LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide build up in your system? This question concerns many patients starting this once-weekly medication for type 2 diabetes or weight management. Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist with a 5-day half-life that reaches steady-state concentrations after four to five weeks of consistent dosing. Understanding the difference between therapeutic steady state and harmful accumulation is essential for patients and clinicians. This article examines tirzepatide's pharmacokinetics, metabolism, and long-term safety profile to clarify how the medication behaves in your body over time.
Quick Answer: Tirzepatide reaches steady-state concentrations after four to five weeks but does not harmfully accumulate in the body.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults. This injectable medication mimics the action of naturally occurring incretin hormones that regulate blood sugar and appetite. After subcutaneous administration, tirzepatide binds to both GIP and GLP-1 receptors on pancreatic beta cells, enhancing insulin secretion in a glucose-dependent manner while simultaneously suppressing glucagon release when blood glucose levels are elevated. It also acts on GLP-1 receptors in the brain to regulate appetite and food intake.
The medication's pharmacokinetic profile is characterized by slow absorption and a prolonged half-life of approximately 5 days, which allows for once-weekly dosing. Following injection, tirzepatide reaches peak plasma concentrations within 8 to 72 hours. The drug undergoes proteolytic cleavage and beta-oxidation as its primary metabolic pathways, with minimal involvement of cytochrome P450 enzymes. This metabolic process occurs gradually, breaking down the peptide structure into smaller amino acid fragments that are eventually eliminated from the body.
Tirzepatide demonstrates high bioavailability of approximately 80% when administered subcutaneously in the abdomen, thigh, or upper arm. The medication's molecular structure includes modifications that protect it from rapid enzymatic degradation, contributing to its extended duration of action. Understanding these pharmacological properties is essential for clinicians and patients to appreciate how the medication maintains therapeutic levels throughout the weekly dosing interval while minimizing fluctuations in drug concentration.
Importantly, tirzepatide carries an FDA boxed warning for risk of thyroid C-cell tumors, and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
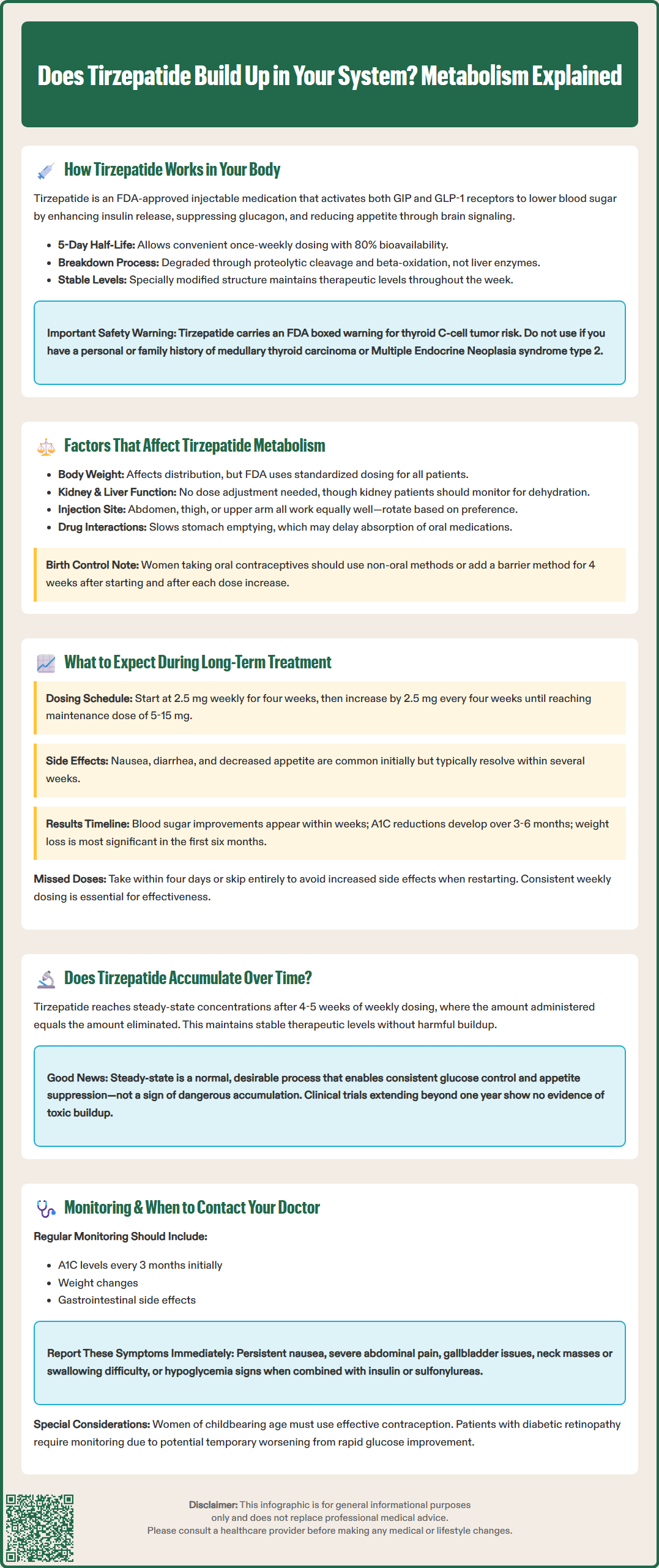
Several physiological and clinical factors influence how tirzepatide is processed and eliminated from the body. Body weight plays a significant role in drug distribution, with the FDA-approved dosing strategy accounting for this variable through standardized dose escalation rather than weight-based calculations. Patients with higher body mass may experience slightly different pharmacokinetic profiles, though the clinical significance remains modest within the therapeutic range.
Renal function has minimal impact on tirzepatide clearance, as the medication is primarily metabolized through proteolytic pathways rather than renal excretion. According to FDA labeling, no dose adjustment is required for patients with renal impairment, including those with end-stage renal disease. However, patients with kidney impairment should be monitored for potential dehydration and acute kidney injury if severe gastrointestinal side effects occur.
Hepatic function similarly shows limited influence on tirzepatide metabolism. Patients with hepatic impairment do not require dose modifications per FDA labeling. Age-related changes in metabolism appear to have minimal clinical impact, with pharmacokinetic studies showing comparable drug exposure across adult age groups. Injection site selection (abdomen, thigh, or upper arm) does not significantly alter absorption rates or overall bioavailability, providing flexibility for patient preference and rotation strategies to minimize injection site reactions.
Drug interactions with tirzepatide are relatively uncommon due to its peptide structure and metabolic pathway. However, the medication's effect on gastric emptying may delay the absorption of oral medications, particularly those requiring rapid onset of action. Notably, tirzepatide can affect the absorption of oral hormonal contraceptives. The FDA recommends using non-oral contraceptives or adding a barrier method for 4 weeks after initiation and after each dose increase when taking tirzepatide with oral contraceptives.
Long-term tirzepatide therapy follows a structured dose escalation protocol designed to optimize therapeutic benefits while minimizing gastrointestinal adverse effects. Treatment typically begins at 2.5 mg once weekly for four weeks, serving as an initial tolerability dose rather than a therapeutic maintenance dose. The dose is then increased in 2.5 mg increments every four weeks, with maintenance doses ranging from 5 mg to 15 mg weekly depending on individual glycemic control, weight management goals, and tolerability.
Patients commonly experience gastrointestinal side effects during the initial weeks and following dose increases, including nausea, diarrhea, decreased appetite, and occasional vomiting. These effects typically diminish over time as physiological adaptation occurs. Clinical trials have demonstrated that most gastrointestinal symptoms are mild to moderate in severity and resolve within several weeks of maintaining a stable dose. The gradual dose escalation strategy specifically aims to improve tolerability by allowing the digestive system to adjust to the medication's effects on gastric emptying and satiety signaling.
As treatment continues beyond the initial titration phase, patients generally achieve steady-state drug concentrations after approximately three to four weeks at each dose level. Glycemic improvements typically become evident within the first few weeks, with A1C reductions continuing to develop over three to six months. Weight loss follows a similar trajectory, with the most substantial changes occurring during the first six months of therapy, followed by continued gradual weight reduction or maintenance through one year and beyond. Patients with pre-existing diabetic retinopathy should be monitored, as rapid improvement in glucose control may temporarily worsen retinopathy.
Patients should be counseled about the importance of adherence to the weekly dosing schedule. Missing doses or inconsistent administration can lead to suboptimal therapeutic outcomes and potentially increased side effects when restarting. If a dose is missed, it should be administered within four days; otherwise, patients should skip that dose and resume the regular schedule. Tirzepatide is not recommended during pregnancy, and women of childbearing potential should use effective contraception during treatment.
Tirzepatide does reach steady-state concentrations in the body, but this represents therapeutic equilibrium rather than harmful accumulation. With its approximate 5-day half-life and once-weekly dosing schedule, the medication achieves steady-state plasma levels after approximately four to five weeks of consistent administration at a given dose. At steady state, the amount of drug administered each week equals the amount eliminated, maintaining stable therapeutic concentrations without progressive buildup.
This pharmacokinetic behavior is intentional and clinically desirable. The steady-state concentration provides consistent receptor activation throughout the dosing interval, ensuring continuous therapeutic effects on glucose regulation and appetite control. Clinical studies have not demonstrated evidence of toxic accumulation or progressive increases in drug levels beyond the expected steady-state plateau. The medication's clearance mechanisms remain functional throughout long-term treatment, with no indication of saturation or impairment of metabolic pathways.
Patients and clinicians should understand that achieving steady state is fundamentally different from harmful drug accumulation. The former represents a predictable pharmacokinetic principle that enables effective once-weekly dosing, while the latter would suggest inadequate elimination leading to toxicity. Tirzepatide's safety profile in clinical trials extending beyond one year supports the absence of problematic accumulation, with adverse events remaining consistent rather than increasing in frequency or severity over time. FDA pharmacokinetic data confirm that renal or hepatic impairment does not lead to clinically significant accumulation of tirzepatide.
Monitoring recommendations during long-term therapy focus on therapeutic outcomes and known adverse effects rather than concerns about drug buildup. Regular assessment should include glycemic control (A1C every three months initially), weight trends, gastrointestinal tolerability, and screening for potential complications. Patients should be advised to report persistent or severe nausea, severe abdominal pain (which may indicate pancreatitis), symptoms of gallbladder disease, signs of thyroid tumors (neck mass, hoarseness, difficulty swallowing), or signs of hypoglycemia, particularly when tirzepatide is used in combination with insulin or sulfonylureas. There is no requirement for routine drug level monitoring, as therapeutic drug monitoring is not clinically indicated or available for tirzepatide.
Tirzepatide has a half-life of approximately 5 days, meaning it takes about four to five weeks of consistent weekly dosing to reach steady-state concentrations in the body. The medication is gradually metabolized through proteolytic cleavage and eliminated without harmful accumulation.
No dose adjustments are required for renal or hepatic impairment per FDA labeling, as tirzepatide is primarily metabolized through proteolytic pathways. However, patients with kidney impairment should be monitored for dehydration if severe gastrointestinal side effects occur.
Regular monitoring should include A1C levels every three months initially, gastrointestinal tolerability, signs of pancreatitis or gallbladder disease, symptoms of thyroid tumors, and hypoglycemia when combined with insulin or sulfonylureas. Routine drug level monitoring is not clinically indicated for tirzepatide.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.