LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 make you poop? GLP-1 receptor agonists—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—commonly affect bowel movements, though responses vary widely among patients. These FDA-approved medications for type 2 diabetes and chronic weight management work by mimicking a natural gut hormone that slows gastric emptying and alters intestinal motility. While some patients experience diarrhea, others develop constipation, and many notice changes in bowel frequency or consistency. Understanding how these medications interact with your digestive system helps you anticipate potential side effects and recognize when symptoms require medical attention. This article explains the gastrointestinal effects of GLP-1 therapy and provides practical guidance for managing bowel changes during treatment.
Quick Answer: GLP-1 medications commonly alter bowel movements, causing either diarrhea or constipation in many patients, though individual responses vary significantly.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are medications approved by the FDA for managing type 2 diabetes and, in some formulations, for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound)—though tirzepatide is technically a dual GIP/GLP-1 receptor agonist with a slightly different mechanism. Understanding how these incretin-based therapies interact with your gastrointestinal system helps explain their common digestive side effects.
GLP-1 medications work by mimicking a naturally occurring hormone that your intestines release after eating. This hormone activates GLP-1 receptors in the enteric nervous system and through vagal pathways that influence digestive function. When activated, these receptors slow gastric emptying—the rate at which food leaves your stomach and enters your small intestine. This delayed emptying contributes to increased satiety and improved blood sugar control, which are therapeutic benefits of these medications.
However, the effects on the gastrointestinal system are widespread. These medications influence gut motility (the movement of contents through your intestines), fluid secretion, and the communication between your gut and brain. These effects explain why gastrointestinal side effects are among the most commonly reported adverse reactions to GLP-1 therapy.
According to FDA prescribing information for these medications, gastrointestinal adverse effects occur in a substantial proportion of patients. The slowed movement through your digestive system can affect bowel patterns, though the specific effects vary considerably between individuals. Some patients experience constipation due to prolonged transit time, while others may develop diarrhea, possibly related to changes in gut motility patterns or alterations in intestinal fluid handling. Notably, the gastric emptying effects often diminish over time with continued therapy, which may help reduce some digestive symptoms.
Yes, GLP-1 medications commonly cause changes in bowel movements, though the nature and severity of these changes vary significantly among patients. Clinical trial data and FDA labeling information indicate that gastrointestinal effects are dose-dependent and typically most pronounced during initial treatment or dose escalation.
Common bowel-related side effects include:
Diarrhea: Reported in approximately 8–30% of patients, with higher rates typically seen with weight management doses compared to diabetes doses. This may result from altered gut motility or changes in intestinal fluid secretion.
Constipation: Affects approximately 3–24% of patients depending on the specific medication and dose, likely due to significantly slowed gastrointestinal transit time.
Abdominal discomfort: Including bloating, cramping, or a sensation of fullness, which may accompany changes in bowel patterns.
The frequency of bowel movements may increase or decrease compared to your baseline pattern. Some patients report more frequent, looser stools, particularly after eating or during the first few weeks of treatment. Others experience reduced bowel movement frequency with harder stools. There is no single "typical" response, as individual gastrointestinal physiology and baseline bowel habits influence how these medications affect you.
These changes generally occur because GLP-1 receptor activation fundamentally alters the coordinated muscular contractions (peristalsis) that move contents through your intestines. The medication doesn't specifically "make you poop" in the sense of acting as a laxative, but rather modifies your overall digestive transit and function. Most patients find that bowel changes are most noticeable during initial treatment and often improve as their body adapts to the medication, though some degree of altered bowel pattern may persist throughout treatment. In rare cases, more serious complications like intestinal obstruction have been reported in FDA labeling for some of these medications.
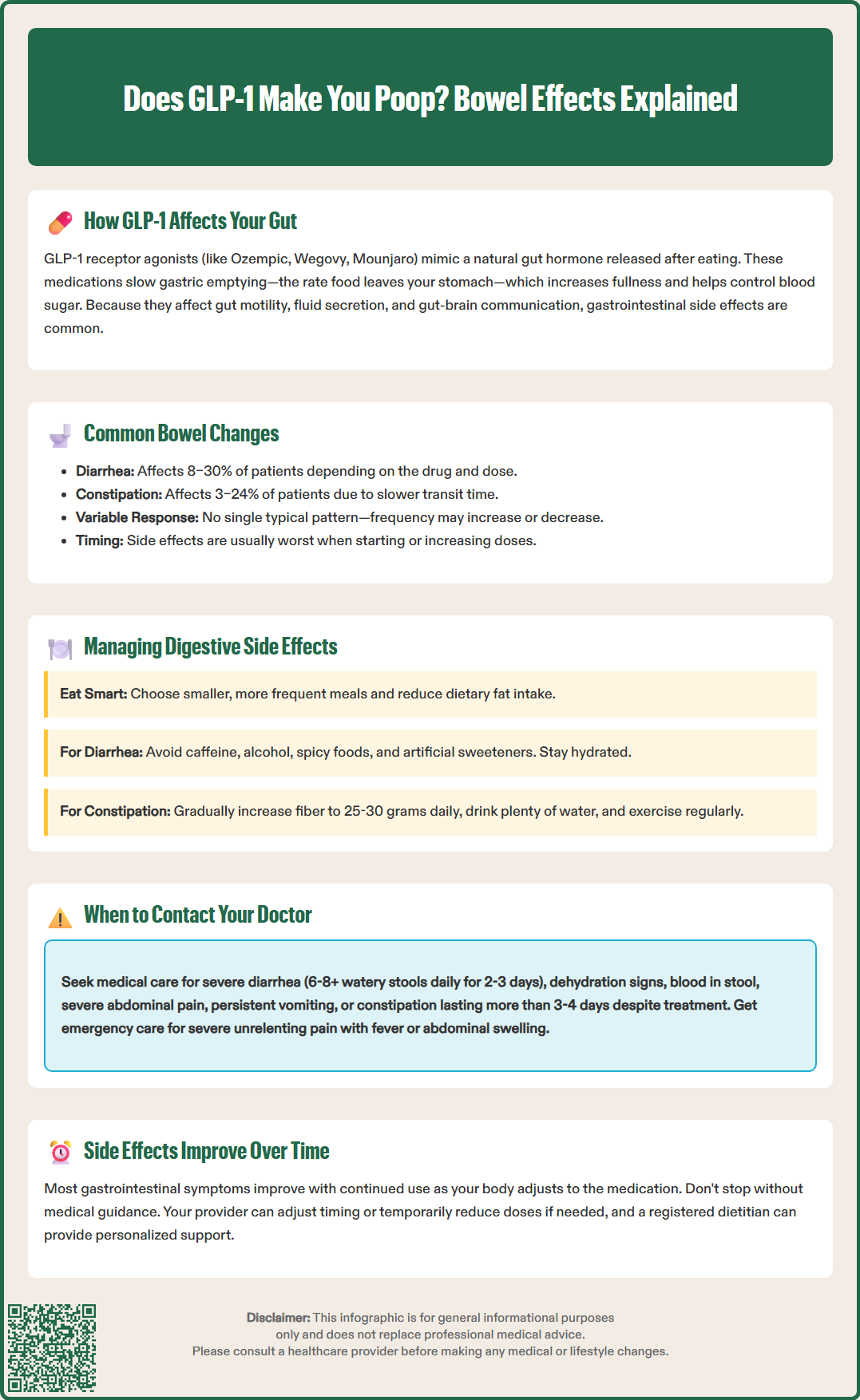
Effectively managing digestive side effects can significantly improve your treatment experience and adherence to GLP-1 therapy. Most gastrointestinal symptoms are mild to moderate and can be addressed through practical dietary and lifestyle modifications.
For diarrhea or loose stools:
Eat smaller, more frequent meals rather than large portions, which can overwhelm your slowed digestive system.
Reduce dietary fat intake, as high-fat foods are particularly difficult to digest when gastric emptying is delayed.
Avoid foods that commonly trigger diarrhea, such as caffeine, alcohol, spicy foods, and artificial sweeteners.
Stay well-hydrated; ask your healthcare provider about specific fluid recommendations if you have heart or kidney disease.
Over-the-counter antidiarrheal medications like loperamide may be used short-term after discussing with your healthcare provider, but avoid overuse.
For constipation:
Gradually increase dietary fiber intake through fruits, vegetables, and whole grains, aiming for 25–30 grams daily. Start slowly to avoid worsening bloating or fullness.
Maintain adequate hydration, as fiber requires sufficient fluid to be effective.
Engage in regular physical activity, which stimulates intestinal motility.
Establish a consistent bathroom routine, allowing adequate time without rushing.
If dietary measures are insufficient, over-the-counter fiber supplements (psyllium, methylcellulose) or osmotic laxatives (polyethylene glycol) may be appropriate after discussing with your healthcare provider.
General strategies:
Follow the prescribed dose titration schedule carefully. If gastrointestinal symptoms are problematic, your provider may recommend delaying dose increases, temporarily reducing your dose, or holding treatment briefly while symptoms improve. Eat slowly and chew food thoroughly to aid digestion. Avoid lying down immediately after meals, which can worsen symptoms related to delayed gastric emptying. Keep a symptom diary to identify specific food triggers. The American Diabetes Association recommends medical nutrition therapy with a registered dietitian for people with diabetes and those on weight management programs. Most importantly, do not discontinue your medication without medical guidance, as symptoms often improve with continued use and appropriate management strategies.
While mild digestive changes are expected with GLP-1 therapy, certain symptoms warrant prompt medical evaluation. Understanding when bowel changes represent a normal medication effect versus a potentially serious complication is essential for patient safety.
Contact your healthcare provider promptly if you experience:
Severe or persistent diarrhea: More than 6–8 watery stools daily, or diarrhea lasting beyond 2–3 days, which may lead to dehydration and electrolyte imbalances.
Signs of dehydration: Excessive thirst, dark urine, dizziness, decreased urination, or confusion.
Severe constipation: No bowel movement for more than 3–4 days despite home management, or inability to pass gas.
Severe abdominal pain: Particularly if constant, worsening, or localized to one area, which could indicate complications such as pancreatitis (severe pain often radiating to the back) or bowel obstruction.
Blood in stool: Either bright red blood or black, tarry stools, which may indicate gastrointestinal bleeding.
Persistent nausea and vomiting: Especially if preventing adequate fluid or medication intake.
Upper right abdominal pain, fever, or yellowing of skin/eyes: These may indicate gallbladder disease, which occurs at higher rates in patients taking GLP-1 medications.
Unintentional weight loss: Beyond expected therapeutic weight reduction, or inability to maintain adequate nutrition.
Seek emergency care immediately for:
Severe, unrelenting abdominal pain, particularly if accompanied by fever, vomiting, or abdominal distension. These symptoms may indicate serious complications such as acute pancreatitis, bowel obstruction, or severe gallbladder disease requiring urgent intervention.
If you experience severe vomiting or diarrhea, temporarily hold your next dose and contact your healthcare provider, as dehydration can increase the risk of acute kidney injury. Your doctor may need to adjust your GLP-1 dose, temporarily discontinue therapy, or investigate alternative causes for your symptoms. Persistent gastrointestinal symptoms should prompt evaluation for other conditions, as these medications can unmask or worsen pre-existing digestive disorders. Never assume that all digestive symptoms are simply medication side effects without appropriate medical assessment, particularly if symptoms are severe, worsening, or accompanied by warning signs.
Most bowel changes are most noticeable during initial treatment and often improve as your body adapts to the medication, typically within several weeks. However, some degree of altered bowel pattern may persist throughout treatment, and symptoms may temporarily worsen with dose increases.
Over-the-counter antidiarrheal medications like loperamide or fiber supplements and osmotic laxatives may be appropriate for short-term use, but you should discuss these options with your healthcare provider before starting them to ensure safe and effective management.
Both diarrhea and constipation are common, with diarrhea generally reported more frequently (8–30% of patients) compared to constipation (3–24%). Individual responses vary based on the specific medication, dose, and personal gastrointestinal physiology.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.