LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections, including GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro), have revolutionized obesity management. While these medications offer significant metabolic benefits, questions about their impact on kidney health are common among patients and clinicians. Understanding whether weight loss injections can cause kidney problems requires examining clinical trial data, FDA safety warnings, and the mechanisms by which these medications might affect renal function. This article explores the evidence on kidney safety, identifies risk factors, and provides practical guidance for protecting kidney health during treatment with these increasingly prescribed medications.
Quick Answer: Weight loss injections like semaglutide and tirzepatide rarely cause direct kidney damage, but can lead to acute kidney injury through dehydration from gastrointestinal side effects rather than direct toxicity.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections have transformed obesity management in recent years. These include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro), which is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications work by mimicking natural gut hormones that regulate appetite, slow gastric emptying, and enhance insulin secretion. Clinical trials have shown significant weight loss—approximately 15% with semaglutide 2.4 mg weekly and up to 20% with tirzepatide at higher doses—which can improve metabolic health, including blood pressure and glycemic control.
The kidneys play a critical role in filtering waste products, maintaining fluid and electrolyte balance, and regulating blood pressure. Kidney function is typically assessed through serum creatinine, estimated glomerular filtration rate (eGFR), and urinary albumin-to-creatinine ratio. Chronic kidney disease (CKD) is defined as abnormalities in kidney structure or function (eGFR <60 mL/min/1.73m² or albuminuria ≥30 mg/g) present for at least 3 months. Many patients seeking weight loss injections have comorbidities such as type 2 diabetes, hypertension, and obesity—all established risk factors for CKD.
Understanding the relationship between weight loss medications and kidney health requires distinguishing between direct drug toxicity, indirect effects from rapid weight loss or dehydration, and the baseline kidney disease burden in this patient population. These medications are primarily eliminated through protein catabolism rather than renal excretion, which theoretically reduces direct kidney exposure. However, their effects on fluid balance, gastrointestinal symptoms, and metabolic parameters can indirectly influence kidney function.
Clinicians must carefully evaluate baseline kidney function before initiating weight loss injections and monitor patients throughout treatment, particularly those with pre-existing kidney disease or multiple cardiovascular risk factors. Gradual dose titration, as recommended in FDA labeling, helps minimize gastrointestinal side effects.
The evidence regarding weight loss injections and kidney problems is nuanced. Large clinical trials of GLP-1 receptor agonists, including the STEP trials for semaglutide and SURMOUNT trials for tirzepatide, have shown low rates of acute kidney injury (AKI) compared to placebo. In fact, some studies suggest potential renoprotective effects. The FLOW trial demonstrated that semaglutide slowed CKD progression in patients with type 2 diabetes and CKD, while SURPASS-4 showed that tirzepatide was associated with reduced albuminuria progression compared to insulin glargine in patients with type 2 diabetes.
However, FDA labeling for both semaglutide and tirzepatide includes warnings about acute kidney injury, particularly in patients experiencing severe gastrointestinal adverse effects. The mechanism appears to be prerenal azotemia—kidney dysfunction resulting from volume depletion rather than direct drug toxicity. Nausea, vomiting, and diarrhea, which occur in 20-40% of patients initiating these medications, can lead to dehydration and reduced kidney perfusion if fluid intake is inadequate.
Importantly, while direct nephrotoxicity is not established as a common mechanism, rare case reports of intrinsic kidney injury exist. The FDA recommends monitoring kidney function in patients who report severe adverse gastrointestinal reactions or who have baseline renal impairment.
Regarding use in patients with kidney disease, neither semaglutide nor tirzepatide requires dose adjustment based on renal function, even in severe CKD or end-stage renal disease. However, clinical experience in patients on dialysis or with advanced CKD and obesity (without diabetes) is more limited. The American Diabetes Association guidelines support GLP-1 receptor agonist use in patients with diabetic kidney disease, recognizing their cardiovascular and potential renal benefits, but emphasize individualized risk assessment and close follow-up.
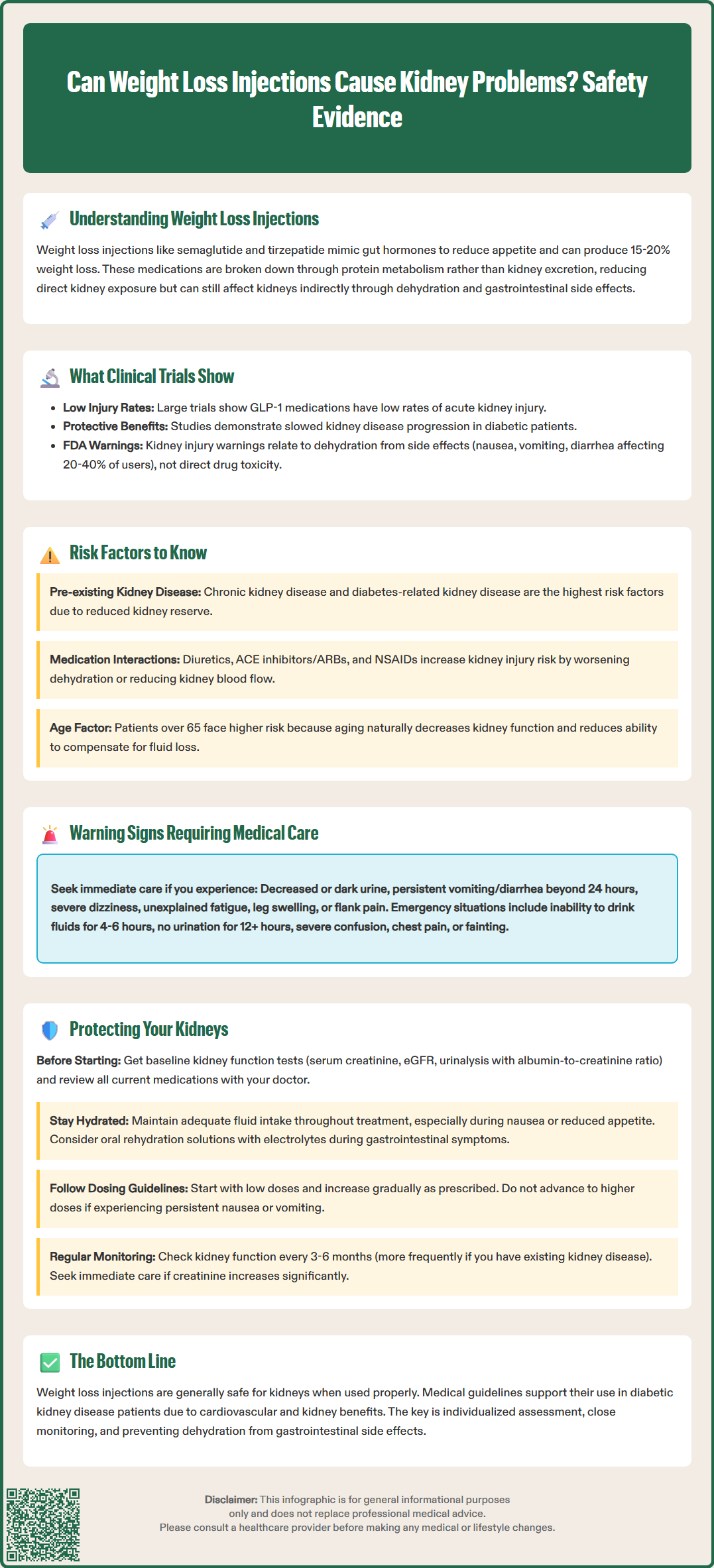
Several patient-specific factors increase the risk of kidney complications when using weight loss injections. Pre-existing chronic kidney disease is the most significant risk factor, as these patients have reduced renal reserve and are more vulnerable to volume depletion. Patients with diabetes-related kidney disease (diabetic nephropathy) require particular attention, as they may already have compromised kidney function despite normal creatinine levels.
Concurrent medications that affect kidney function or fluid balance amplify risk. These include:
Diuretics (furosemide, hydrochlorothiazide) which can exacerbate volume depletion
ACE inhibitors or ARBs (lisinopril, losartan) which may cause acute kidney injury when combined with dehydration
NSAIDs (ibuprofen, naproxen) which reduce kidney blood flow
SGLT2 inhibitors (empagliflozin, dapagliflozin) which cause osmotic diuresis, though these medications have proven renal and cardiovascular benefits and should not be discontinued without medical advice
Advanced age (over 65 years) and cardiovascular disease also increase vulnerability to kidney injury. Older adults have naturally declining kidney function and may be less able to compensate for fluid losses.
Warning signs that warrant immediate medical evaluation include:
Decreased urine output or dark, concentrated urine
Persistent nausea, vomiting, or diarrhea lasting more than 24 hours
Dizziness, lightheadedness, or orthostatic symptoms suggesting volume depletion
Unexplained fatigue or confusion which may indicate uremia
Swelling of the legs, ankles, or face suggesting fluid retention
Flank pain or blood in the urine (though rare with these medications)
Emergency red flags include inability to keep fluids down for 4-6 hours, no urination for ≥12 hours, severe confusion, chest pain, or syncope.
Patients experiencing severe gastrointestinal symptoms should contact their healthcare provider promptly. Those unable to maintain adequate oral intake may require intravenous fluid resuscitation and kidney function testing.
The FDA's evaluation of weight loss injections has included extensive kidney safety monitoring through clinical trials and post-marketing surveillance. The prescribing information for both semaglutide (Wegovy) and tirzepatide (Zepbound) includes warnings about the risk of acute kidney injury, particularly in patients who experience severe adverse gastrointestinal reactions. The FDA recommends monitoring kidney function in patients reporting severe adverse gastrointestinal reactions and in those with renal impairment.
Importantly, no dose adjustments are required for patients with renal impairment, including those with severe CKD or end-stage renal disease, though clinical experience in patients on dialysis is more limited.
In the STEP clinical trial program for semaglutide, involving over 4,500 participants, serious kidney-related adverse events were uncommon and typically associated with severe dehydration from gastrointestinal symptoms. For tirzepatide, the SURMOUNT trials demonstrated a favorable kidney safety profile. The SURPASS-4 trial showed that tirzepatide was associated with reduced progression of albuminuria compared to insulin glargine in patients with type 2 diabetes, suggesting potential kidney benefits.
The FDA Adverse Event Reporting System (FAERS) has received reports of acute kidney injury associated with these medications, but these reports do not establish causation and often involve patients with multiple risk factors or concurrent illnesses. The FDA continues to monitor these medications through routine pharmacovigilance.
Clinicians should note that FDA labeling emphasizes the importance of patient education about gastrointestinal side effects and maintaining adequate hydration. The kidney warnings reflect the potential for indirect effects through volume depletion in susceptible individuals rather than direct nephrotoxicity.
Patients and clinicians can take several evidence-based steps to minimize kidney risks while using weight loss injections. Baseline kidney function assessment is essential before starting treatment. This should include serum creatinine, eGFR calculation, and urinalysis with albumin-to-creatinine ratio.
Adequate hydration is the cornerstone of kidney protection. Patients should maintain appropriate fluid intake based on their individual needs and medical conditions. Those with heart failure or severe CKD may have fluid restrictions and should follow their clinician's guidance. Patients experiencing nausea or reduced appetite should prioritize hydration even when food intake is limited. Oral rehydration solutions containing electrolytes may be beneficial during gastrointestinal symptoms.
Medication review and adjustment should occur before initiating weight loss injections. Consider:
Monitoring diuretic needs during dose escalation or gastrointestinal symptoms
Monitoring blood pressure closely if taking ACE inhibitors or ARBs
Avoiding NSAIDs for routine pain management; use acetaminophen instead
Coordinating with specialists if taking multiple medications affecting kidney function
Gradual dose titration as recommended in FDA labeling helps minimize gastrointestinal side effects and associated dehydration risk. Patients should not advance to higher doses if experiencing persistent nausea or vomiting.
Regular monitoring should include kidney function testing at 3-6 month intervals, or more frequently in patients with baseline kidney disease or risk factors. According to KDIGO (Kidney Disease: Improving Global Outcomes) criteria, acute kidney injury is defined as an increase in serum creatinine by ≥0.3 mg/dL within 48 hours or ≥1.5 times baseline within 7 days. These thresholds warrant prompt evaluation.
Patient education should emphasize recognizing warning signs and knowing when to seek care. Patients should understand that temporary medication management during acute illness ("sick-day management") may be necessary, particularly with gastrointestinal infections or other conditions causing fluid loss. Establishing clear communication channels with healthcare providers ensures prompt intervention if kidney concerns arise.
Nephrology referral should be considered for patients with eGFR <30 mL/min/1.73m², albuminuria ≥300 mg/g, rapidly progressive kidney function decline, or refractory electrolyte abnormalities.
No dose adjustment is required for semaglutide or tirzepatide based on kidney function, even in severe chronic kidney disease or end-stage renal disease. However, patients with kidney disease require closer monitoring for dehydration and gastrointestinal side effects.
Warning signs include decreased urine output, dark concentrated urine, persistent nausea or vomiting lasting more than 24 hours, dizziness suggesting dehydration, unexplained fatigue, and leg swelling. Contact your healthcare provider immediately if you experience these symptoms.
Maintain adequate hydration, especially during gastrointestinal symptoms, follow gradual dose titration as prescribed, have baseline kidney function testing before starting treatment, and undergo regular monitoring every 3-6 months. Avoid NSAIDs and inform your doctor about all medications you take.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.