LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is an FDA-approved medication for type 2 diabetes and chronic weight management that commonly causes gastrointestinal side effects. While nausea, diarrhea, and constipation are well-documented reactions, some patients report noticing mucus in stool during treatment. Although mucus in stool is not specifically listed as a recognized adverse effect in FDA prescribing information, understanding how tirzepatide affects digestive function helps patients and clinicians determine whether symptoms require medical evaluation. This article examines the potential relationship between tirzepatide therapy and changes in stool characteristics, including when to seek medical attention.
Quick Answer: Mucus in stool is not a recognized adverse effect of tirzepatide, though the medication's gastrointestinal effects may theoretically make intestinal mucus more visible.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). This once-weekly injectable medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, and slowing gastric emptying, which collectively improve glycemic control and promote weight loss.
Gastrointestinal side effects are among the most commonly reported adverse reactions with tirzepatide therapy. Clinical trials have demonstrated that nausea, diarrhea, vomiting, constipation, and abdominal discomfort occur frequently, particularly during dose initiation and escalation. These effects result primarily from the medication's mechanism of slowing gastric motility. According to FDA prescribing information, gastrointestinal adverse events led to treatment discontinuation in approximately 4-7% of patients in clinical trials, with rates varying by dose and indication.
While the FDA label and clinical literature extensively document common digestive symptoms, mucus in stool is not specifically listed as a recognized adverse effect of tirzepatide. However, patients taking this medication may notice changes in bowel habits and stool characteristics due to altered gastrointestinal transit time and digestive processes. Understanding the relationship between tirzepatide's pharmacological effects and potential bowel changes helps patients and clinicians distinguish between expected medication effects and symptoms requiring further evaluation.
The gastrointestinal tolerability profile of tirzepatide generally improves over time as the body adapts to the medication, though individual responses vary considerably. Proper patient education regarding anticipated digestive effects supports medication adherence and appropriate symptom management. It's important to note that tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Additionally, tirzepatide has not been studied in patients with severe gastrointestinal disease, including severe gastroparesis.
There is no established direct causal link between tirzepatide and mucus in stool based on current clinical evidence. However, several mechanisms related to the medication's gastrointestinal effects may theoretically contribute to changes in stool appearance, including increased mucus production or visibility.
Tirzepatide significantly slows gastric emptying, which represents a core component of its therapeutic mechanism. This effect is most pronounced after initiation and may diminish somewhat with chronic use. While the medication's primary effect is on gastric emptying, it may theoretically influence intestinal transit as well, potentially altering the intestinal environment and affecting the normal balance of digestive secretions. The intestinal mucosa naturally produces mucus as a protective barrier, and changes in transit time might make this mucus more apparent in stool.
Diarrhea, which occurs in approximately 15-23% of patients taking tirzepatide (with higher rates at higher doses and in the weight management indication), can independently cause visible mucus in stool. When intestinal transit accelerates during diarrheal episodes, the normal reabsorption of intestinal secretions decreases, and protective mucus may become more prominent. Some patients may theoretically experience changes in intestinal secretions or sensitivity as the digestive system adapts to the medication, though this mechanism remains speculative without specific clinical evidence.
It is important to recognize that mucus in stool can result from numerous conditions unrelated to tirzepatide therapy, including irritable bowel syndrome, inflammatory bowel disease, infections, food intolerances, and other gastrointestinal disorders. The temporal relationship between medication initiation and symptom onset provides important diagnostic information, but does not confirm causation. Patients experiencing this symptom should consider both medication-related and independent gastrointestinal causes, particularly if mucus is accompanied by other concerning features such as blood, significant abdominal pain, or persistent changes in bowel habits.
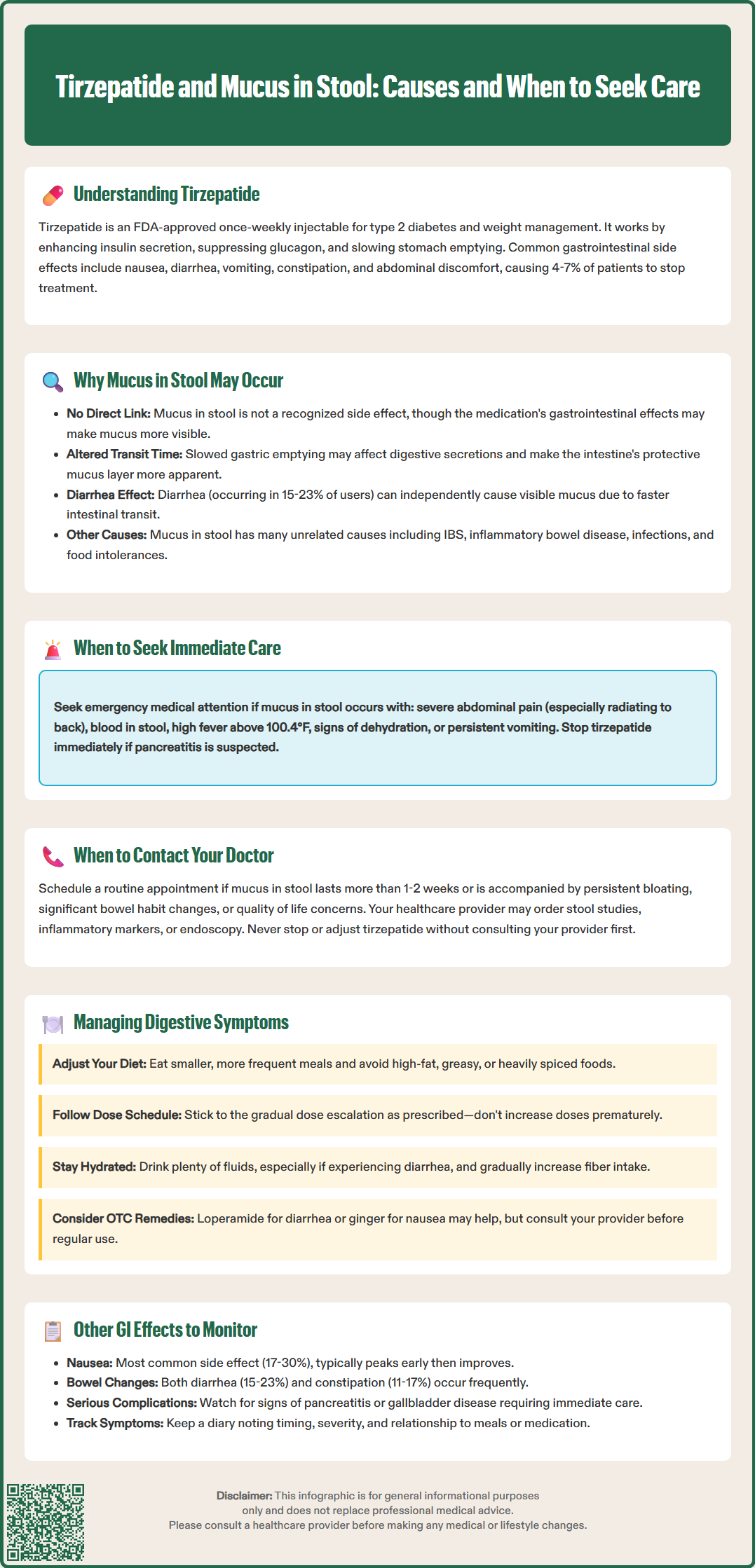
While mild gastrointestinal symptoms are common with tirzepatide and often resolve with continued therapy, certain presentations warrant prompt medical evaluation. Patients should contact their healthcare provider if mucus in stool is accompanied by any of the following warning signs:
Immediate medical attention is recommended for:
Severe, persistent abdominal pain, especially if radiating to the back or accompanied by nausea/vomiting (possible pancreatitis)
Blood in stool (red blood or black, tarry stools)
Right upper quadrant pain, especially with fever or yellowing of skin/eyes (possible gallbladder disease)
Fever above 100.4°F (38°C)
Signs of dehydration (decreased urination, dizziness, extreme thirst, dry mouth)
Unintentional weight loss beyond expected therapeutic effects
Persistent vomiting preventing adequate fluid intake
Schedule a routine appointment if experiencing:
Mucus in stool persisting beyond 1-2 weeks
Significant changes in bowel habits (frequency, consistency, or appearance)
Mucus accompanied by persistent bloating or discomfort
New onset of symptoms after stable medication tolerance
Concerns about symptom severity or impact on quality of life
Healthcare providers will typically conduct a thorough clinical assessment including detailed history, physical examination, and potentially laboratory investigations. Stool studies may be indicated to exclude infectious causes, particularly if diarrhea is prominent. Inflammatory markers such as C-reactive protein or fecal calprotectin can help identify inflammatory bowel conditions. In some cases, endoscopic evaluation may be necessary to visualize the intestinal mucosa directly and obtain tissue samples.
Patients should stop tirzepatide immediately and seek urgent medical care if pancreatitis is suspected. For other concerns, patients should consult their healthcare provider before making medication changes, as adjustments may affect glycemic control in diabetes management. Healthcare providers can assess whether symptoms represent expected medication effects, require symptomatic management, warrant dose adjustment, or indicate an unrelated condition requiring specific treatment. Documentation of symptom timing, severity, and associated features assists clinical decision-making and ensures appropriate care.
Effective management of gastrointestinal symptoms during tirzepatide therapy involves both pharmacological strategies and lifestyle modifications. These approaches can improve tolerability and support medication adherence while maintaining therapeutic benefits.
Dietary modifications represent the cornerstone of symptom management. Patients should consider eating smaller, more frequent meals rather than large portions, as this approach accommodates the medication's effect on gastric emptying. Avoiding high-fat, greasy, or heavily spiced foods reduces gastrointestinal irritation and may decrease nausea and diarrhea. Adequate fiber intake from sources like vegetables, fruits, and whole grains supports healthy bowel function, though patients should increase fiber gradually to avoid bloating. Maintaining appropriate hydration is essential, particularly if experiencing diarrhea or mucus in stool, with fluid intake individualized based on health status, activity level, and climate.
Medication timing and dosing strategies can significantly impact tolerability. Tirzepatide is administered once weekly on the same day each week and can be taken any time of day, with or without food. The FDA-approved dosing schedule includes gradual dose escalation specifically designed to improve gastrointestinal tolerability. Patients should not advance to higher doses prematurely, even if glycemic or weight loss goals have not yet been achieved. Some clinicians may recommend slower titration schedules for patients experiencing significant symptoms.
Symptomatic treatments may provide relief for specific gastrointestinal complaints. Over-the-counter antidiarrheal medications like loperamide can be used judiciously for diarrhea (avoiding use if fever, blood in stool, or infection is suspected), though patients should consult their healthcare provider before regular use. Probiotics may support gut health, though evidence for their efficacy in medication-induced gastrointestinal symptoms remains limited. Anti-nausea strategies including ginger, acupressure, or prescribed antiemetics may benefit patients with prominent nausea.
Patients should maintain open communication with their healthcare team regarding symptom severity and impact on daily functioning. Women of childbearing potential should be aware that tirzepatide may reduce the effectiveness of oral hormonal contraceptives, particularly after initiation or dose increases, and should consider using non-oral or additional contraceptive methods. Persistent or severe symptoms may warrant dose reduction, temporary treatment interruption, or consideration of alternative therapeutic options. Many patients find that gastrointestinal side effects tend to improve as their body adjusts to a stable dose.
Beyond mucus in stool, tirzepatide therapy is associated with a spectrum of gastrointestinal effects that patients and clinicians should monitor throughout treatment. Understanding these potential adverse reactions enables early recognition and appropriate management.
Nausea represents the most frequently reported gastrointestinal side effect, occurring in approximately 17-30% of patients depending on dose and indication, with higher rates typically seen at higher doses and in the weight management indication. This symptom typically peaks during the first few weeks after initiation or dose escalation and generally diminishes with continued therapy. Severe or persistent nausea may impair nutritional intake and quality of life, warranting intervention. Patients should report nausea that prevents adequate food or fluid consumption, as this may lead to dehydration or nutritional deficiencies.
Diarrhea and constipation both occur commonly with tirzepatide, reflecting the medication's complex effects on gastrointestinal motility. Diarrhea affects 15-23% of patients and may range from mild loose stools to frequent watery bowel movements. Conversely, constipation occurs in approximately 11-17% of patients, likely related to delayed gastric emptying. Alternating bowel habits may occur as the gastrointestinal system adapts to medication effects.
Abdominal pain and dyspepsia are reported in 6-10% of patients. These symptoms may manifest as upper abdominal discomfort, bloating, early satiety, or generalized cramping. While usually mild to moderate, severe or persistent abdominal pain requires evaluation to exclude serious complications.
Serious gastrointestinal complications require vigilant monitoring. Acute pancreatitis has been reported with tirzepatide use. Patients should immediately discontinue tirzepatide and seek urgent medical care for severe, persistent abdominal pain radiating to the back, particularly if accompanied by nausea and vomiting. Gallbladder disease, including cholelithiasis and cholecystitis, has been observed with tirzepatide therapy. Patients should promptly report right upper quadrant pain, fever, or jaundice for evaluation. Severe gastrointestinal adverse reactions may lead to dehydration and acute kidney injury, particularly in patients with pre-existing renal impairment, requiring close monitoring of fluid status and kidney function.
Regular follow-up appointments allow healthcare providers to assess gastrointestinal tolerability, adjust management strategies, and ensure that the benefits of tirzepatide therapy continue to outweigh any adverse effects. Patients should maintain symptom diaries when experiencing persistent gastrointestinal issues, documenting timing, severity, and relationship to meals or medication administration.
Mucus in stool is not specifically listed as a recognized adverse effect in tirzepatide's FDA prescribing information. However, the medication's effects on gastrointestinal motility and common side effects like diarrhea may theoretically make intestinal mucus more visible in some patients.
Contact your healthcare provider immediately if mucus in stool is accompanied by blood, severe abdominal pain, fever above 100.4°F, signs of dehydration, or persistent vomiting. Schedule a routine appointment if mucus persists beyond 1-2 weeks or is accompanied by significant changes in bowel habits.
The most common gastrointestinal side effects include nausea (17-30% of patients), diarrhea (15-23%), constipation (11-17%), vomiting, and abdominal discomfort. These effects typically occur during dose initiation or escalation and often improve as the body adapts to the medication.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.