LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do GLP-1 medications make you tired? Fatigue is a reported side effect for some GLP-1 receptor agonists, particularly at higher doses used for weight management. While not universally experienced, tiredness can occur through several mechanisms—including reduced caloric intake, gastrointestinal symptoms, and rapid metabolic changes. Understanding whether your fatigue stems directly from the medication or from secondary effects like inadequate nutrition or dehydration is essential for appropriate management. This article examines the relationship between GLP-1 therapy and tiredness, explores contributing factors, and provides practical strategies to maintain energy levels while benefiting from treatment.
Quick Answer: GLP-1 medications can cause tiredness in some patients, primarily through reduced caloric intake, gastrointestinal side effects, and rapid metabolic changes rather than direct drug effects.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Fatigue is listed as a reported adverse reaction for some GLP-1 receptor agonists, particularly those used at higher doses for weight management such as semaglutide (Wegovy) and liraglutide (Saxenda). In other GLP-1 medications like Ozempic, Trulicity, or Victoza, fatigue is less frequently reported or not specifically listed as a common side effect in FDA prescribing information. Beyond clinical trial data, many patients report feeling tired or experiencing low energy when starting or adjusting doses of these medications.
The relationship between GLP-1 medications and tiredness may involve both direct and indirect mechanisms. GLP-1 receptor agonists work by mimicking the incretin hormone glucagon-like peptide-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety. While these primary mechanisms don't necessarily cause fatigue directly, the downstream effects—particularly reduced caloric intake and gastrointestinal symptoms—may contribute to feelings of tiredness in some individuals.
It's important to distinguish between medication side effects and secondary consequences of treatment. The physiological changes that accompany GLP-1 therapy can create conditions where tiredness becomes more noticeable. Understanding this distinction helps patients and clinicians address fatigue appropriately, whether through medication adjustment, nutritional support, or investigation of alternative causes. If you experience persistent or severe fatigue while taking a GLP-1 medication, this symptom should be evaluated in the context of your overall health status and treatment goals.
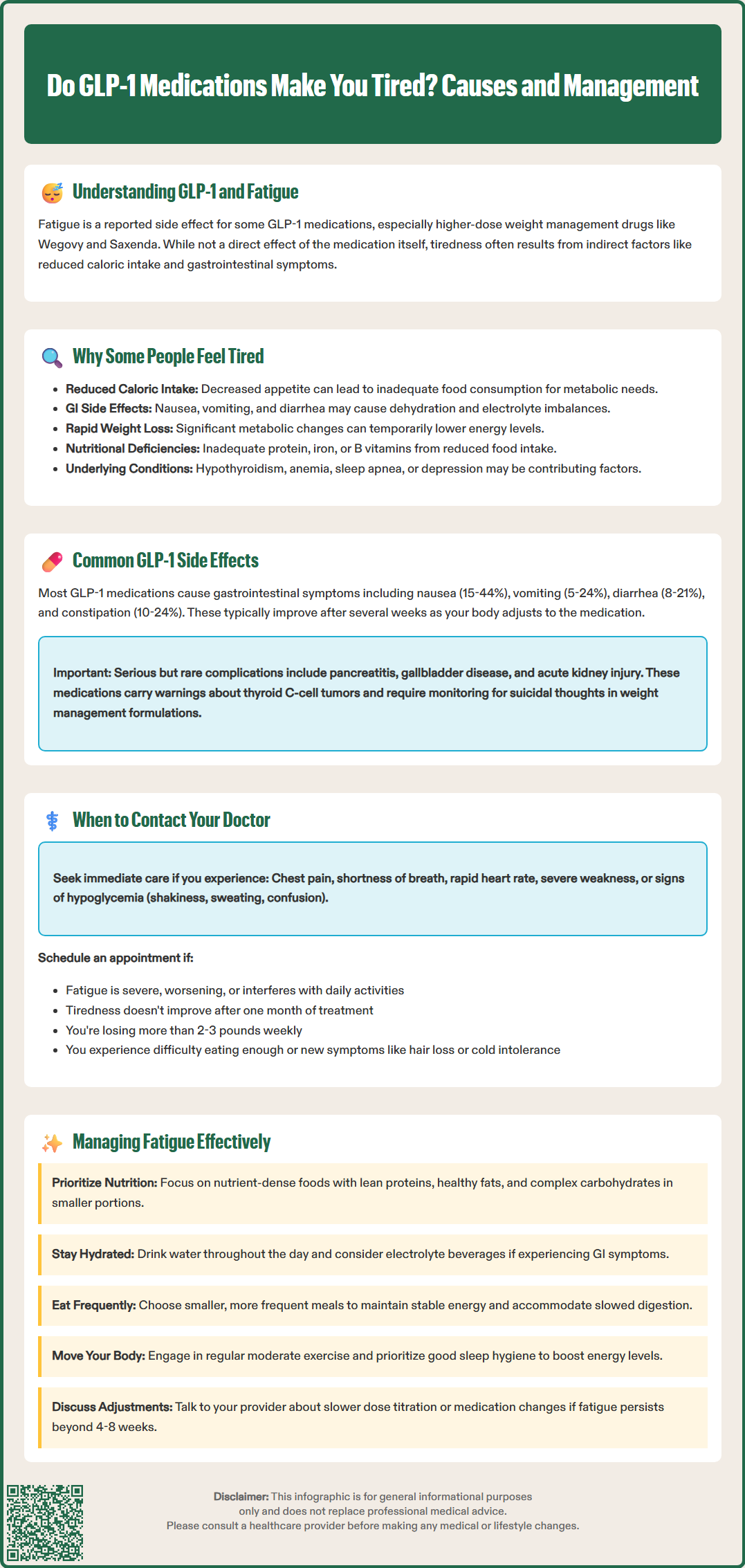
Several mechanisms may explain why some patients experience tiredness while taking GLP-1 receptor agonists. The most common contributor is likely reduced caloric intake. These medications significantly decrease appetite and promote early satiety, often leading to substantial reductions in daily food consumption. When caloric intake drops too quickly or becomes inadequate to meet metabolic needs, fatigue naturally follows. This is particularly relevant for patients using higher doses or those who experience pronounced appetite suppression.
Gastrointestinal side effects represent another important factor. Nausea, vomiting, and diarrhea—the most frequently reported adverse effects of GLP-1 medications—can lead to dehydration, electrolyte imbalances, and poor nutrient absorption. These conditions commonly manifest as tiredness or weakness. The slowed gastric emptying that contributes to satiety may also cause prolonged feelings of fullness or discomfort, potentially disrupting normal eating patterns and sleep quality.
Rapid weight loss itself can contribute to fatigue, independent of the medication mechanism. As the body adapts to significant caloric restriction and metabolic changes, temporary periods of low energy may occur. Additionally, some patients may possibly develop nutritional deficiencies—particularly in protein, iron, or B vitamins—if their reduced food intake is not nutritionally balanced. This risk is especially relevant for patients who were already at risk for deficiencies before starting treatment.
Hypoglycemia may occur in patients taking GLP-1 medications alongside insulin or sulfonylureas, though GLP-1 agonists alone carry minimal hypoglycemia risk due to their glucose-dependent mechanism. When blood glucose drops too low, fatigue, weakness, and confusion are characteristic symptoms. It is also worth considering that fatigue attributed to GLP-1 therapy may actually reflect underlying conditions such as hypothyroidism, anemia, sleep apnea, or depression, which should be evaluated if tiredness persists.
The most frequently reported adverse effects of GLP-1 receptor agonists are gastrointestinal in nature. According to FDA prescribing information, these include:
Nausea (occurring in 15–44% of patients depending on the specific agent and dose)
Vomiting (5–24% of patients)
Diarrhea (8–21% of patients)
Constipation (10–24% of patients)
Abdominal pain or discomfort (5–14% of patients)
These symptoms typically emerge during dose initiation or escalation and often diminish over several weeks as the body adapts. The severity varies considerably among individuals, with some experiencing minimal discomfort while others find these effects significantly impact quality of life.
Injection site reactions are common with subcutaneous formulations, presenting as redness, itching, or mild swelling at the injection site. These reactions are generally mild and self-limiting. Decreased appetite is an expected pharmacological effect rather than an adverse event, though the degree of appetite suppression can be more pronounced than some patients anticipate.
More serious but less common adverse effects require clinical vigilance. Pancreatitis has been reported with GLP-1 receptor agonists. Patients should be counseled to stop the medication and seek immediate medical attention for severe, persistent abdominal pain that may radiate to the back. Gallbladder disease, including cholelithiasis and cholecystitis, occurs more frequently with rapid weight loss and has been observed in clinical trials. Acute kidney injury has been reported, typically in the context of severe dehydration from gastrointestinal side effects.
Additionally, there is a boxed warning regarding thyroid C-cell tumors based on rodent studies, though human relevance remains uncertain. GLP-1 medications are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Diabetic retinopathy complications have been observed primarily with semaglutide, particularly with rapid glucose improvement in patients with pre-existing retinopathy, warranting ophthalmologic monitoring in high-risk individuals. Weight management formulations (Wegovy, Saxenda) also carry warnings about suicidal ideation and behavior.
While mild fatigue during the initial weeks of GLP-1 therapy may resolve as your body adjusts, certain patterns or accompanying symptoms warrant prompt medical evaluation. You should contact your healthcare provider if you experience severe or worsening fatigue that interferes with daily activities or does not improve after the first month of treatment. This may indicate inadequate caloric intake, nutritional deficiencies, or an unrelated medical condition requiring investigation.
Seek immediate medical attention if tiredness is accompanied by:
Symptoms of hypoglycemia: shakiness, sweating, confusion, rapid heartbeat, or dizziness (particularly relevant if you take insulin or sulfonylureas). If you suspect hypoglycemia and can check your blood glucose, follow the ADA's "15-15 rule": take 15 grams of fast-acting carbohydrate, wait 15 minutes, then recheck. Repeat if needed.
Signs of dehydration: decreased urination, dark urine, extreme thirst, dry mouth, or lightheadedness upon standing
Severe gastrointestinal symptoms: persistent vomiting preventing fluid intake, bloody stools, or severe abdominal pain. Hold your GLP-1 medication and seek urgent care if you cannot keep fluids down or suspect pancreatitis.
Chest pain, shortness of breath, or rapid heart rate: which could indicate cardiovascular complications
Severe weakness or inability to perform normal activities: suggesting possible electrolyte imbalances or other serious conditions
You should also schedule a non-urgent appointment if you notice unintentional excessive weight loss (more than 2–3 pounds per week consistently), difficulty maintaining adequate nutrition, or new symptoms such as cold intolerance, hair loss, or mood changes that might suggest thyroid dysfunction or other endocrine issues.
Before your appointment, it may be helpful to track your symptoms: document when fatigue occurs, its severity, associated symptoms, dietary intake, and any patterns you notice. This information assists your physician in determining whether fatigue relates to the medication, requires dose adjustment, or necessitates further diagnostic evaluation. Blood tests to assess glucose control, kidney function, electrolytes, thyroid function, and nutritional markers (such as vitamin B12, iron studies, and complete blood count) may be appropriate depending on your clinical presentation and risk factors.
If you experience tiredness while taking a GLP-1 medication, several strategies may help manage this symptom while maintaining the therapeutic benefits of treatment. Ensure adequate caloric and nutritional intake despite reduced appetite. Focus on nutrient-dense foods that provide essential vitamins, minerals, and macronutrients in smaller volumes. Prioritize lean proteins to preserve muscle mass during weight loss, and include healthy fats and complex carbohydrates to sustain energy levels throughout the day. Consider consulting a registered dietitian who can develop a meal plan tailored to your reduced appetite and nutritional needs.
Stay well-hydrated, particularly if you experience gastrointestinal side effects. Dehydration significantly contributes to fatigue and can be subtle in onset. Aim for adequate fluid intake throughout the day, and consider low-sugar or sugar-free electrolyte-containing beverages if you have persistent diarrhea or vomiting, especially if you have diabetes. Eat smaller, more frequent meals rather than attempting large meals that may be difficult to tolerate with slowed gastric emptying. This approach can help maintain more stable energy levels and reduce gastrointestinal discomfort.
Optimize sleep hygiene and physical activity. Paradoxically, regular moderate exercise can improve energy levels and reduce fatigue, though you may need to adjust intensity during the initial adaptation period. Ensure you get adequate sleep, as poor sleep quality exacerbates tiredness and may worsen other side effects. Communicate with your healthcare provider about dose titration strategies. A slower escalation schedule following FDA-approved titration guidelines may reduce side effects and allow better adaptation, though this must be balanced against therapeutic goals.
If fatigue persists despite these measures, your physician may consider adjusting your medication regimen. This could involve temporarily reducing the dose, switching to a different GLP-1 receptor agonist with a different pharmacokinetic profile, or investigating whether concurrent medications contribute to tiredness. Address underlying conditions that may compound fatigue, such as optimizing thyroid function, treating anemia, or managing sleep disorders. Finally, set realistic expectations: some degree of adjustment is normal when starting these medications, and many patients find that energy levels improve as their bodies adapt to the new metabolic state and side effects diminish, typically within the first 4–8 weeks of treatment.
Most patients experience improvement in fatigue within 4–8 weeks as their bodies adapt to the medication and gastrointestinal side effects diminish. Persistent tiredness beyond this period warrants medical evaluation for nutritional deficiencies or underlying conditions.
While not entirely preventable, you can minimize fatigue by ensuring adequate caloric and protein intake despite reduced appetite, staying well-hydrated, following a gradual dose escalation schedule, and maintaining regular moderate physical activity.
Do not stop your medication without consulting your healthcare provider. Contact your doctor if you experience severe fatigue, especially with symptoms of hypoglycemia, dehydration, persistent vomiting, or inability to perform daily activities, as dose adjustment or further evaluation may be needed.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.