LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide cause gallstones? This question concerns many patients considering or currently using this GLP-1 receptor agonist for diabetes management or weight loss. Clinical evidence indicates that semaglutide is associated with an increased risk of gallstone formation and related gallbladder complications. Understanding this connection, recognizing warning signs, and implementing preventive strategies can help patients and healthcare providers make informed treatment decisions. This article examines the relationship between semaglutide and gallbladder disease, explores underlying mechanisms, identifies risk factors, and provides practical guidance for minimizing complications during treatment.
Quick Answer: Semaglutide is associated with an increased risk of gallstone formation, with clinical trials showing cholelithiasis occurring in approximately 1.6% of treated patients compared to 0.7% receiving placebo.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes (under the brand name Ozempic) and chronic weight management (as Wegovy). This medication works by mimicking the natural hormone GLP-1, which plays several important roles in metabolic regulation.
The primary mechanisms of action include stimulating insulin secretion in response to elevated blood glucose levels, suppressing glucagon release when blood sugar is high, and slowing gastric emptying. These effects help improve glycemic control in people with diabetes. Additionally, semaglutide acts on appetite centers in the brain, reducing hunger and promoting satiety, which contributes to significant weight loss in many patients.
Clinical trials have demonstrated that semaglutide can lead to substantial weight reduction. In the STEP 1 trial published in the New England Journal of Medicine, patients receiving semaglutide 2.4 mg weekly plus lifestyle intervention lost an average of approximately 15% of their body weight over 68 weeks. This degree of weight loss, while beneficial for metabolic health and cardiovascular risk reduction, can have secondary effects on various body systems.
The medication is administered as a once-weekly subcutaneous injection, with dosing gradually increased to minimize gastrointestinal side effects. Ozempic (for diabetes) typically follows a 4-week titration schedule, while Wegovy (for weight management) uses a more gradual 16-20 week titration approach.
Common adverse effects include nausea, vomiting, diarrhea, constipation, and abdominal pain, which typically improve over time as the body adjusts to treatment. Understanding how semaglutide affects metabolism and body composition is essential for recognizing potential complications, including those affecting the gallbladder and biliary system.
Research indicates that semaglutide use is associated with an increased risk of gallbladder-related complications, including gallstone formation (cholelithiasis) and inflammation of the gallbladder (cholecystitis). This relationship appears to be partly mediated by rapid weight loss, though direct effects on gallbladder motility may also play a role.
Clinical trial data for semaglutide has documented this risk. According to the FDA prescribing information for Wegovy, in the STEP clinical trials, cholelithiasis was reported in approximately 1.6% of semaglutide-treated patients compared to 0.7% of placebo recipients. Overall gallbladder-related adverse events occurred in 2.6% of semaglutide patients versus 1.2% with placebo, and acute cholecystitis in 0.6% versus 0.2%, respectively. Notably, this increased risk persisted even after adjusting for the magnitude of weight loss.
A 2022 systematic review and meta-analysis published in JAMA Internal Medicine found that GLP-1 receptor agonists as a class were associated with increased biliary disease risk. The analysis suggested higher risk with weight-management doses and longer treatment duration compared to lower doses used for diabetes management.
The FDA label for both Ozempic and Wegovy includes warnings about acute gallbladder disease. Patients should be informed of this risk and the characteristic symptoms that warrant medical attention.
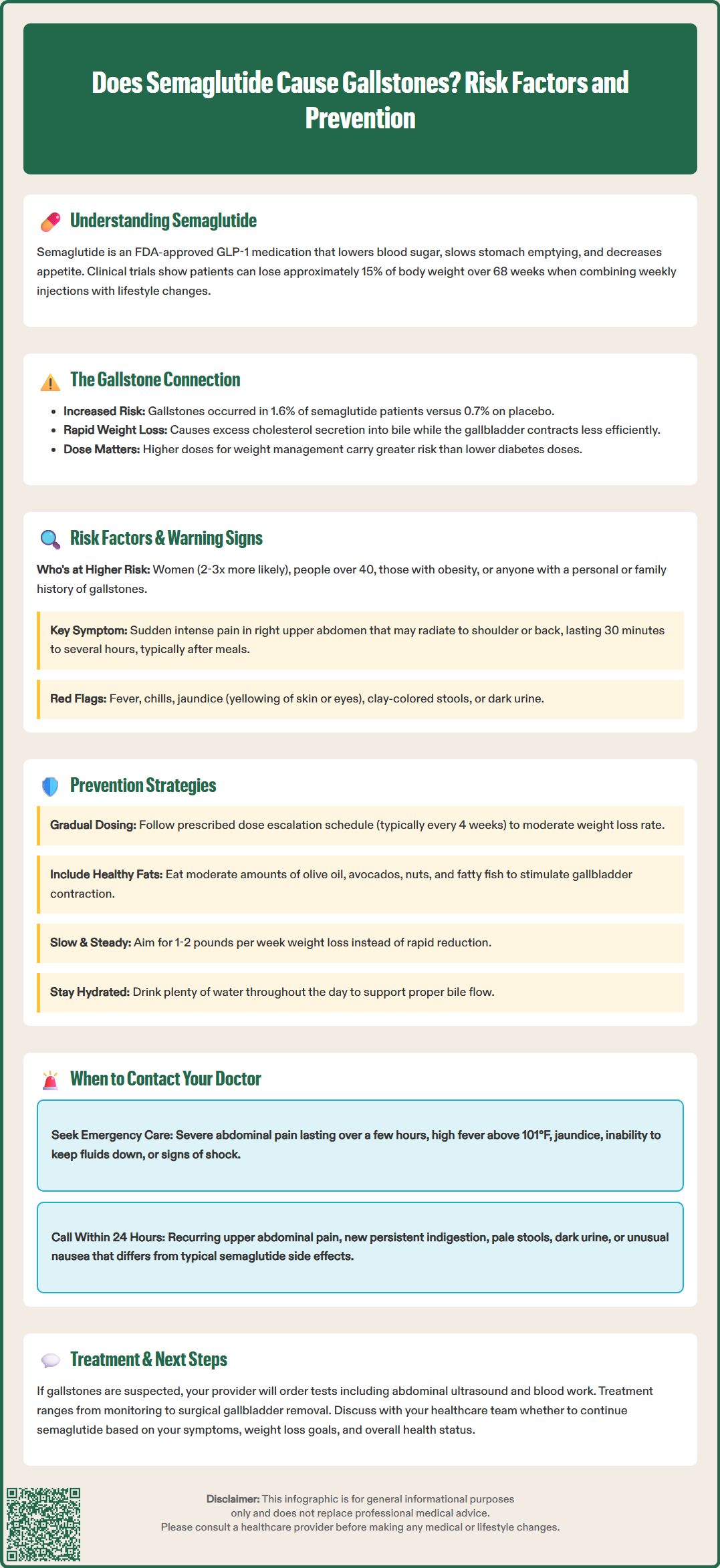
Certain patient characteristics increase the likelihood of developing gallstones while taking semaglutide. Understanding these risk factors helps clinicians identify individuals who may benefit from closer monitoring or preventive strategies.
Key risk factors include:
Rapid weight loss: Losing weight quickly significantly increases gallstone risk
Female sex: Women are two to three times more likely to develop gallstones than men
Age over 40 years: Gallstone prevalence increases with age
Obesity: Higher baseline BMI correlates with increased risk
Previous history of gallstones: Prior biliary disease predicts recurrence
Family history: Genetic factors contribute to gallstone susceptibility
Certain ethnicities: Native American and Hispanic populations have higher baseline rates
Estrogen exposure: Oral contraceptives, hormone replacement therapy, and multiple pregnancies
Diabetes and dyslipidemia: Metabolic conditions affecting bile composition
Prolonged fasting or TPN use: Reduces gallbladder contraction
Patients should be educated about warning signs that may indicate gallstone complications. Classic symptoms include:
Sudden, intense pain in the right upper abdomen or center of the abdomen, often radiating to the right shoulder or back
Pain episodes (biliary colic) lasting 30 minutes to several hours, typically occurring after meals
Nausea and vomiting accompanying abdominal pain
Fever and chills, which may indicate cholecystitis or infection
Jaundice (yellowing of skin or eyes), suggesting bile duct obstruction
Clay-colored stools or dark urine
Persistent indigestion or bloating
It is important to note that many gallstones remain asymptomatic and are discovered incidentally on imaging performed for other reasons. Additionally, some gallbladder symptoms may overlap with common semaglutide side effects, potentially delaying recognition. Patients should maintain a low threshold for reporting new or different right upper quadrant pain to their healthcare provider.
Symptomatic gallstones require medical evaluation, as complications such as acute cholecystitis, choledocholithiasis, or pancreatitis can develop and may necessitate surgical intervention.
While the risk of gallstone formation cannot be entirely eliminated, several strategies may help reduce the likelihood of developing gallbladder complications during semaglutide treatment.
Gradual dose escalation is built into semaglutide prescribing guidelines and serves multiple purposes. Starting at lower doses and slowly increasing helps minimize gastrointestinal side effects and may moderate the rate of weight loss, potentially reducing gallstone risk. For Ozempic, doses typically increase every 4 weeks as needed for glycemic control. For Wegovy, the titration extends over at least 16 weeks, with 4-week intervals between dose increases. Patients should follow the prescribed titration schedule rather than advancing doses more quickly.
Maintaining adequate dietary fat intake may be beneficial. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), consuming moderate amounts of healthy fats with meals stimulates gallbladder contraction and bile flow, potentially preventing bile stasis. Very low-fat diets may paradoxically increase gallstone risk by allowing bile to become concentrated in a poorly contracting gallbladder. Patients should aim for balanced meals including sources of unsaturated fats such as olive oil, avocados, nuts, and fatty fish.
Gradual, sustainable weight loss is preferable to rapid reduction. While semaglutide is highly effective for weight loss, aiming for 1-2 pounds per week rather than more aggressive reduction may lower gallstone risk. This can be achieved through appropriate dose management and lifestyle modifications.
Adequate hydration supports overall metabolic function and may help maintain proper bile flow. Patients should consume sufficient water throughout the day.
For patients at particularly high risk, some clinicians consider ursodeoxycholic acid (UDCA) prophylaxis. This bile acid medication can reduce cholesterol saturation in bile and has been shown in studies of bariatric surgery and very low calorie diets to decrease gallstone formation during rapid weight loss. However, this approach is not FDA-approved specifically for semaglutide-induced weight loss, is not routinely recommended for all patients, and should be discussed with a healthcare provider on an individual basis after shared decision-making. The typical prophylactic dose studied in rapid weight loss settings is 300 mg twice daily for up to 6 months.
Regular follow-up appointments allow for monitoring of weight loss velocity and assessment of any developing symptoms. Patients should maintain open communication with their healthcare team about any abdominal symptoms or concerns.
Patients taking semaglutide should understand when gallbladder-related symptoms require medical attention. Prompt evaluation can prevent serious complications and guide appropriate management decisions.
Seek immediate medical attention (emergency department or call 911) if you experience:
Severe, persistent abdominal pain lasting more than a few hours, particularly in the right upper quadrant
Abdominal pain accompanied by high fever (temperature above 101°F or 38.3°C)
Jaundice (yellowing of the skin or whites of the eyes)
Severe nausea and vomiting preventing fluid intake
Abdominal pain with confusion, rapid heartbeat, or signs of shock
These symptoms may indicate acute cholecystitis, choledocholithiasis with cholangitis, or gallstone pancreatitis—conditions requiring urgent evaluation and treatment. If pancreatitis is suspected, semaglutide should be discontinued immediately per FDA guidance.
Contact your healthcare provider within 24 hours for:
Recurrent episodes of right upper abdominal pain, even if they resolve
Persistent indigestion or bloating that is new or worsening
Changes in stool color (pale or clay-colored) or dark urine
Unexplained nausea that differs from typical semaglutide side effects
Any abdominal pain that concerns you or interferes with daily activities
Your provider may order diagnostic tests including abdominal ultrasound (the first-line imaging for gallstones), liver function tests, complete blood count, and lipase levels if pancreatitis is suspected. If gallstones are confirmed and symptomatic, treatment options range from conservative management to cholecystectomy (surgical gallbladder removal), depending on symptom severity and complication risk.
Referral pathways typically include general surgery consultation for symptomatic gallstones or cholecystitis, while suspected bile duct stones (choledocholithiasis) or cholangitis may require gastroenterology evaluation for possible endoscopic retrograde cholangiopancreatography (ERCP).
Patients with documented gallstones should discuss with their healthcare team whether to continue semaglutide, as the decision depends on individual circumstances including symptom severity, weight loss goals, glycemic control needs, and surgical candidacy. In some cases, temporary discontinuation may be appropriate while addressing gallbladder issues.
Regular monitoring visits should include discussion of any new abdominal symptoms, even if mild, as early detection of gallbladder problems allows for more treatment options and better outcomes.
In clinical trials, gallstones occurred in approximately 1.6% of semaglutide-treated patients compared to 0.7% of placebo recipients. Overall gallbladder-related adverse events occurred in 2.6% of semaglutide patients versus 1.2% with placebo.
Warning signs include sudden, intense pain in the right upper abdomen or center of the abdomen that may radiate to the right shoulder or back, nausea and vomiting with abdominal pain, fever and chills, jaundice, or clay-colored stools. Seek immediate medical attention if these symptoms occur.
While gallstone risk cannot be entirely eliminated, strategies that may help include following the prescribed gradual dose titration schedule, maintaining adequate dietary fat intake with meals, aiming for gradual rather than rapid weight loss, and attending regular follow-up appointments for symptom monitoring.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.