LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many women navigating menopause wonder: can you take weight loss injections with HRT? As FDA-approved GLP-1 medications like semaglutide (Wegovy) and tirzepatide (Zepbound) become more widely prescribed for chronic weight management, understanding their compatibility with hormone replacement therapy is increasingly important. Currently, no official contraindication exists for combining these therapies, and many healthcare providers prescribe them together when clinically appropriate. However, the decision requires careful individualized assessment, considering each medication's risk profile, potential interactions, and your complete medical history. This article examines the safety considerations, potential interactions, and medical guidance for women considering both treatments simultaneously.
Quick Answer: There is no official contraindication to using GLP-1 or GIP/GLP-1 weight loss injections concurrently with hormone replacement therapy, and many healthcare providers prescribe them together when clinically appropriate.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections approved by the FDA for chronic weight management include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonist tirzepatide (Zepbound). These medications work by mimicking natural hormones that regulate appetite and blood sugar levels, slowing gastric emptying and promoting satiety. It's important to note that while Wegovy and Zepbound are FDA-approved for chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity, similar medications like Ozempic (semaglutide) and Mounjaro (tirzepatide) are approved only for type 2 diabetes management.
Hormone replacement therapy (HRT) encompasses various formulations of estrogen, progesterone, or combination therapies used primarily to manage menopausal symptoms such as hot flashes, night sweats, and vaginal dryness. HRT may be administered through FDA-approved oral tablets, transdermal patches, topical gels, or vaginal preparations. Some women use compounded bioidentical hormone pellets, though these are not FDA-approved and lack the same safety and efficacy evidence as regulated products. Many women experience weight changes during the menopausal transition, which can be attributed to hormonal changes, aging, and lifestyle factors.
The intersection of these two treatment categories has become clinically relevant as more perimenopausal and postmenopausal women seek solutions for weight management while managing menopausal symptoms. Understanding how these medications function independently provides essential context for evaluating their combined use. Both medication classes influence metabolic processes, though through different mechanisms, making it important to consider potential interactions and cumulative effects on the body's hormonal and metabolic systems.
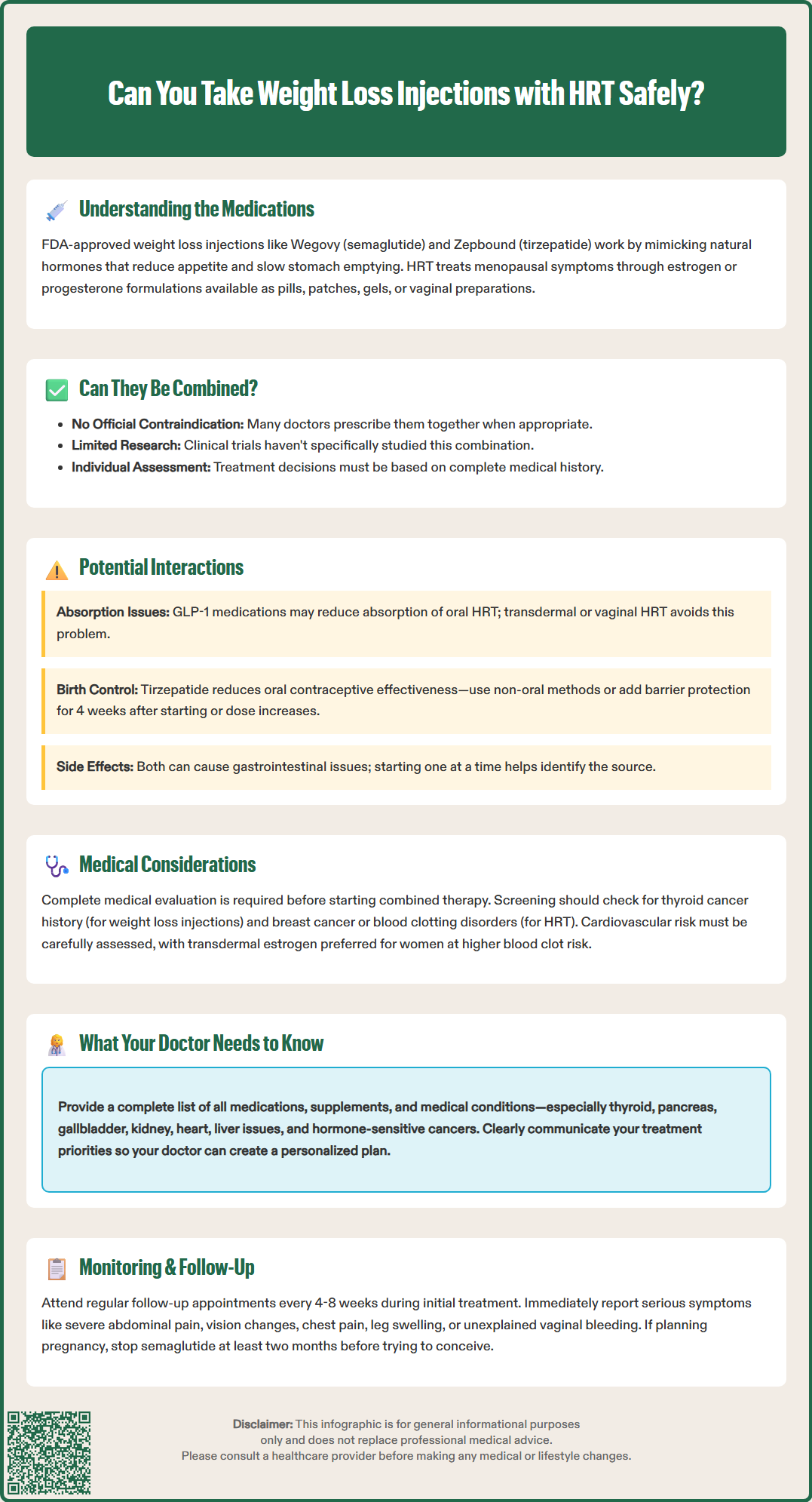
There is currently no official contraindication to using GLP-1 receptor agonists or GIP/GLP-1 receptor agonist weight loss injections concurrently with hormone replacement therapy. The FDA-approved prescribing information for semaglutide and tirzepatide does not list HRT as a contraindication, and no direct pharmacological interaction between these medication classes has been established in clinical trials. Many healthcare providers do prescribe these therapies together when clinically appropriate.
However, the absence of a documented contraindication does not automatically mean the combination is without considerations. Clinical trials for weight loss injections have generally not specifically studied populations using HRT, creating a gap in evidence-based guidance. Most safety data comes from real-world clinical experience rather than controlled studies examining this specific combination.
Both medication classes carry their own risk profiles that require consideration. GLP-1 and GIP/GLP-1 medications have boxed warnings regarding thyroid C-cell tumors (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2) and carry risks of pancreatitis, gallbladder disease, and diabetic retinopathy progression. HRT carries risks including venous thromboembolism (VTE), with transdermal estrogen generally associated with lower VTE risk than oral formulations.
The decision to use both therapies should be individualized, considering the patient's complete medical history, current health status, and treatment goals. Women with certain medical histories—including previous blood clots, cardiovascular disease, liver disease, or hormone-sensitive cancers—require particularly careful evaluation.
Healthcare providers typically assess the risk-benefit ratio for each patient individually. For many women experiencing both menopausal symptoms and obesity, the benefits of addressing both conditions may outweigh potential risks, particularly when appropriate monitoring is in place. Close medical supervision during the initial treatment period allows for early identification of any unexpected effects.
While direct pharmacokinetic interactions between GLP-1/GIP medications and HRT are not well-documented, several considerations warrant attention. GLP-1 and GIP/GLP-1 medications significantly slow gastric emptying, which can affect the absorption of oral medications, including oral estrogen or progesterone formulations. FDA labeling for semaglutide specifically notes that delayed gastric emptying may impact absorption of concomitant oral medications. This altered absorption pattern could theoretically affect symptom control, though clinical significance remains unclear.
For women using oral HRT, monitoring menopausal symptom control after initiating GLP-1/GIP therapy is advisable. Transdermal, vaginal, or other non-oral HRT formulations bypass the gastrointestinal tract entirely, eliminating this potential concern. Healthcare providers may consider non-oral HRT routes for women starting GLP-1/GIP therapy, particularly if symptom control becomes inconsistent.
Tirzepatide has a specific labeled interaction with oral contraceptives, reducing their exposure. While this is not specific to HRT, it has implications for women using these medications. Women using tirzepatide with oral contraceptives should use non-oral contraception or add a barrier method for 4 weeks after initiation and after each dose increase.
Both medication classes can influence metabolic parameters, though through different mechanisms. Weight loss achieved through GLP-1/GIP therapy may improve insulin sensitivity and lipid profiles, potentially complementing some beneficial metabolic effects of HRT. Conversely, estrogen therapy can affect glucose metabolism and insulin sensitivity, though effects vary based on formulation, dose, and route of administration.
Gastrointestinal side effects represent another consideration. GLP-1/GIP medications commonly cause nausea, vomiting, diarrhea, and constipation, particularly during dose escalation. Some women experience similar gastrointestinal symptoms when initiating oral HRT. When starting both therapies simultaneously or in close succession, distinguishing which medication causes side effects becomes challenging, potentially complicating management decisions. Staggered initiation—starting one medication and achieving stable dosing before introducing the second—may help identify the source of any adverse effects and improve tolerability.
Before initiating combined therapy with weight loss injections and HRT, comprehensive medical evaluation is essential. A thorough personal and family medical history should identify contraindications to either therapy, including history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2 (contraindications to GLP-1/GIP therapy), and history of breast cancer, endometrial cancer, unexplained vaginal bleeding, active liver disease, or thromboembolic disease (potential contraindications to HRT).
Baseline laboratory investigations should be targeted based on individual risk factors and medical history rather than routine comprehensive panels. Relevant tests may include fasting glucose and hemoglobin A1c to assess glycemic status, lipid panel, and liver and renal function tests as clinically indicated. For women considering HRT, age-appropriate breast cancer screening per USPSTF guidelines is recommended, rather than mandatory pre-HRT mammography. Pelvic examination and endometrial assessment may be indicated based on clinical presentation.
Cardiovascular risk assessment deserves particular attention when combining these therapies. While GLP-1/GIP medications have demonstrated cardiovascular benefits in some populations, HRT's cardiovascular effects vary based on timing of initiation, formulation, and individual risk factors. For women at higher risk of venous thromboembolism, transdermal estrogen is generally preferred over oral formulations. Women with an intact uterus who use systemic estrogen therapy require adequate progestogen for endometrial protection.
Patients should understand realistic expectations for both therapies. Weight loss injections typically produce gradual weight reduction of 10-15% of body weight over 12-18 months when combined with lifestyle modifications. Early efficacy assessment at 12-16 weeks helps determine whether to continue therapy. HRT effectively manages vasomotor symptoms but is not indicated for weight management, and its effects on weight are small and inconsistent. Setting appropriate expectations prevents disappointment and supports treatment adherence.
Women should also understand the commitment required, including regular follow-up appointments, potential side effects, and the importance of lifestyle modifications including nutrition and physical activity.
Transparent communication with healthcare providers is crucial when considering or using both weight loss injections and HRT. Patients should provide a complete medication list, including all prescription medications, over-the-counter drugs, supplements, and herbal products. This comprehensive inventory helps identify potential interactions and ensures coordinated care.
Inform your doctor about all current and past medical conditions, particularly thyroid disorders, pancreatitis, gallbladder disease, kidney disease, diabetic retinopathy, cardiovascular disease, liver disease, and any history of hormone-sensitive cancers. Previous experiences with either medication class, including any adverse reactions or treatment failures, guide current prescribing decisions. Family history of medullary thyroid cancer, multiple endocrine neoplasia, breast cancer, or thromboembolic disease also influences risk assessment.
Your healthcare provider needs to know your treatment goals and priorities. Are menopausal symptoms significantly impacting quality of life? Is weight loss the primary concern, or are you addressing obesity-related comorbidities such as type 2 diabetes or hypertension? Understanding your priorities helps your doctor develop an individualized treatment plan that addresses your most pressing health concerns.
Regular monitoring is essential when using both therapies. Follow-up appointments may occur every 4-8 weeks during initial titration of weight loss medications, with efficacy assessment at 12-16 weeks to determine whether to continue therapy. Report new or worsening symptoms promptly, including severe abdominal pain (potential pancreatitis), visual changes, chest pain, leg swelling or pain (potential thrombosis), unexplained vaginal bleeding, or persistent gastrointestinal symptoms. Your doctor should coordinate care if you see multiple specialists, ensuring all providers are aware of your complete treatment regimen.
Patients should discuss their plans if considering pregnancy. For semaglutide, FDA labeling recommends discontinuation at least two months before attempting conception. While tirzepatide labeling does not specify a preconception interval, it should be discontinued prior to planned pregnancy with timing discussed with your healthcare provider. Women using tirzepatide should be aware that it reduces the exposure of oral contraceptives; non-oral contraception or additional barrier methods are recommended for 4 weeks after initiation and dose increases. Weight loss can affect fertility, so contraceptive needs should be addressed even if pregnancy is not immediately planned.
No direct pharmacological interactions have been established between GLP-1/GIP weight loss medications and HRT. However, GLP-1 medications slow gastric emptying, which may affect absorption of oral HRT formulations, though transdermal or vaginal HRT routes bypass this concern entirely.
Yes, regular follow-up appointments are recommended, typically every 4-8 weeks during initial dose titration of weight loss medications. Patients should promptly report severe abdominal pain, visual changes, chest pain, leg swelling, unexplained vaginal bleeding, or persistent gastrointestinal symptoms to their healthcare provider.
Staggered initiation—starting one medication and achieving stable dosing before introducing the second—may help identify the source of any side effects and improve tolerability. This approach is particularly helpful since both therapies can cause gastrointestinal symptoms, making it difficult to determine which medication is responsible when started simultaneously.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.