LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide (Ozempic, Wegovy) is a GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management. While highly effective for glycemic control and weight loss, clinical trials and FDA labeling indicate an association between semaglutide and acute gallbladder disease, including gallstones (cholelithiasis) and gallbladder inflammation (cholecystitis). This risk appears linked primarily to rapid weight loss rather than direct drug toxicity. Understanding the connection between semaglutide and gallbladder complications, recognizing warning symptoms, and knowing when to seek medical attention are essential for patients and clinicians managing treatment with this medication.
Quick Answer: Semaglutide is associated with increased risk of acute gallbladder disease, including gallstones and cholecystitis, as documented in FDA labeling and clinical trials.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes (under the brand name Ozempic) and chronic weight management (as Wegovy). This medication works by mimicking the natural hormone GLP-1, which plays several important roles in metabolic regulation.
The primary mechanism of action involves stimulating insulin secretion in a glucose-dependent manner, meaning it helps lower blood sugar levels when they are elevated. Semaglutide also suppresses glucagon release, slows gastric emptying, and acts on appetite centers in the brain to promote satiety. These combined effects lead to improved glycemic control in people with diabetes and significant weight reduction in those using it for obesity management.
Clinical trials have demonstrated that semaglutide can reduce hemoglobin A1c by 1.5–2.0% in patients with type 2 diabetes (SUSTAIN clinical trial program) and produce weight loss of 10–15% of body weight over 68 weeks in obesity treatment (STEP clinical trial program). The medication is administered as a once-weekly subcutaneous injection, with doses gradually titrated to minimize gastrointestinal side effects. Ozempic is typically titrated up to 1 mg or 2 mg weekly for diabetes, while Wegovy is titrated to 2.4 mg weekly for weight management.
Common adverse effects include nausea, vomiting, diarrhea, constipation, and abdominal pain, which typically diminish over time as the body adjusts to treatment. More serious but less common concerns have emerged regarding potential effects on various organ systems, including the gallbladder. It's important to note that semaglutide carries a boxed warning about the risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Clinical trial data reveal an increased incidence of gallbladder-related adverse events in patients treated with semaglutide compared to placebo. According to the Wegovy prescribing information, cholelithiasis occurred in approximately 1.6% of semaglutide-treated patients versus 0.7% in placebo groups. Similarly, cholecystitis rates were approximately 0.6% with semaglutide compared to 0.2% with placebo. A 2022 JAMA meta-analysis of GLP-1 receptor agonists confirmed an increased risk of biliary disease with this medication class.
The mechanism underlying this association likely relates primarily to rapid weight loss rather than direct drug toxicity. When individuals lose weight quickly, the liver secretes extra cholesterol into bile while the gallbladder contracts less frequently due to reduced food intake. This combination creates conditions favorable for gallstone formation. Since semaglutide is highly effective at promoting weight loss, patients may be at increased risk through this indirect pathway.
Additionally, GLP-1 receptor agonists may affect gallbladder motility and bile flow patterns through their effects on gastrointestinal motility, though this mechanism requires further investigation. Current evidence suggests that gallbladder complications are associated with both the degree and rate of weight loss as well as possibly direct effects of GLP-1 receptor agonists on biliary function.
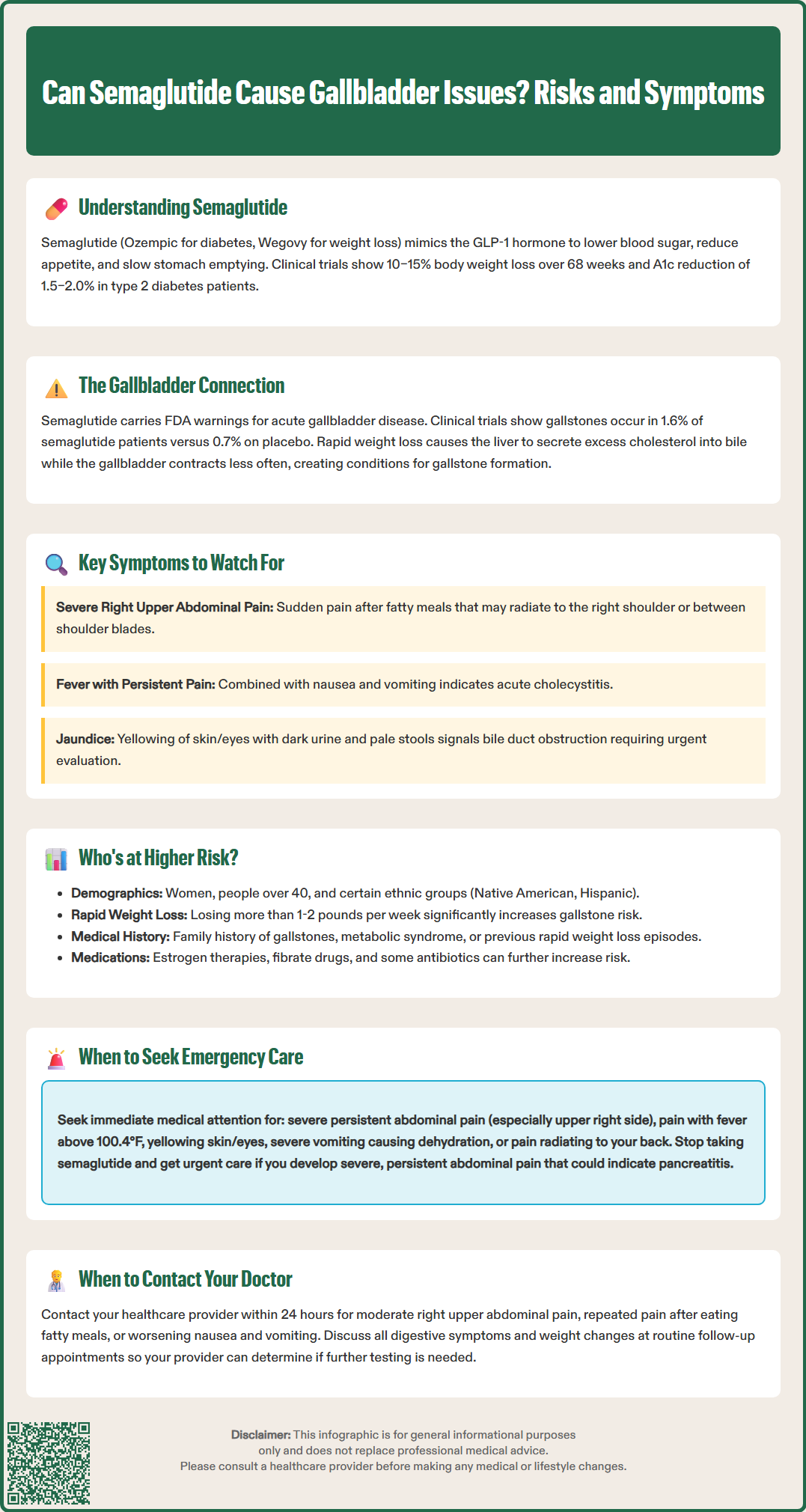
Patients taking semaglutide should be educated about the warning signs of gallbladder disease to enable early detection and appropriate management. The most characteristic symptom of gallbladder problems is biliary colic—sudden, severe pain in the right upper quadrant or epigastric region that may radiate to the right shoulder or between the shoulder blades. This pain typically occurs after meals, particularly those high in fat, and can last from 30 minutes to several hours.
Acute cholecystitis presents with more persistent right upper quadrant pain accompanied by fever, nausea, and vomiting. Patients may notice tenderness when pressure is applied below the right rib cage, and the pain may worsen with deep breathing (Murphy's sign). Jaundice—yellowing of the skin and whites of the eyes—suggests possible bile duct obstruction and requires urgent evaluation. Dark urine and pale or clay-colored stools may accompany jaundice, indicating impaired bile flow.
The combination of fever, jaundice, and right upper quadrant pain (Charcot's triad) may indicate cholangitis, a potentially life-threatening infection of the bile ducts requiring emergency treatment.
It is important to distinguish gallbladder-related pain from the common gastrointestinal side effects of semaglutide. While both can cause abdominal discomfort, typical semaglutide-related symptoms include diffuse abdominal cramping, nausea, and changes in bowel habits that generally improve over time and are not localized to the right upper quadrant. Gallbladder pain tends to be more severe, localized, and episodic rather than constant.
Importantly, if severe, persistent abdominal pain (with or without vomiting) suggests pancreatitis, patients should stop taking semaglutide immediately and seek urgent medical care, as directed in the FDA labeling. Early recognition and appropriate diagnostic workup, typically including right upper quadrant ultrasound and laboratory tests (complete blood count, liver function tests, bilirubin, and lipase), can prevent progression to more serious complications.
Certain patient characteristics and clinical factors increase the likelihood of developing gallbladder problems while taking semaglutide. Understanding these risk factors helps clinicians identify individuals who may benefit from enhanced monitoring or preventive strategies.
Pre-existing risk factors for gallstone disease include:
Female sex: Women are two to three times more likely to develop gallstones than men, particularly during reproductive years due to hormonal influences
Age over 40 years: Gallstone prevalence increases progressively with age
Obesity: Higher body mass index correlates with increased gallstone risk, creating a paradox where the condition being treated is itself a risk factor
Rapid weight loss history: Previous episodes of quick weight reduction may indicate susceptibility
Pregnancy or recent pregnancy: Hormonal changes affect bile composition and gallbladder motility
Family history: Genetic factors contribute to gallstone formation
Certain ethnicities: Native American and Hispanic populations have higher gallstone prevalence
Metabolic syndrome and diabetes: These conditions are associated with altered bile metabolism
The rate and magnitude of weight loss during semaglutide treatment significantly influence gallbladder complication risk. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), gradual weight loss (about 1-2 pounds per week) is recommended to reduce gallstone risk. Patients losing weight very rapidly face higher risk than those with more gradual weight reduction. Starting at higher body weights and achieving greater total weight loss percentages also correlates with increased gallbladder event rates.
Other medications may compound risk, including estrogen-containing hormonal therapies, fibrate lipid-lowering drugs, and certain antibiotics like ceftriaxone. Patients with pre-existing gallbladder sludge or small asymptomatic gallstones detected on imaging may be at higher risk for progression to symptomatic disease during treatment.
Clinicians should conduct thorough baseline assessments including detailed medical and family histories before initiating semaglutide. While routine screening ultrasound is not recommended for asymptomatic patients, those with multiple risk factors warrant counseling about symptoms and potentially closer monitoring. Ursodeoxycholic acid therapy has shown benefit for gallstone prevention during rapid weight loss after bariatric surgery, but there is currently insufficient evidence to support its routine use in patients taking semaglutide.
Patients taking semaglutide should understand which symptoms require immediate medical attention versus those that can be addressed at routine follow-up appointments. Clear communication guidelines help ensure timely intervention when necessary while avoiding unnecessary emergency visits for expected medication side effects.
Seek immediate medical care (emergency department or urgent care) if you experience:
Severe, persistent abdominal pain, especially in the right upper quadrant, lasting more than a few hours
Abdominal pain accompanied by fever (temperature above 100.4°F or 38°C)
Yellowing of the skin or eyes (jaundice)
Severe nausea and vomiting preventing fluid intake and leading to dehydration
Dark urine combined with pale stools
Abdominal pain radiating to the back, which could indicate pancreatitis
The combination of fever, jaundice, and abdominal pain, which may indicate cholangitis (bile duct infection)
Confusion, extreme weakness, or very low blood pressure with any of the above symptoms (possible signs of sepsis)
Important: If you experience severe, persistent abdominal pain with or without vomiting that could be consistent with pancreatitis, stop taking semaglutide immediately and seek urgent medical care, as directed in the FDA labeling.
Contact your healthcare provider within 24 hours for:
New or worsening abdominal pain that is moderate in severity and localized to the right upper abdomen
Recurrent episodes of pain after eating, particularly fatty meals
Persistent nausea or vomiting that is worsening rather than improving over time
Any abdominal symptoms that concern you or differ from your usual experience with the medication
Routine follow-up appointments should include discussion of any gastrointestinal symptoms, weight loss patterns, and overall tolerance of the medication. Your healthcare provider will assess whether symptoms represent expected side effects or warrant further investigation with laboratory tests or imaging studies.
If gallbladder disease is diagnosed, management depends on severity and may range from conservative observation for asymptomatic gallstones to cholecystectomy (surgical gallbladder removal) for acute cholecystitis or symptomatic cholelithiasis. Your provider will discuss whether to continue, adjust, or discontinue semaglutide based on individual circumstances. The decision to resume semaglutide after cholecystectomy should be individualized and made in consultation with your healthcare provider, particularly if you experienced complications such as gallstone pancreatitis. Maintaining open communication with your healthcare team throughout treatment optimizes both safety and therapeutic outcomes.
Warning signs include severe right upper quadrant pain (especially after meals), fever, jaundice (yellowing of skin or eyes), persistent nausea and vomiting, and dark urine with pale stools. Seek immediate medical care if you experience these symptoms, particularly the combination of fever, jaundice, and abdominal pain.
The increased risk relates primarily to rapid weight loss, which causes the liver to secrete extra cholesterol into bile while the gallbladder contracts less frequently. This combination creates favorable conditions for gallstone formation.
If you experience severe, persistent abdominal pain that could indicate gallbladder disease or pancreatitis, stop semaglutide immediately and seek urgent medical care as directed in FDA labeling. Your healthcare provider will determine whether to resume treatment based on your individual circumstances and diagnosis.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.