LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro) have raised important questions about reproductive health. These glucagon-like peptide-1 (GLP-1) receptor agonists are FDA-approved for chronic weight management and type 2 diabetes, but their effects on fertility require careful consideration. While these medications don't directly impair fertility, they can actually improve conception potential through metabolic optimization—particularly in individuals with obesity-related reproductive dysfunction. However, pregnancy during treatment poses safety concerns, making proper planning essential for anyone considering conception. Understanding the relationship between these medications and fertility helps patients and healthcare providers make informed decisions about weight management and family planning.
Quick Answer: Weight loss injections do not directly impair fertility and may improve conception potential through metabolic optimization, but require discontinuation before planned pregnancy due to potential fetal risks.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and tirzepatide (Zepbound), work through multiple physiological mechanisms to promote weight reduction. Wegovy and Zepbound are FDA-approved for chronic weight management, while Ozempic (semaglutide) and Mounjaro (tirzepatide) are approved for type 2 diabetes management.
These medications mimic naturally occurring incretin hormones that regulate glucose metabolism and appetite control. The primary mechanism involves binding to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract. In the pancreas, these agents enhance glucose-dependent insulin secretion while suppressing glucagon release, leading to improved glycemic control. Centrally, GLP-1 receptor agonists act on hypothalamic appetite centers to increase satiety and reduce food intake. Additionally, these medications slow gastric emptying, prolonging the sensation of fullness after meals and reducing overall caloric consumption.
Tirzepatide offers dual agonist activity, targeting both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors, which may contribute to its enhanced weight loss efficacy compared to single-receptor agonists. Clinical trials demonstrate average weight reductions of approximately 15% with semaglutide 2.4 mg (STEP 1 trial) and 20-22.5% with tirzepatide 10-15 mg (SURMOUNT-1 trial) over 68-72 weeks.
Beyond weight loss, these medications improve multiple metabolic parameters including hemoglobin A1c, blood pressure, and lipid profiles. Important safety considerations include contraindications for patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. The systemic effects extend to various organ systems, raising important questions about their impact on reproductive function.
The relationship between weight loss injections and fertility is complex and primarily indirect. In women, obesity itself is a significant risk factor for infertility, contributing to anovulation, polycystic ovary syndrome (PCOS), and menstrual irregularities. Weight loss achieved through any means—including GLP-1 receptor agonists—can restore ovulatory function and improve fertility outcomes in women with obesity-related reproductive dysfunction.
Clinical observations suggest that women using weight loss injections may experience restoration of regular menstrual cycles and improved ovulation rates as metabolic parameters normalize, though individual responses vary considerably and timing is unpredictable. For women with PCOS, weight reduction of 5-10% can significantly improve insulin sensitivity, reduce hyperandrogenism, and restore ovulatory cycles. However, this enhanced fertility creates an important safety consideration, as these medications are not recommended during pregnancy.
In men, obesity negatively affects fertility through multiple mechanisms including reduced testosterone levels, impaired spermatogenesis, and erectile dysfunction. Weight loss can improve these parameters, potentially enhancing male fertility. Limited data exist specifically examining GLP-1 receptor agonist effects on male reproductive function, though improvements in metabolic health would theoretically benefit fertility. No paternal washout period is generally recommended, as there is no known male-mediated teratogenic risk.
There is limited human evidence regarding direct effects of GLP-1 receptor agonists on fertility in either sex. The primary concern relates to inadvertent pregnancy exposure rather than reduced conception rates. Animal studies have shown potential fetal risks, making pregnancy avoidance during treatment essential. The FDA labels for these medications emphasize discontinuation before planned conception.
Individuals experiencing infertility should seek evaluation after 12 months of trying to conceive if under 35 years of age, or after 6 months if 35 or older. Persistent amenorrhea (absence of menstruation for more than 3 months) warrants medical evaluation regardless of fertility goals.
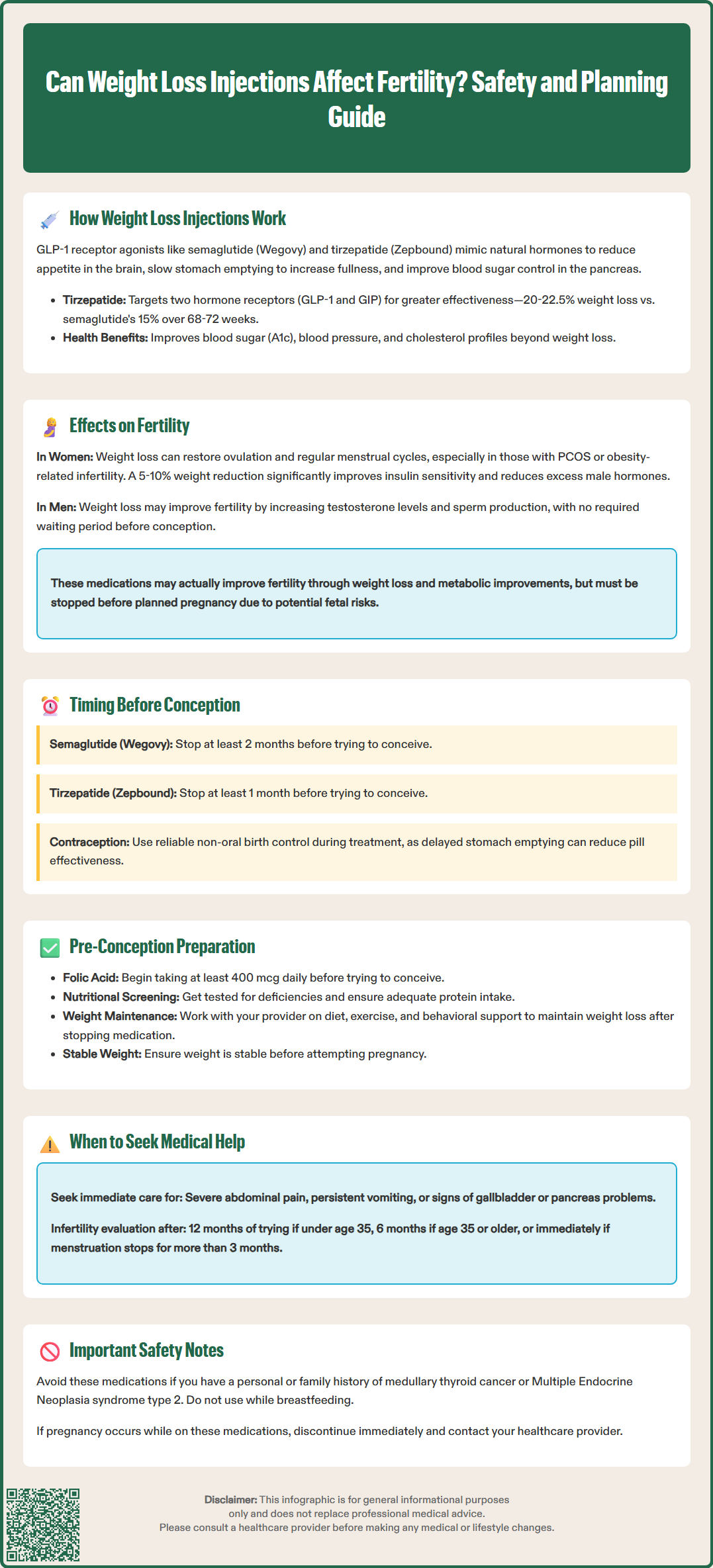
Individuals planning pregnancy should discontinue weight loss injections well in advance of conception attempts. Current FDA guidance recommends stopping semaglutide (Wegovy, Ozempic) at least two months before planned pregnancy, based on the medication's elimination half-life of approximately one week. For tirzepatide (Zepbound, Mounjaro), FDA labeling advises discontinuation at least one month before planned pregnancy, reflecting its half-life of approximately five days.
Preconception counseling should address several key considerations. First, effective contraception is essential during treatment with GLP-1 receptor agonists. For tirzepatide specifically, the FDA label warns that delayed gastric emptying may reduce oral contraceptive effectiveness. Non-oral contraception or backup contraceptive methods are recommended for 4 weeks after initiation and with each dose increase. If pregnancy is recognized during treatment, the medication should be discontinued immediately and the healthcare provider contacted promptly.
The timing of discontinuation should balance two competing considerations: allowing adequate medication clearance while maintaining the metabolic benefits achieved through weight loss. Rapid weight regain after stopping these medications can occur, potentially negating fertility improvements. Healthcare providers should develop individualized plans that may include transitioning to lifestyle modifications, nutritional counseling, and behavioral support to maintain weight loss.
Additional preconception optimization includes folic acid supplementation (at least 400 mcg daily per CDC recommendations), screening for nutritional deficiencies that may have developed during rapid weight loss, and ensuring adequate protein intake. Women should achieve stable weight and optimized metabolic parameters before conception attempts.
These medications are not recommended during breastfeeding. Patients should be alert to warning signs requiring urgent medical attention, including severe abdominal pain (especially if radiating to the back), persistent vomiting, or signs of gallbladder disease or pancreatitis. Consultation with reproductive endocrinology specialists may benefit individuals with complex fertility issues or significant obesity-related comorbidities.
The direct answer is nuanced: weight loss injections do not appear to impair fertility and may actually improve fertility potential through metabolic improvements, but they require careful management in the preconception period. The primary effect on fertility is indirect and generally positive, resulting from weight reduction and metabolic optimization rather than direct reproductive toxicity.
For women with obesity-related infertility, particularly those with PCOS or anovulation, the weight loss achieved with GLP-1 receptor agonists can restore reproductive function. Studies examining bariatric interventions consistently demonstrate improved fertility outcomes with significant weight reduction. While specific prospective trials examining fertility outcomes with GLP-1 receptor agonists are limited, the metabolic improvements observed—including enhanced insulin sensitivity, reduced inflammation, and hormonal normalization—would theoretically support improved fertility.
The critical safety concern is not reduced fertility but rather the potential for pregnancy during treatment. Animal reproduction studies have demonstrated fetal risks including structural abnormalities and growth restriction. Human data on pregnancy outcomes following prior use of these medications remain limited, emphasizing the importance of following recommended washout periods. These medications are contraindicated during pregnancy and offer no benefit during pregnancy.
Healthcare providers should counsel patients that fertility may improve during treatment, emphasizing the importance of reliable contraception. For individuals actively trying to conceive, discontinuation with appropriate washout periods is essential. The decision to use these medications should consider reproductive timeline, with those planning near-term pregnancy potentially benefiting from alternative weight loss strategies.
If pregnancy occurs during treatment, the medication should be stopped immediately and healthcare providers notified. Individuals should plan weight management therapy around their reproductive goals, with appropriate timing of discontinuation before conception attempts. Consultation with specialists in reproductive endocrinology may be beneficial for those with complex fertility concerns.
The FDA recommends discontinuing semaglutide (Wegovy, Ozempic) at least two months before planned pregnancy and tirzepatide (Zepbound, Mounjaro) at least one month before conception attempts. These washout periods are based on the medications' elimination half-lives and allow adequate clearance from the body.
Yes, weight loss achieved with GLP-1 receptor agonists can improve fertility in women with polycystic ovary syndrome (PCOS) by enhancing insulin sensitivity, reducing hyperandrogenism, and restoring ovulatory cycles. Weight reduction of 5-10% can significantly improve reproductive function in women with obesity-related infertility.
If pregnancy occurs during treatment with weight loss injections, discontinue the medication immediately and contact your healthcare provider promptly. These medications are contraindicated during pregnancy due to potential fetal risks demonstrated in animal studies, and your provider will guide appropriate prenatal care.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.