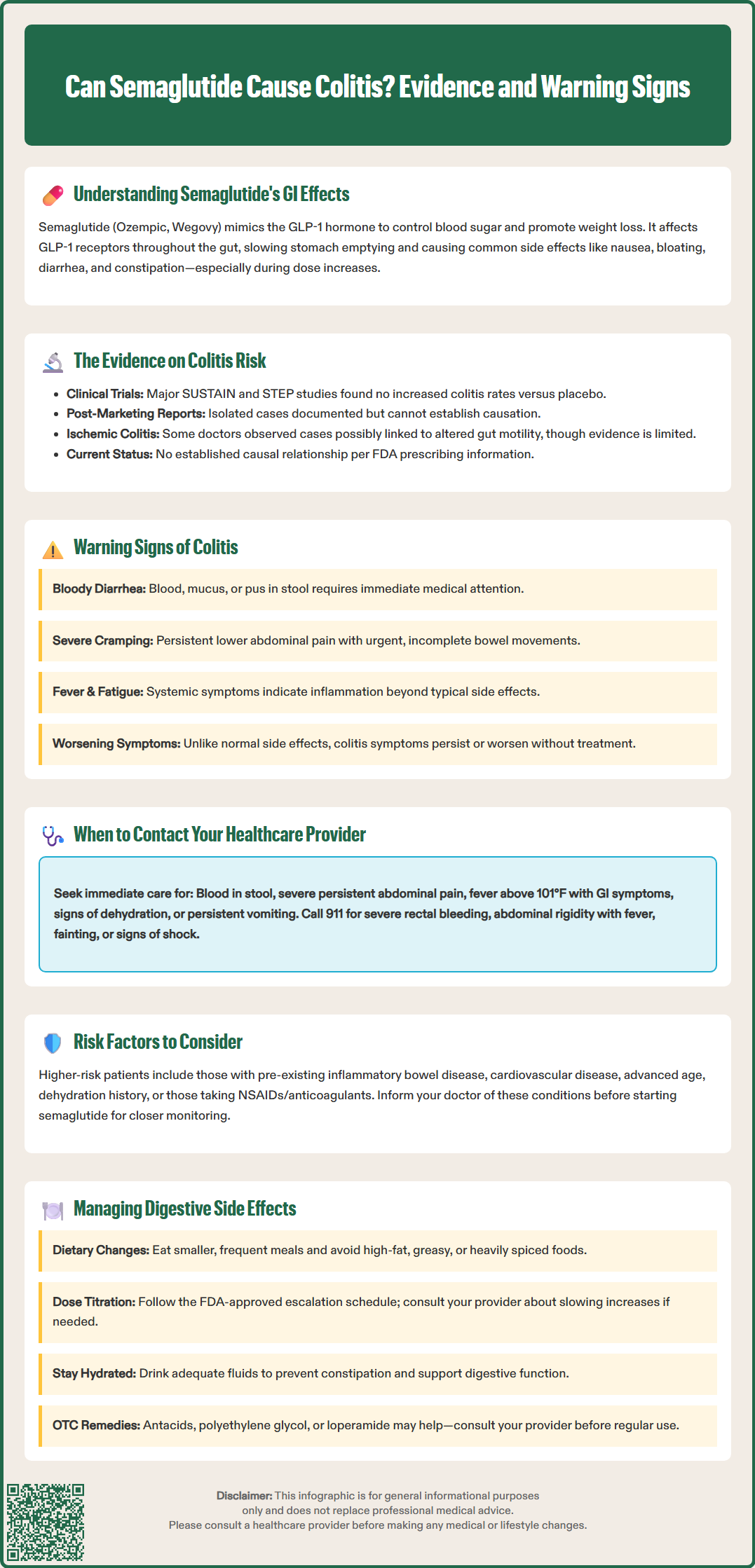
Currently, there is no established causal relationship between semaglutide and colitis in the FDA-approved prescribing information or major clinical trials. Colitis—inflammation of the colon—has not been identified as a recognized adverse effect in the pivotal SUSTAIN trials for diabetes management or the STEP trials for weight management. These large-scale studies, involving thousands of participants, did not report increased rates of colitis compared to placebo groups, though it's important to note that clinical trials may not detect rare adverse events due to sample size limitations.
However, post-marketing surveillance and case reports have documented isolated instances of gastrointestinal inflammatory conditions in patients taking GLP-1 receptor agonists, including semaglutide. The FDA Adverse Event Reporting System (FAERS) contains reports of various gastrointestinal complications, though these reports have significant limitations—including underreporting, lack of denominator data, and inability to establish causality. Spontaneous reporting systems alone cannot definitively determine whether a medication causes a specific adverse event.
Some gastroenterologists have noted reports of ischemic colitis—reduced blood flow to the colon—in patients taking GLP-1 agonists, potentially related to altered gut motility or other mechanisms. Ischemic colitis presents differently from inflammatory colitis but can cause similar symptoms. The theoretical concern centers on whether delayed gastric emptying and altered intestinal transit might predispose susceptible individuals to ischemic events, though this hypothesis lacks robust clinical evidence.
Patients with pre-existing inflammatory bowel disease (IBD), including ulcerative colitis or Crohn's disease, should discuss their condition with their healthcare provider before starting semaglutide. While the medication is not contraindicated in IBD, careful monitoring may be warranted to distinguish disease flares from medication-related effects. The absence of a proven link does not eliminate the need for clinical vigilance when new or worsening gastrointestinal symptoms develop during treatment.
Colitis manifests through several characteristic symptoms that differ in severity and pattern from the common gastrointestinal side effects of semaglutide. Key warning signs of possible colitis include:
Persistent or bloody diarrhea – While diarrhea is a known semaglutide side effect, the presence of blood, mucus, or pus in stool suggests inflammatory or ischemic colitis and requires immediate medical evaluation
Severe abdominal cramping – Intense, persistent cramping pain, particularly in the lower abdomen, that differs from mild discomfort associated with typical medication side effects
Urgent bowel movements – Sudden, uncontrollable urges to defecate, especially if accompanied by inability to empty the bowel completely (tenesmus)
Fever and systemic symptoms – Elevated temperature, chills, fatigue, or malaise accompanying gastrointestinal symptoms may indicate inflammatory processes
Unintended weight loss – Progressive weight loss out of proportion to expected therapeutic effects, particularly when accompanied by decreased appetite and nutritional deficiencies
Severe constipation or abdominal distension – Inability to pass stool or gas, abdominal bloating, or vomiting may indicate ileus or intestinal obstruction requiring urgent evaluation
Distinguishing between common semaglutide-related gastrointestinal effects and potential colitis requires attention to symptom severity, duration, and progression. Typical medication side effects generally improve within several weeks as tolerance develops, whereas colitis symptoms often worsen or persist without treatment. The timing of symptom onset also provides diagnostic clues—while semaglutide side effects typically emerge shortly after initiation or dose increases, colitis can develop at any point during therapy.
Patients should maintain awareness of their bowel patterns and stool characteristics throughout treatment. Any significant change from baseline—particularly the development of bloody stools, nocturnal diarrhea awakening them from sleep, or progressive worsening of symptoms—warrants prompt clinical assessment. Documentation of symptom frequency, severity, and associated factors helps healthcare providers determine whether further investigation is necessary.
Several patient characteristics may increase the risk of gastrointestinal complications, particularly ischemic colitis, though specific risk factors for semaglutide-associated colitis have not been definitively established. Patients with the following conditions should exercise particular caution:
Pre-existing inflammatory bowel disease – History of ulcerative colitis, Crohn's disease, or microscopic colitis
Cardiovascular disease – Atherosclerotic disease or conditions affecting blood flow may increase ischemic colitis risk
Advanced age – Older adults may have reduced intestinal blood flow and increased susceptibility to ischemic events
History of diverticular disease – Pre-existing colonic abnormalities may complicate symptom interpretation
Dehydration or hypotension – Reduced fluid volume may compromise intestinal perfusion
Severe constipation – May increase risk of complications with altered GI motility
Concurrent medications – NSAIDs, anticoagulants, or other drugs affecting gastrointestinal mucosa or blood flow
Contact your healthcare provider immediately if you experience:
Blood in stool or black, tarry stools indicating gastrointestinal bleeding
Severe, persistent abdominal pain unrelieved by usual measures
High fever (temperature above 101°F/38.3°C) with gastrointestinal symptoms
Signs of dehydration—decreased urination, dizziness, extreme thirst, or confusion
Persistent vomiting preventing adequate fluid or medication intake
Sudden worsening of symptoms or new symptoms after stable treatment period
Seek emergency care (call 911 or go to the emergency department) for:
Severe, uncontrolled bleeding from the rectum
Severe abdominal pain with fever and abdominal rigidity/tenderness
Fainting, dizziness, or rapid heart rate with gastrointestinal symptoms
Signs of shock (confusion, cold/clammy skin, very low blood pressure)
Routine follow-up appointments should include discussion of any gastrointestinal symptoms, even if mild. Healthcare providers can assess whether symptoms represent expected medication effects or require diagnostic evaluation such as stool studies, inflammatory markers (C-reactive protein, fecal calprotectin), or colonoscopy. Early identification of serious complications improves outcomes and allows for appropriate treatment modifications.
If you experience severe gastrointestinal symptoms, suspected pancreatitis, or signs of intestinal obstruction/ileus, stop taking semaglutide and seek immediate medical attention. For less severe symptoms, consult your healthcare provider before making any changes to your treatment regimen.
Effective management of gastrointestinal side effects can improve treatment adherence and quality of life during semaglutide therapy. FDA prescribing information and expert consensus support several strategies for minimizing digestive discomfort while maintaining therapeutic efficacy.
Dietary modifications form the cornerstone of symptom management. Patients should consume smaller, more frequent meals rather than large portions, which can overwhelm the delayed gastric emptying caused by semaglutide. Avoiding high-fat, greasy, or heavily spiced foods reduces nausea and abdominal discomfort. Maintaining adequate hydration based on individual needs helps prevent constipation and supports overall digestive function (follow clinician guidance if you have fluid restrictions due to heart failure or kidney disease). Limiting alcohol and caffeine intake may also decrease gastrointestinal irritation.
Dose escalation strategies significantly impact side effect severity. The FDA-approved titration schedule varies by product—Wegovy follows a 16-20 week escalation, while Ozempic has a different schedule. Patients experiencing intolerable symptoms may benefit from slower titration or temporarily maintaining a lower dose before advancing. Never adjust dosing without consulting your healthcare provider, as individualized titration balances efficacy with tolerability.
Timing of administration can influence side effect patterns. Taking semaglutide at a consistent time each week helps patients anticipate and manage symptoms.
Symptomatic relief measures include over-the-counter remedies for specific complaints. Antacids or acid reducers may alleviate heartburn and indigestion. For constipation, gradual fiber introduction, polyethylene glycol laxatives, or stool softeners may help. Anti-diarrheal medications like loperamide can manage loose stools, but should be avoided if you have bloody diarrhea, fever, or suspected infection or ischemia. Always consult your provider before regular use of any over-the-counter remedy.
If gastrointestinal side effects persist despite conservative measures, healthcare providers may consider alternative GLP-1 receptor agonists with different pharmacokinetic profiles, adjust the treatment regimen, or explore complementary therapies for diabetes or weight management. The goal remains achieving therapeutic objectives while maintaining acceptable quality of life and minimizing adverse effects that could compromise long-term adherence.
The most common gastrointestinal side effects of semaglutide include nausea, vomiting, diarrhea, abdominal pain, and constipation, particularly during dose escalation. These effects typically diminish over time as the body adjusts to treatment.
Contact your healthcare provider immediately if you experience blood in stool, severe persistent abdominal pain, high fever with gastrointestinal symptoms, signs of dehydration, or persistent vomiting. Seek emergency care for severe rectal bleeding, abdominal pain with fever and rigidity, or signs of shock.
Semaglutide is not contraindicated in inflammatory bowel disease, but patients with ulcerative colitis or Crohn's disease should discuss their condition with their healthcare provider before starting treatment. Careful monitoring may be warranted to distinguish disease flares from medication-related effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.