LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
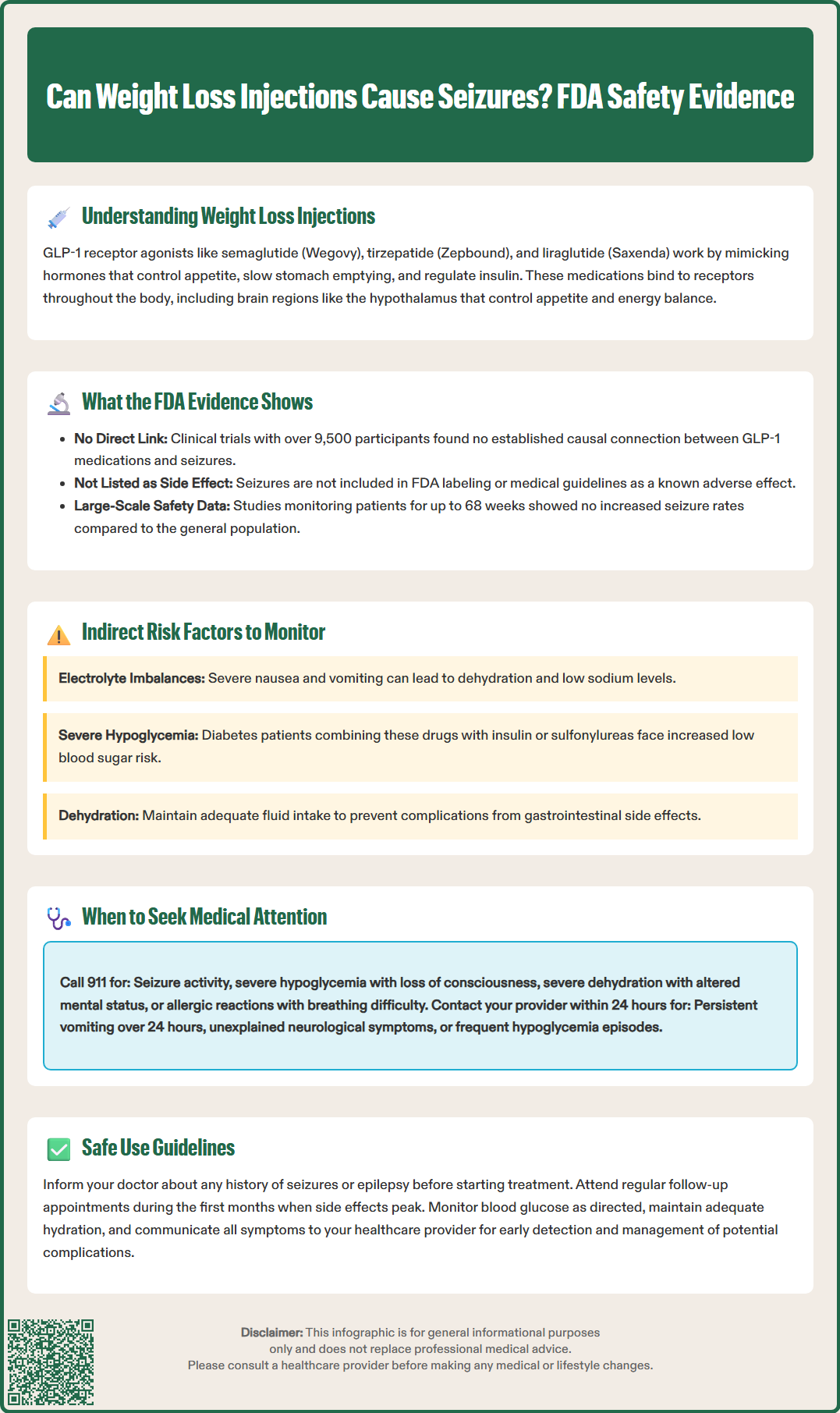
Weight loss injections, particularly GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro), have transformed obesity treatment in the United States. As these medications gain widespread use, patients and clinicians naturally question their complete safety profile, including potential neurological effects. Can weight loss injections cause seizures? Understanding the evidence-based answer to this concern is essential for informed treatment decisions. This article examines current FDA data, clinical trial evidence, and safety considerations to clarify the relationship between weight loss injections and seizure risk, helping patients and providers navigate this important safety question.
Quick Answer: Based on FDA-approved labeling and large-scale clinical trials, there is no established causal link between GLP-1 receptor agonist weight loss injections and seizures.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections have become increasingly prevalent in clinical practice, with glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro) leading the therapeutic landscape. These medications work by mimicking naturally occurring incretin hormones that regulate appetite, slow gastric emptying, and enhance insulin secretion in response to meals. While their efficacy in achieving significant weight reduction is well-established, understanding their complete safety profile—including potential neurological effects—remains essential for both clinicians and patients.
The mechanism of action of GLP-1 receptor agonists involves binding to receptors distributed throughout the body, including the central nervous system. GLP-1 receptors are present in various brain regions, including the hypothalamus, which regulates appetite and energy homeostasis. This central nervous system activity raises legitimate questions about potential neurological adverse effects, including the theoretical concern about seizure risk.
Most FDA-approved weight loss injections are incretin-based (GLP-1 or dual GIP/GLP-1 receptor agonists). These include semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound). Setmelanotide is reserved for specific rare genetic forms of obesity. Each medication has undergone rigorous clinical trials examining safety outcomes, though the specific relationship between these agents and seizure activity requires careful examination of available evidence. Understanding the distinction between established adverse effects and theoretical or unconfirmed risks helps patients and providers make informed treatment decisions while maintaining appropriate clinical vigilance.
Based on current FDA-approved labeling and published clinical trial data, there is no established causal link between GLP-1 receptor agonist weight loss injections and seizures. Seizures are not listed as a known adverse effect in the prescribing information for semaglutide, tirzepatide, or liraglutide. Large-scale randomized controlled trials, including the STEP program for semaglutide (≥4,500 participants) and SURMOUNT trials for tirzepatide (>5,000 participants), have not identified seizures as a significant safety signal associated with these medications.
However, this does not mean the question is entirely without clinical relevance. Post-marketing surveillance and pharmacovigilance databases occasionally report seizure events in patients using weight loss medications, but establishing causality versus coincidental occurrence remains challenging. About 1.2% of US adults have active epilepsy, and the lifetime risk of epilepsy is approximately 3%, creating a background rate of seizure disorders in the general population.
Indirect mechanisms could theoretically contribute to seizure risk in specific circumstances. Rapid weight loss from any cause can lead to electrolyte disturbances, particularly hyponatremia (low sodium) or hypoglycemia (low blood sugar), both of which are recognized seizure triggers. GLP-1 receptor agonists can cause significant nausea and vomiting in some patients, potentially leading to dehydration and electrolyte imbalances if fluid intake is inadequate. Additionally, patients with diabetes using these medications alongside insulin or sulfonylureas face increased hypoglycemia risk, which could precipitate seizures in severe cases.
The current medical consensus, supported by the American Diabetes Association and obesity medicine guidelines, does not identify seizures as a contraindication or significant concern when prescribing GLP-1 receptor agonists for weight management. Clinicians should focus on established adverse effects such as gastrointestinal symptoms, pancreatitis risk, and thyroid considerations rather than unsubstantiated neurological concerns.
While weight loss injections themselves do not directly cause seizures, certain patient populations and clinical scenarios warrant heightened awareness. Patients with a pre-existing seizure disorder or epilepsy should inform their healthcare provider before starting any weight loss medication, as metabolic changes associated with treatment could theoretically affect seizure threshold or interact with antiepileptic medications.
Key risk factors that may increase vulnerability include:
History of seizures or epilepsy – Baseline neurological conditions require careful monitoring during any metabolic intervention
Diabetes with insulin or sulfonylurea use – Increased hypoglycemia risk, which can trigger seizures when severe (Level 2 hypoglycemia <54 mg/dL or Level 3 requiring assistance)
Electrolyte disorders – Pre-existing sodium, calcium, or magnesium imbalances that could worsen with gastrointestinal side effects
Severe nausea and vomiting – Inability to maintain adequate hydration and nutrition
Rapid weight loss – Particularly when accompanied by poor intake or dehydration that can precipitate electrolyte disturbances
Alcohol use disorder – Alcohol withdrawal combined with metabolic changes presents compounded risk
Warning signs requiring clinical attention include:
Persistent severe nausea preventing adequate fluid intake, symptoms of dehydration (dark urine, dizziness, confusion), signs of hypoglycemia (tremor, sweating, confusion, palpitations), unexplained muscle weakness or cramping suggesting electrolyte disturbance, and any new neurological symptoms such as unusual sensations, visual changes, or altered consciousness.
Patients should maintain regular follow-up appointments during the initial months of treatment, when side effects are most pronounced. Healthcare providers typically monitor weight loss trajectory, assess tolerability of gastrointestinal effects, and may order laboratory tests including comprehensive metabolic panels to evaluate electrolyte status and kidney function. For patients with diabetes, more frequent blood glucose monitoring helps prevent hypoglycemic episodes that could pose neurological risk.
Patients taking medications with a narrow therapeutic index, including some antiseizure medications, should be monitored closely, as delayed gastric emptying from GLP-1 receptor agonists may affect drug absorption.
The FDA's approval process for weight loss medications involves comprehensive safety evaluation through multiple phases of clinical trials. For semaglutide (Wegovy), the STEP trial program enrolled over 4,500 participants across multiple studies, with safety monitoring extending up to 68 weeks. Similarly, tirzepatide's SURMOUNT trials included more than 5,000 participants. Throughout these extensive clinical development programs, seizures were not identified as an adverse event occurring at rates higher than expected in the general population.
The FDA Adverse Event Reporting System (FAERS) serves as a post-marketing surveillance tool that collects voluntary reports of adverse events associated with medications. While this database may contain isolated reports of seizures in patients using weight loss injections, such reports do not establish causation. The FAERS database is subject to reporting bias, lacks denominator data (total number of patients exposed), and cannot distinguish between coincidental associations and true drug-related effects.
Prescribing information for currently approved GLP-1 receptor agonists lists established adverse effects with clear frequency data. Common side effects (occurring in ≥5% of patients) include nausea, diarrhea, vomiting, constipation, and abdominal pain. Serious but rare adverse effects specifically mentioned include pancreatitis, gallbladder disease, acute kidney injury (typically related to dehydration), and hypoglycemia when used with insulin or insulin secretagogues. Notably, seizures do not appear in these safety sections.
The FDA does require a boxed warning for GLP-1 receptor agonists (Wegovy, Saxenda) and the dual GIP/GLP-1 receptor agonist tirzepatide (Zepbound) regarding thyroid C-cell tumors, based on rodent studies, though human relevance remains uncertain. This demonstrates the agency's conservative approach to safety signaling. The absence of seizure-related warnings or precautions in FDA-approved labeling reflects the lack of evidence supporting a meaningful association. Healthcare providers should rely on this official safety information rather than anecdotal reports when counseling patients about neurological risks.
Patients using weight loss injections should understand which symptoms warrant immediate medical evaluation versus those that can be addressed at a scheduled appointment. While seizures are not an expected complication of GLP-1 receptor agonist therapy, any seizure-like event requires urgent assessment regardless of medication use.
Seek emergency medical care (call 911) if experiencing:
Seizure activity – Convulsions, loss of consciousness, uncontrolled shaking, or post-event confusion
Severe hypoglycemia symptoms – Extreme confusion, loss of consciousness, inability to swallow, or seizure in a patient with diabetes
Signs of severe dehydration – Inability to urinate, extreme dizziness, rapid heartbeat, or altered mental status
Severe abdominal pain – Particularly if radiating to the back, which may indicate pancreatitis
Allergic reactions – Difficulty breathing, throat swelling, or widespread rash
Contact your healthcare provider within 24 hours for:
Persistent vomiting preventing medication or fluid intake for more than 24 hours, signs of dehydration (decreased urination, persistent dizziness), unexplained neurological symptoms (numbness, tingling, vision changes, severe headache), symptoms of hypoglycemia occurring frequently despite medication adjustments, or severe gastrointestinal symptoms not improving with standard management.
Routine follow-up should address:
Tolerance of gastrointestinal side effects, weight loss trajectory and nutritional adequacy, blood glucose patterns for patients with diabetes, and any new or concerning symptoms even if seemingly unrelated to the medication.
Patients with pre-existing seizure disorders should maintain their established neurology care and inform both their neurologist and prescribing physician about the weight loss medication. Any changes in seizure frequency or character should prompt neurological reassessment. Maintaining adequate hydration, following prescribed dosing schedules, monitoring blood glucose as directed, and attending scheduled follow-up appointments constitute the foundation of safe weight loss injection therapy. Open communication with healthcare providers about all symptoms—even those that seem minor—enables early identification and management of potential complications.
No, seizures are not listed as a known adverse effect in FDA prescribing information for semaglutide (Wegovy, Ozempic) or other GLP-1 receptor agonists. Large clinical trials have not identified seizures as a safety concern with these medications.
Patients with pre-existing seizure disorders should inform their healthcare provider before starting weight loss injections, as metabolic changes could theoretically affect seizure threshold. However, these medications are not contraindicated in epilepsy, and close monitoring can ensure safe use.
Call 911 immediately if you experience seizure activity, loss of consciousness, or severe confusion. Contact your healthcare provider within 24 hours for persistent neurological symptoms like numbness, vision changes, or severe headaches that may require evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.