LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro®, Zepbound®) is an FDA-approved dual GIP/GLP-1 receptor agonist for type 2 diabetes and chronic weight management. While highly effective, gastrointestinal side effects—particularly constipation (10-24%), nausea (17-31%), and diarrhea (12-23%)—are common due to slowed gastric emptying. Adequate fiber intake becomes essential during treatment to support digestive health and mitigate these effects. However, reduced appetite on tirzepatide can make meeting the recommended 25-38g daily fiber intake challenging through diet alone. Selecting the best fiber supplement for tirzepatide therapy requires understanding which types optimize tolerability, support bowel regularity, and complement the medication's metabolic benefits without interfering with treatment outcomes.
Quick Answer: Methylcellulose (Citrucel®) and psyllium husk (Metamucil®) are generally the best fiber supplements for tirzepatide users, offering effective digestive support with minimal gas production.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro®) and chronic weight management (Zepbound®). The medication works by slowing gastric emptying, enhancing insulin secretion, and reducing appetite—mechanisms that affect gastrointestinal function.
Gastrointestinal adverse effects are among the most commonly reported with tirzepatide therapy. According to FDA prescribing information, nausea occurs in 17-25% of patients taking Mounjaro and 24-31% with Zepbound, constipation in 10-17% (Mounjaro) and 16-24% (Zepbound), and diarrhea in 12-17% (Mounjaro) and 18-23% (Zepbound), with incidence varying by dose. These effects are associated with the medication's impact on gastric emptying and gut motility. Adequate fiber intake becomes particularly important during tirzepatide treatment to support regular bowel function and mitigate constipation risk.
Dietary fiber promotes digestive health through multiple mechanisms: it adds bulk to stool, facilitates intestinal transit, supports beneficial gut microbiota, and helps regulate blood glucose levels—complementing tirzepatide's glycemic effects. The Dietary Guidelines for Americans recommend adults consume about 14g of fiber per 1,000 calories (approximately 25g daily for women and 38g for men), which the American Diabetes Association endorses for people with diabetes. However, NHANES data shows most Americans consume only about 15 grams on average. For patients experiencing reduced appetite on tirzepatide, meeting fiber requirements through diet alone may prove challenging.
Fiber supplementation offers a practical strategy to maintain adequate intake during treatment. However, the timing, type, and amount of supplemental fiber require careful consideration. While tirzepatide itself is administered by injection and not affected by oral fiber intake, fiber supplements may interfere with the absorption of other oral medications. Understanding which fiber supplements work best alongside tirzepatide can help optimize both therapeutic outcomes and tolerability.
Dietary fiber comprises two main categories—soluble and insoluble—each with distinct physiological properties and clinical applications. Understanding these differences helps guide appropriate supplementation during tirzepatide therapy.
Soluble fiber dissolves in water to form a gel-like substance in the digestive tract. This type slows gastric emptying, moderates glucose absorption, and can help lower LDL cholesterol. Common soluble fiber supplements include:
Psyllium husk (Metamucil®, Konsyl®): derived from Plantago ovata seeds, contains approximately 70% soluble fiber
Methylcellulose (Citrucel®): a semi-synthetic fiber that is non-fermentable and typically well-tolerated
Inulin and oligofructose: prebiotic fibers that support beneficial gut bacteria but may increase gas production
Wheat dextrin (Benefiber® Original): a soluble, low-viscosity fiber that dissolves completely in liquids
Soluble fiber is particularly beneficial for patients with diarrhea-predominant symptoms, as it absorbs excess water and adds form to loose stools. The American Gastroenterological Association recommends psyllium as a first-line treatment for chronic constipation due to its effectiveness and safety profile.
Insoluble fiber does not dissolve in water and passes through the digestive system largely intact. It adds bulk to stool and accelerates intestinal transit. Sources include:
Wheat bran: high in insoluble fiber, effective for promoting regularity
Cellulose: found in many vegetables and available as a supplement
For tirzepatide users experiencing constipation, psyllium or a combination product may provide the most benefit based on clinical guidelines. Patients with diarrhea should generally emphasize soluble fiber. Many commercial products contain both types in varying ratios, offering balanced support for overall digestive function. Insoluble fiber should be introduced cautiously as it may increase bloating and gas in some individuals, potentially compounding tirzepatide's gastrointestinal effects.
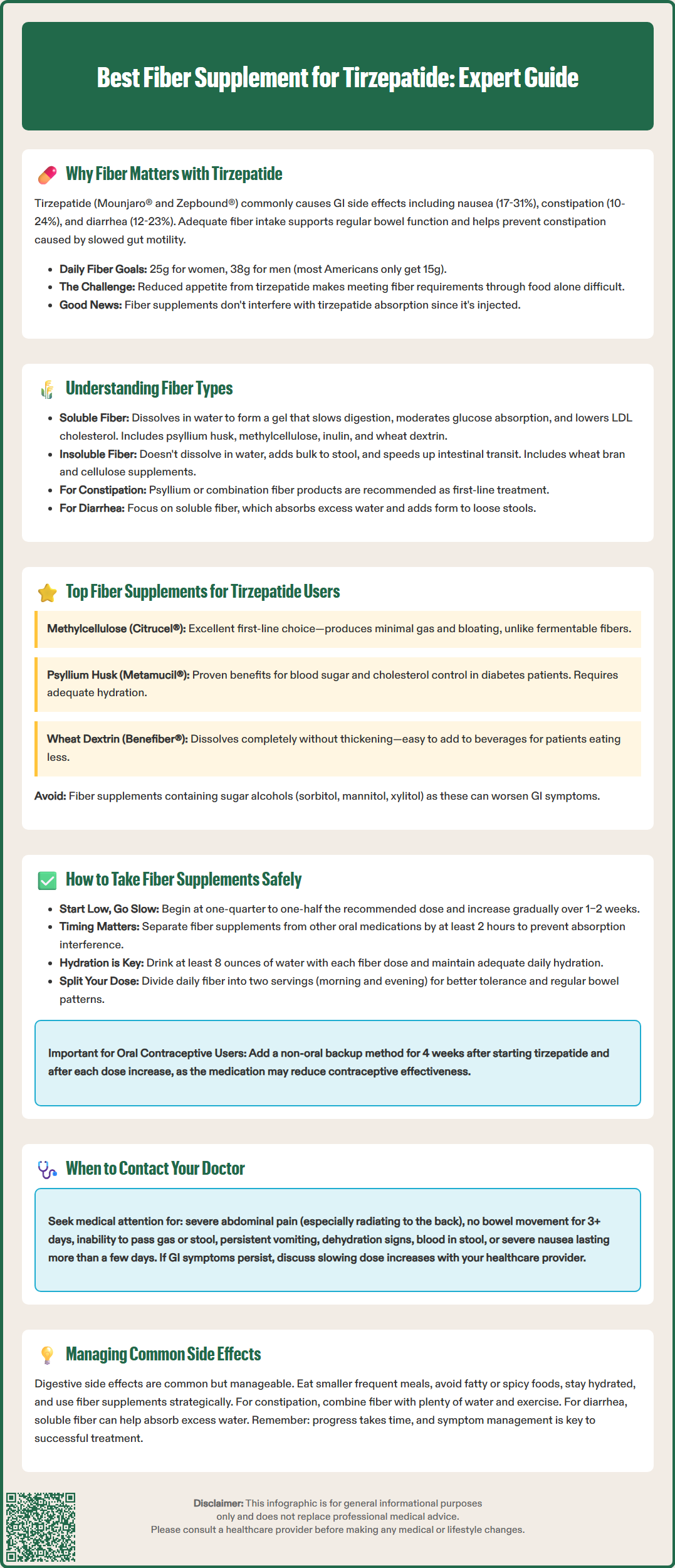
Several fiber supplements have favorable profiles for use alongside tirzepatide, based on their mechanism of action, tolerability, and lack of significant drug interactions. No fiber supplement has been specifically studied in combination with tirzepatide in clinical trials, but general principles of fiber supplementation and GLP-1 receptor agonist therapy inform these recommendations.
Methylcellulose (Citrucel®) represents an excellent first-line option for many patients. This non-fermentable fiber supplement produces minimal gas and bloating—important considerations given tirzepatide's gastrointestinal side effect profile. Methylcellulose is a soluble fiber that absorbs water and adds bulk without the fermentation that can worsen abdominal discomfort. Like all bulk-forming fibers, it should be taken separately from oral medications to prevent potential interference with absorption.
Psyllium husk (Metamucil®, Konsyl®) is a well-studied fiber supplement with extensive safety data. It provides predominantly soluble fiber and has demonstrated benefits for glycemic control and cholesterol reduction in patients with diabetes. Psyllium can absorb significant amounts of water, so adequate hydration is essential. Some patients experience increased gas initially, though tolerance typically improves within 1–2 weeks.
Wheat dextrin (Benefiber® Original) offers a convenient, tasteless option that dissolves completely in liquids without thickening. This soluble fiber is well-tolerated by many patients and can be easily incorporated into the reduced food intake common during tirzepatide therapy.
Combination products containing both soluble and insoluble fiber may benefit patients experiencing mixed bowel symptoms. However, these should be introduced gradually to assess individual tolerance.
Patients should avoid fiber supplements containing sugar alcohols (sorbitol, mannitol, xylitol), as these can worsen gastrointestinal symptoms. Sugar-free formulations are preferable for patients with diabetes. When possible, select products with third-party quality verification (USP Verified, NSF certification) as fiber supplements are regulated as foods rather than drugs by the FDA.
Proper timing and administration of fiber supplements relative to tirzepatide injections can optimize both medication efficacy and gastrointestinal tolerability. Tirzepatide is administered subcutaneously once weekly and does not require specific timing with meals, but fiber supplementation strategy should account for the medication's effects on gut motility.
Timing considerations: While there is no direct pharmacokinetic interaction between injectable tirzepatide and oral fiber supplements, it is prudent to separate fiber supplementation from any oral medications by at least 2 hours. This precaution prevents potential interference with absorption of other drugs, particularly those with narrow therapeutic windows such as levothyroxine, digoxin, and certain anticonvulsants. Tirzepatide itself, being injected, is not affected by oral fiber intake.
Initiation and titration: Begin fiber supplementation at a low dose—approximately one-quarter to one-half of the recommended serving size—and increase gradually over 1–2 weeks. This approach minimizes gas, bloating, and cramping that can occur with abrupt increases in fiber intake. Some patients may find it helpful to start fiber supplementation after establishing tolerance to tirzepatide, though this approach is based on clinical experience rather than specific studies.
Hydration requirements: Adequate fluid intake is critical when taking fiber supplements, particularly with tirzepatide's appetite-suppressing effects potentially reducing overall fluid consumption. Patients should consume at least 8 ounces of water with each fiber supplement dose and maintain adequate daily fluid intake. Patients with heart failure, kidney disease, or other conditions requiring fluid restriction should consult their healthcare provider for personalized hydration targets. Insufficient hydration can paradoxically worsen constipation and increase risk of intestinal obstruction, though this complication is rare.
Dosing strategy: Most patients benefit from divided doses rather than a single large dose. For example, taking half the daily fiber supplement in the morning and half in the evening distributes the gastrointestinal effects and may improve tolerance. Consistency in timing helps establish regular bowel patterns.
Special considerations: The FDA prescribing information for tirzepatide notes that it may decrease exposure to oral contraceptives, particularly during dose initiation and escalation. Patients using oral contraceptives should use an additional non-oral contraceptive method for 4 weeks after starting tirzepatide and for 4 weeks after each dose increase.
Gastrointestinal adverse effects represent the primary tolerability challenge with tirzepatide therapy, and a comprehensive management strategy extends beyond fiber supplementation alone. Understanding when fiber helps, when it may worsen symptoms, and when to seek medical evaluation is essential for patient safety.
Nausea management: Nausea is the most frequently reported adverse effect with tirzepatide, occurring most commonly during dose escalation. While fiber does not directly address nausea, maintaining regular bowel function can prevent the additional discomfort of constipation-related nausea. Patients should eat smaller, more frequent meals; avoid high-fat, spicy, or strong-smelling foods; and stay well-hydrated. If nausea is severe or persistent (lasting more than a few days after injection), patients should contact their healthcare provider, as dose adjustment or antiemetic medication may be warranted.
Constipation: This common side effect results from slowed gastric emptying and reduced gut motility. Fiber supplementation, particularly psyllium or mixed fiber products, should be first-line management alongside increased water intake and physical activity. If no bowel movement occurs for 3 or more days, or constipation is accompanied by severe abdominal pain, distension, or vomiting, patients should seek medical evaluation to rule out more serious complications such as ileus or bowel obstruction.
Diarrhea: When diarrhea occurs with tirzepatide, soluble fiber supplements like psyllium or methylcellulose can help by absorbing excess water and adding form to stools. However, if diarrhea is accompanied by blood, fever, dehydration, or severe abdominal pain, immediate medical attention is necessary. These symptoms may indicate complications unrelated to expected medication effects.
When to contact a healthcare provider: Patients should seek medical advice if they experience:
Severe or persistent abdominal pain, especially if radiating to the back (potential pancreatitis)
Right upper quadrant pain, fever, or yellowing of skin/eyes (potential gallbladder disease)
Inability to pass gas or stool for more than 3 days
Vomiting that prevents adequate hydration
Signs of dehydration (dark urine, dizziness, decreased urination)
Blood in stool or black, tarry stools
Unintentional weight loss exceeding expected therapeutic effects
New or worsening symptoms after several weeks of stable treatment
Patients experiencing persistent gastrointestinal symptoms should discuss with their provider whether adjusting the tirzepatide dose escalation schedule or temporarily holding at a lower dose might improve tolerability while maintaining therapeutic benefits.
Yes, fiber supplements do not interfere with injectable tirzepatide since it is administered subcutaneously. However, separate fiber from any oral medications by at least 2 hours to prevent potential absorption interference.
Methylcellulose (Citrucel®) is a non-fermentable fiber that produces minimal gas and bloating, making it an excellent first-line choice for patients on tirzepatide who are already experiencing gastrointestinal side effects.
Consume at least 8 ounces of water with each fiber supplement dose and maintain adequate daily fluid intake. Insufficient hydration can worsen constipation, particularly important given tirzepatide's appetite-suppressing effects may reduce overall fluid consumption.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.