LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and weight management. Many patients wonder about semaglutide and high blood pressure, particularly whether this medication increases cardiovascular risk. Clinical evidence consistently shows that semaglutide typically lowers blood pressure rather than raising it, with reductions of 3–8 mmHg observed in major trials. These improvements occur primarily through significant weight loss and metabolic benefits. Understanding how semaglutide affects blood pressure helps patients and clinicians optimize treatment safety and cardiovascular outcomes during therapy.
Quick Answer: Semaglutide typically lowers blood pressure rather than raising it, with clinical trials showing systolic reductions of 3–8 mmHg primarily through weight loss and metabolic improvements.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Available under brand names including Ozempic, Wegovy, and Rybelsus, this medication mimics the action of naturally occurring GLP-1, a hormone that plays multiple roles in glucose metabolism and appetite regulation.
The mechanism of action involves binding to GLP-1 receptors located throughout the body, including the pancreas, brain, and cardiovascular system. In the pancreas, semaglutide stimulates glucose-dependent insulin secretion while suppressing inappropriate glucagon release, leading to improved glycemic control. In the central nervous system, it acts on appetite centers in the hypothalamus to reduce hunger and increase satiety, contributing to significant weight loss in many patients. The medication also slows gastric emptying, which helps moderate postprandial glucose excursions.
Semaglutide is administered either as a once-weekly subcutaneous injection (Ozempic 0.25–2 mg, Wegovy 0.25–2.4 mg) or as a daily oral tablet (Rybelsus 3–14 mg). Both injectable formulations require gradual dose titration to minimize gastrointestinal side effects. Rybelsus must be taken on an empty stomach with a small sip of water (no more than 4 ounces), at least 30 minutes before eating, drinking, or taking other medications. The injectable formulations have gained particular attention due to their efficacy in producing substantial weight loss—about 15% of body weight on average in pivotal trials—alongside improvements in cardiovascular risk factors. Wegovy is also FDA-approved to reduce the risk of cardiovascular events in adults with established cardiovascular disease and either overweight or obesity.
Important safety considerations include a boxed warning for risk of thyroid C-cell tumors (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2). Other significant warnings include risks of pancreatitis, gallbladder disease, acute kidney injury with dehydration, diabetic retinopathy complications, and hypoglycemia when combined with insulin or sulfonylureas. Semaglutide may also cause a small increase in resting heart rate.
Clinical trial data consistently demonstrate that semaglutide is associated with reductions in systolic blood pressure, rather than increases. The SUSTAIN clinical trial program, which evaluated semaglutide in patients with type 2 diabetes, showed average systolic blood pressure reductions of 3–7 mmHg across multiple studies, with smaller decreases in diastolic blood pressure. The STEP trials, focusing on weight management in patients with obesity, similarly reported systolic blood pressure decreases of 4–8 mmHg with semaglutide 2.4 mg compared to placebo.
The blood pressure-lowering effect appears to be primarily mediated through weight loss. As patients lose significant body weight on semaglutide, multiple cardiovascular parameters improve, including blood pressure, lipid profiles, and inflammatory markers. Weight reduction decreases cardiac workload, improves insulin sensitivity, and reduces activation of the sympathetic nervous system and renin-angiotensin-aldosterone system—all mechanisms that contribute to lower blood pressure readings.
The SELECT cardiovascular outcomes trial provided additional evidence of semaglutide's cardiovascular benefits. This landmark study of over 17,000 adults with established cardiovascular disease and overweight or obesity without diabetes demonstrated a 20% reduction in major adverse cardiovascular events with semaglutide 2.4 mg compared to placebo. Blood pressure improvements were observed alongside these cardiovascular benefits. For patients with type 2 diabetes, the SUSTAIN-6 trial similarly showed cardiovascular benefits with semaglutide treatment.
It is important to note that there is no established causal link between semaglutide and hypertension development. While individual patients may experience blood pressure fluctuations for various reasons during treatment (including dehydration, medication changes, pain, or stress), the preponderance of evidence indicates that semaglutide typically has neutral-to-beneficial effects on blood pressure control. Semaglutide does cause a small increase in resting heart rate (2–4 beats per minute on average), which should be monitored but rarely requires intervention. Any blood pressure elevations observed during semaglutide therapy should prompt evaluation for alternative causes rather than automatic attribution to the medication itself.
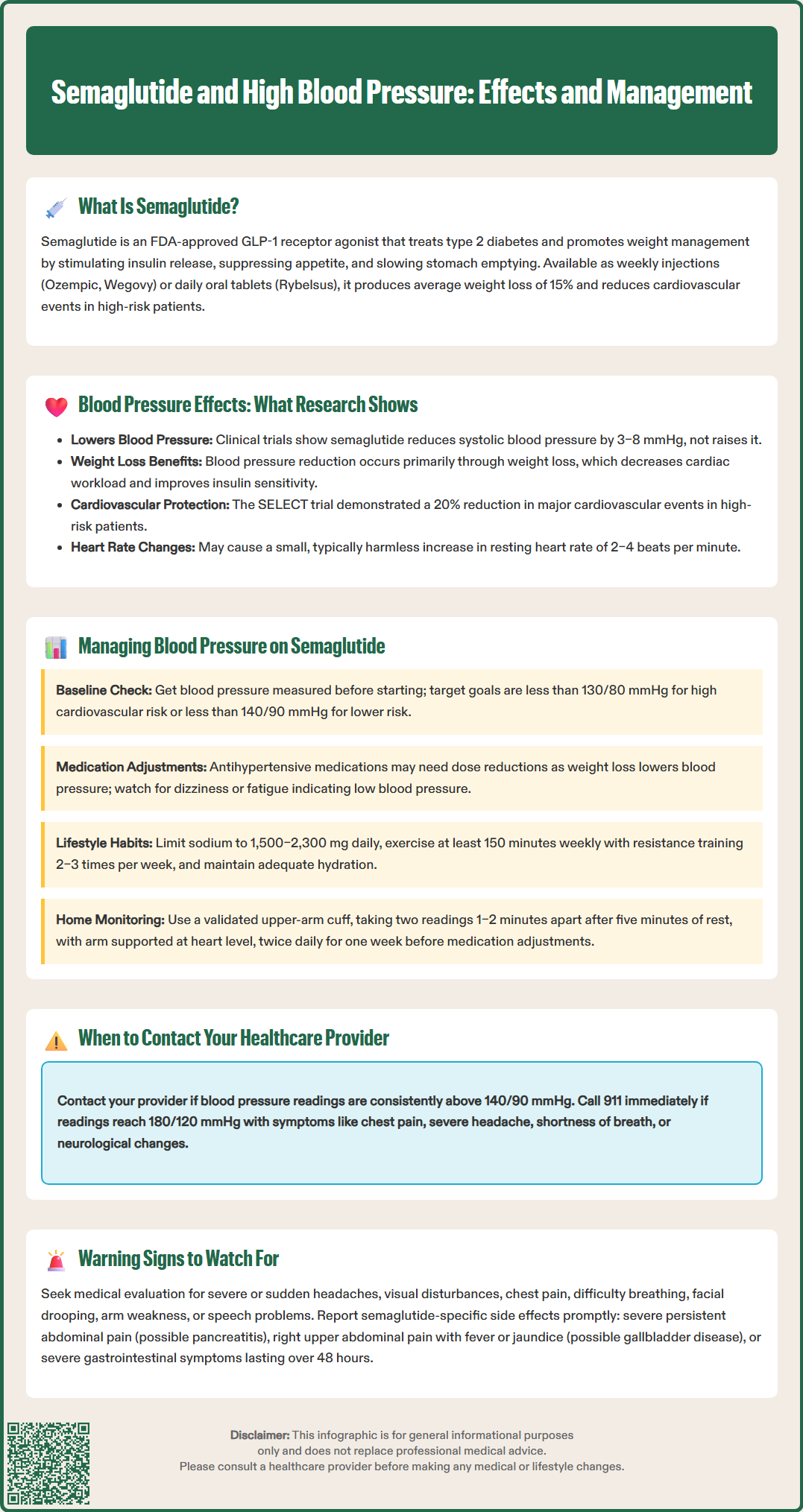
Patients initiating semaglutide therapy should undergo baseline blood pressure assessment as part of comprehensive cardiovascular risk evaluation. The American Diabetes Association recommends blood pressure targets of less than 130/80 mmHg for most adults with diabetes at high cardiovascular risk if safely attainable, and less than 140/90 mmHg for those at lower risk. Individualized goals may be appropriate based on age, comorbidities, and overall cardiovascular risk profile. Blood pressure should be checked at every clinical visit, and structured home blood pressure monitoring is encouraged for ongoing assessment.
For patients with pre-existing hypertension taking antihypertensive medications, semaglutide-associated weight loss may necessitate medication adjustments. As blood pressure decreases with weight reduction, some patients may experience symptoms of relative hypotension, including dizziness, lightheadedness, or fatigue. Healthcare providers should proactively monitor for these symptoms and consider reducing antihypertensive doses when appropriate. Diuretics and medications affecting the renin-angiotensin system are particularly likely to require adjustment as metabolic improvements occur. Monitoring electrolytes and renal function is advisable during significant weight loss or when gastrointestinal side effects are prominent.
Lifestyle modifications remain foundational for blood pressure management during semaglutide therapy. Patients should be counseled on:
Dietary sodium restriction to 1,500–2,300 mg daily for those with hypertension
Regular physical activity with at least 150 minutes of moderate-intensity aerobic exercise weekly, plus resistance training 2–3 days per week
Reducing prolonged sitting by breaking up sedentary time throughout the day
Adequate hydration, particularly important given semaglutide's gastrointestinal effects
Alcohol moderation to no more than one drink daily for women and two for men
Stress management techniques including mindfulness and adequate sleep
Patients should be educated about proper home blood pressure monitoring techniques if self-monitoring is recommended. Measurements should be taken using a validated upper-arm cuff device of appropriate size, after five minutes of rest, with the arm supported at heart level. Two readings should be taken 1–2 minutes apart, twice daily for a week before clinical decisions are made. For patients experiencing dizziness, orthostatic blood pressure measurements (sitting and standing) may be helpful. Keeping a blood pressure log facilitates meaningful discussions during follow-up appointments and helps identify patterns requiring intervention.
Patients taking semaglutide should contact their healthcare provider promptly if they experience sustained blood pressure elevations. Specifically, readings consistently above 140/90 mmHg on multiple occasions warrant medical attention. For non-urgent elevations, patients should confirm with repeated measurements (two readings 1–2 minutes apart) over several days before seeking care.
If blood pressure is 180/120 mmHg or higher without symptoms, patients should recheck after a few minutes and seek same-day medical evaluation if still elevated. However, if this severe elevation is accompanied by symptoms such as chest pain, severe headache, shortness of breath, neurological symptoms, or confusion, patients should call 911 immediately as this represents a hypertensive emergency requiring urgent treatment.
Symptoms potentially related to blood pressure changes require clinical assessment. These include:
Severe headaches, particularly if sudden-onset or different from usual patterns
Visual disturbances such as blurred vision or seeing spots
Chest pain or pressure, which may indicate cardiovascular complications (call 911)
Shortness of breath or difficulty breathing, especially with exertion (call 911 if severe)
Neurological symptoms including facial drooping, arm weakness, speech difficulties (call 911)
Severe dizziness or lightheadedness, particularly upon standing (suggesting hypotension)
Nosebleeds that are difficult to control
Confusion or difficulty concentrating
Patients should also promptly report semaglutide-specific concerns that may require immediate evaluation:
Severe, persistent abdominal pain (possible pancreatitis)
Right upper quadrant pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Signs of allergic reaction including rash, swelling, or difficulty breathing
New or worsening vision problems (potential diabetic retinopathy complications)
Persistent nausea, vomiting, or diarrhea can lead to dehydration, electrolyte imbalances, and secondary blood pressure changes. Severe gastrointestinal symptoms lasting more than 48 hours, inability to maintain adequate oral intake, or signs of dehydration (decreased urine output, extreme thirst, dry mucous membranes) require prompt evaluation.
Regular follow-up appointments are essential for monitoring treatment response and safety. Patients should attend scheduled visits for blood pressure checks, metabolic panel assessments (including renal function and electrolytes), and evaluation of diabetes control through hemoglobin A1c testing. Any concerns about medication tolerability, unexpected symptoms, or questions about blood pressure management should be discussed with the healthcare team rather than discontinuing therapy independently. Collaborative care between patients and providers optimizes both the safety and efficacy of semaglutide treatment while ensuring appropriate cardiovascular risk management.
No, semaglutide does not typically raise blood pressure. Clinical trials consistently show that semaglutide lowers systolic blood pressure by 3–8 mmHg on average, primarily through weight loss and metabolic improvements.
Yes, patients with high blood pressure can take semaglutide. In fact, semaglutide may help lower blood pressure through weight loss. However, antihypertensive medications may need adjustment as blood pressure improves during treatment, so regular monitoring is essential.
Blood pressure readings of 180/120 mmHg or higher require same-day medical evaluation. If this severe elevation is accompanied by chest pain, severe headache, shortness of breath, or neurological symptoms, call 911 immediately as this represents a hypertensive emergency.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.