LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can I ask my doctor for weight loss injections? Absolutely—and you should if you're struggling with weight management despite lifestyle efforts. Weight loss injections like semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound) are FDA-approved medications for obesity treatment. These GLP-1 and dual GIP/GLP-1 receptor agonists work by reducing appetite, slowing digestion, and improving metabolic function. Qualification typically requires a BMI of 30 or higher, or 27 or higher with weight-related conditions like type 2 diabetes or hypertension. Discussing these options with your physician is a medically appropriate step toward addressing obesity as the chronic disease it is.
Quick Answer: Yes, you can and should ask your doctor about weight loss injections if you meet FDA criteria: BMI 30 or higher, or BMI 27 or higher with weight-related conditions.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections represent a significant advancement in obesity medicine, utilizing medications from two main classes: glucagon-like peptide-1 (GLP-1) receptor agonists and dual GIP/GLP-1 receptor agonists. These FDA-approved medications include semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound), which work through multiple physiological mechanisms to promote weight reduction.
These medications function by mimicking naturally occurring hormones that regulate appetite and glucose metabolism. They slow gastric emptying, meaning food remains in the stomach longer, creating prolonged feelings of fullness. They also act on appetite centers in the brain, specifically the hypothalamus, reducing hunger signals and food cravings. Additionally, these medications enhance glucose-dependent insulin secretion and reduce glucagon, which can benefit individuals with prediabetes or type 2 diabetes.
Clinical trials have demonstrated substantial weight loss outcomes. Semaglutide 2.4 mg weekly has shown average weight reductions of approximately 15% of body weight over 68 weeks, while tirzepatide has demonstrated even greater efficacy with losses up to 20-21% in some studies. These results significantly exceed those achieved with older weight loss medications, though they generally remain below the 25-35% typically seen with bariatric surgery.
The injections are administered subcutaneously, with Wegovy and Zepbound given weekly and Saxenda administered daily, using pre-filled pens similar to insulin delivery devices. Treatment requires ongoing use, as discontinuation generally results in weight regain. Common adverse effects include nausea, vomiting, diarrhea, and constipation, which are usually mild to moderate and often diminish over time with dose titration. More serious but rare risks include pancreatitis, gallbladder disease, intestinal obstruction, acute kidney injury from dehydration, and potential thyroid concerns. Patients taking insulin or sulfonylureas may experience hypoglycemia. These medications also carry warnings about suicidal thoughts and behaviors, necessitating careful patient selection and monitoring.
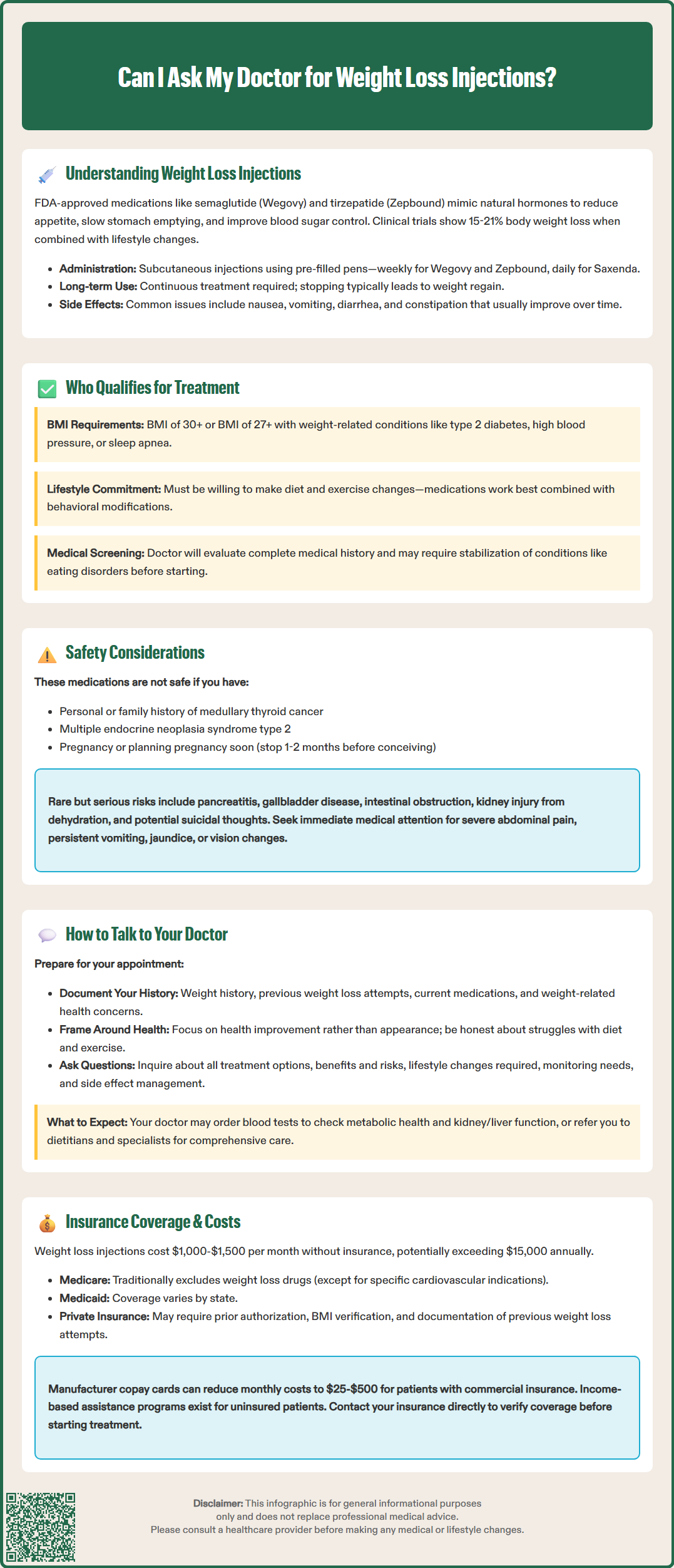
The FDA has established specific criteria for prescribing weight loss injections, based on body mass index (BMI) and the presence of weight-related health conditions. Understanding these qualification standards helps patients determine whether they might be appropriate candidates for this treatment approach.
Standard qualification criteria include:
BMI ≥30 kg/m² (obesity) regardless of comorbidities
BMI ≥27 kg/m² (overweight) with at least one weight-related condition such as type 2 diabetes, hypertension, dyslipidemia, obstructive sleep apnea, or cardiovascular disease
Age 18 years or older (Wegovy and Saxenda are also approved for adolescents aged 12 and above; Zepbound is approved for adults only)
Previous unsuccessful attempts at weight loss through lifestyle modification
Certain medical conditions may preclude the use of weight loss injections. Contraindications and precautions include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, history of pancreatitis (requires careful consideration), severe gastrointestinal disease, diabetic retinopathy (requires caution), and pregnancy or planned pregnancy. Women of childbearing potential should use effective contraception during treatment. Discontinuation timing before attempting conception varies by medication: at least two months for semaglutide and at least one month for tirzepatide. Notably, tirzepatide may reduce the effectiveness of oral contraceptives during initiation and dose escalation, so backup contraception is advised during these periods. These medications are not recommended during breastfeeding.
Physicians also consider overall health status, medication adherence history, and realistic treatment expectations. Candidates should be willing to engage in concurrent lifestyle modifications, including dietary changes and increased physical activity, as medications work most effectively when combined with behavioral interventions. Patients with active substance use disorders, untreated eating disorders, or severe psychiatric conditions may require stabilization of these conditions before initiating weight loss pharmacotherapy. Your healthcare provider will conduct a comprehensive evaluation including medical history, physical examination, and relevant laboratory tests (such as renal and liver function, A1c/glucose, lipids, and pregnancy testing when applicable) to determine appropriateness for treatment.
Initiating a conversation about weight loss injections with your physician requires preparation and openness. Many patients feel hesitant discussing weight concerns, but healthcare providers recognize obesity as a chronic medical condition requiring clinical management, not a personal failing.
Prepare for your appointment by:
Documenting your weight history, including previous weight loss attempts, diets tried, exercise programs, and any medications used
Listing current medications, supplements, and medical conditions
Recording weight-related health concerns such as joint pain, sleep problems, or mobility limitations
Writing down specific questions about treatment options, risks, and expected outcomes
Bringing recent laboratory results if available
During the consultation, be honest about your struggles with weight management and your treatment goals. Frame the conversation around health improvement rather than appearance alone. You might say, "I've tried multiple approaches to lose weight, including diet and exercise, but haven't achieved lasting results. I'm concerned about my health risks and would like to discuss medical treatment options, including weight loss injections."
Ask your physician to explain all available treatment options, not just medications. This demonstrates your commitment to comprehensive care. Important questions include: What are the potential benefits and risks? How long would I need to take this medication? What lifestyle changes should accompany treatment? What monitoring will be required? What happens if I experience side effects?
Your doctor may recommend additional evaluations before prescribing, such as blood tests to assess metabolic health, liver and kidney function. They might also refer you to a registered dietitian, exercise physiologist, or behavioral health specialist as part of a multidisciplinary approach. For patients with BMI ≥40 or ≥35 with obesity-related conditions, bariatric surgery may be discussed as an alternative or future option if medications prove insufficient.
Be aware of red flag symptoms that require immediate medical attention while on these medications: severe or persistent abdominal pain, persistent vomiting/dehydration, jaundice, severe constipation or abdominal distention, vision changes, or signs of hypoglycemia.
If your physician seems dismissive or uncomfortable discussing weight management, seeking a second opinion or consulting an obesity medicine specialist is entirely appropriate. You can find board-certified obesity medicine physicians through the American Board of Obesity Medicine directory.
The financial aspect of weight loss injections represents a significant consideration, as these medications carry substantial costs and insurance coverage remains inconsistent across plans and states.
Cost considerations without insurance (as of 2025):
Wegovy (semaglutide): approximately $1,300-$1,500 per month
Saxenda (liraglutide): approximately $1,300-$1,400 per month
Zepbound (tirzepatide): approximately $1,000-$1,200 per month
These prices reflect list prices; actual costs vary by pharmacy and available discounts. Treatment typically continues for at least one year, often longer, making annual costs potentially exceed $15,000 without coverage.
Insurance coverage varies significantly. Medicare Part D plans traditionally excluded weight loss medications by statute, though Wegovy may now be covered for its cardiovascular risk reduction indication in adults with established cardiovascular disease and overweight/obesity. The Treat and Reduce Obesity Act, if passed, would expand Medicare coverage for obesity medications. Medicaid coverage depends on individual state policies, with some states providing coverage while others explicitly exclude weight loss medications. Private insurance coverage is highly variable—some plans cover these medications with prior authorization, while others exclude them entirely or cover them only for diabetes management (at lower doses than used for weight loss).
To navigate coverage, contact your insurance company directly to verify formulary status and requirements. Many insurers require documentation of previous weight loss attempts, BMI verification, and presence of comorbidities. Prior authorization typically takes 1-3 weeks. If denied, appeals are possible with supporting documentation from your physician.
Manufacturer savings programs can significantly reduce out-of-pocket costs for eligible patients with commercial insurance. Novo Nordisk and Eli Lilly offer copay cards that may reduce monthly costs to $25-$500, depending on insurance status. Uninsured patients may qualify for patient assistance programs based on income.
Some compounding pharmacies offer lower-cost versions of these medications, but the FDA has issued safety warnings about compounded GLP-1 products. These compounded versions lack FDA approval, may contain different salt forms or ingredients than the approved products, and have been associated with adverse events. Discuss all financial options with your healthcare provider and pharmacist to identify the most affordable approach for your situation.
Bring documentation of your weight history, previous weight loss attempts, current medications and medical conditions, recent laboratory results if available, and a list of specific questions about treatment options and expected outcomes.
Without insurance, Wegovy costs approximately $1,300-$1,500 monthly, Saxenda $1,300-$1,400 monthly, and Zepbound $1,000-$1,200 monthly. Manufacturer savings programs and patient assistance programs may reduce costs for eligible patients.
Common side effects include nausea, vomiting, diarrhea, and constipation, which typically diminish with dose adjustment. Serious but rare risks include pancreatitis, gallbladder disease, intestinal obstruction, and acute kidney injury from dehydration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.