LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections like semaglutide (Wegovy) and tirzepatide (Zepbound) have transformed obesity treatment, yet some patients experience disappointing results despite proper use. Understanding why these FDA-approved GLP-1 receptor agonists may not work as expected requires examining multiple factors—from medication dosing and administration technique to underlying medical conditions and lifestyle behaviors. Individual response varies significantly, with some patients achieving minimal weight reduction even with adherence. This article explores the medical, physiological, and practical reasons behind suboptimal treatment outcomes and when to discuss alternative approaches with your healthcare provider.
Quick Answer: Weight loss injections may not work due to insufficient treatment duration, inadequate dosing, underlying medical conditions, compensatory eating behaviors, improper injection technique, or individual metabolic variation in drug response.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists, work through multiple physiological mechanisms to promote weight reduction. FDA-approved medications for chronic weight management include semaglutide (Wegovy) and tirzepatide (Zepbound), while liraglutide (Saxenda) is another approved option. Note that similar medications like Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved only for diabetes management, not weight loss.
These medications mimic naturally occurring incretin hormones that regulate appetite and glucose metabolism. They primarily bind to GLP-1 receptors in brain areas controlling appetite and satiety. This activation slows gastric emptying, keeping food in the stomach longer and creating prolonged feelings of fullness. Simultaneously, these agents reduce hunger signals from the hypothalamus, decreasing overall caloric intake. GLP-1 receptor agonists also enhance insulin secretion while suppressing inappropriate glucagon release, helping stabilize blood sugar levels and reducing cravings.
Tirzepatide offers dual action by activating both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors. Clinical trials demonstrate that semaglutide can produce approximately 15% body weight reduction over 68 weeks, while tirzepatide can achieve about 21% reduction over 72 weeks when combined with lifestyle modifications in people without diabetes.
The effectiveness of these injections depends on consistent receptor activation, appropriate dosing escalation, and adequate time for physiological adaptation. Most patients begin noticing appetite suppression within the first few weeks, though maximum weight loss typically occurs after several months of treatment. It's important to note that weight regain is common if treatment is discontinued.
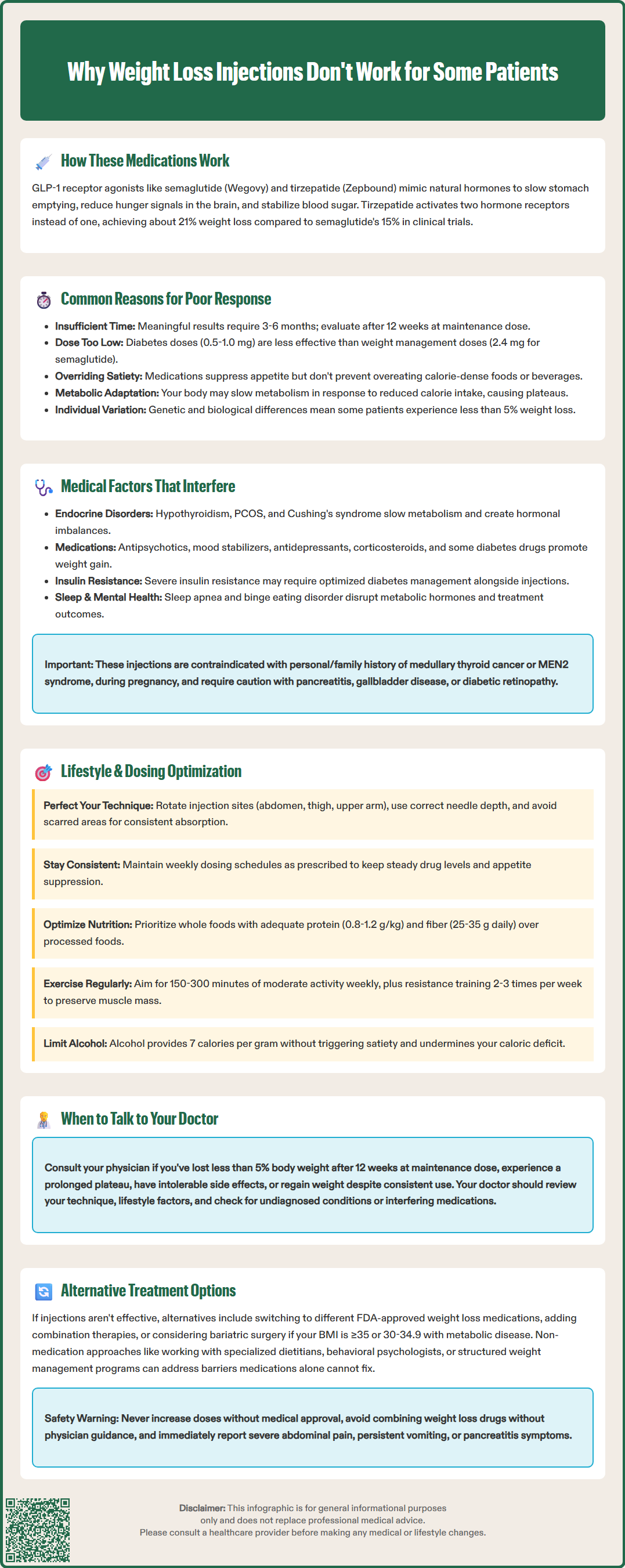
Several factors can diminish or prevent the expected weight loss response to GLP-1 receptor agonists, even when medications are administered correctly. Individual variability in treatment response is well-documented, with some patients achieving less than 5% body weight reduction despite proper use.
Insufficient treatment duration represents a frequent issue. Many patients expect rapid results, but meaningful weight loss typically requires 3-6 months of therapy. According to FDA labeling for Wegovy (semaglutide 2.4 mg), patients should be evaluated after 12 weeks at the maintenance dose, and discontinuation considered if less than 5% weight loss has been achieved. Premature discontinuation before reaching therapeutic doses or adequate treatment duration prevents full pharmacological effect.
Inadequate dosing may occur when patients remain on subtherapeutic doses due to side effect concerns or insurance coverage limitations. For semaglutide, the maintenance dose for weight management is 2.4 mg weekly, significantly higher than the 0.5-1.0 mg doses used for diabetes management. Remaining on lower doses substantially reduces weight loss efficacy.
Compensatory eating behaviors can counteract medication effects. Some patients unconsciously or deliberately increase caloric intake during non-suppressed periods or consume calorie-dense beverages that don't trigger the same satiety response as solid foods. The medication reduces appetite but doesn't eliminate the ability to override satiety signals.
Metabolic adaptation occurs in some individuals, where the body adjusts to reduced caloric intake by decreasing metabolic rate. This adaptive thermogenesis can slow or plateau weight loss despite continued medication use and dietary adherence. While genetic variations in GLP-1 receptor expression or downstream signaling pathways may influence individual treatment response, routine genetic testing isn't currently recommended for predicting outcomes.
Underlying medical conditions and concurrent medications can significantly impact the effectiveness of weight loss injections, sometimes creating physiological barriers to expected outcomes.
Endocrine disorders frequently interfere with weight loss efforts. Hypothyroidism slows metabolic rate and can blunt response to weight loss medications. Thyroid function testing (TSH, free T4) should be current before attributing treatment failure solely to the injection. Treatment decisions for subclinical hypothyroidism should follow American Thyroid Association guidelines. Polycystic ovary syndrome (PCOS) creates insulin resistance and hormonal imbalances that may require additional interventions beyond GLP-1 agonists. Cushing's syndrome, though rare, causes weight gain through cortisol excess that weight loss injections cannot adequately address.
Medications that promote weight gain can counteract GLP-1 effects. These include certain antipsychotics (olanzapine, clozapine), mood stabilizers (valproate, lithium), antidepressants (mirtazapine, paroxetine), corticosteroids, and some diabetes medications like insulin or sulfonylureas. The weight-promoting effects of these medications may partially or completely offset the benefits of weight loss injections.
Insulin resistance severity influences treatment response. Patients with type 2 diabetes and significant insulin resistance may benefit from optimizing diabetes medications according to American Diabetes Association guidelines. A comprehensive metabolic assessment rather than isolated lab values provides better guidance for treatment adjustments.
Sleep disorders, particularly obstructive sleep apnea, disrupt metabolic hormones including leptin and ghrelin, potentially reducing medication effectiveness. Similarly, undiagnosed or poorly controlled psychiatric conditions—especially binge eating disorder or depression—can impair treatment outcomes.
Important safety considerations: These medications are contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. They should not be used during pregnancy, and caution is needed in patients with history of pancreatitis, gallbladder disease, or diabetic retinopathy. Acute kidney injury risk increases with dehydration.
Even with appropriate medical management, lifestyle factors and medication administration practices critically influence treatment outcomes with weight loss injections.
Injection technique problems can reduce drug absorption and effectiveness. Injecting into areas with significant scarring, lipohypertrophy, or inadequate subcutaneous tissue may impair absorption. Rotating injection sites among the abdomen, thigh, and upper arm helps maintain consistent absorption. Injecting too deeply (intramuscular rather than subcutaneous) or too superficially can also affect pharmacokinetics. Proper needle length selection and technique education from healthcare providers ensures optimal drug delivery.
Inconsistent dosing schedules diminish therapeutic effect. GLP-1 receptor agonists require regular administration—weekly for semaglutide and tirzepatide—to maintain steady-state drug levels. Missing doses or irregular timing creates fluctuating drug concentrations that reduce appetite suppression and metabolic benefits. Follow the specific missed-dose instructions in your medication's FDA-approved patient information, as timing recommendations vary by product.
Dietary composition matters beyond total calories. Diets extremely high in processed foods, added sugars, and refined carbohydrates can overwhelm the appetite-suppressing effects of these medications. While GLP-1 agonists don't require specific dietary patterns, emphasizing whole foods, adequate protein (generally 0.8-1.2 g/kg body weight, with higher amounts individualized based on health status), and fiber (25-35 g daily) enhances satiety. Protein recommendations should be adjusted for patients with kidney disease.
Physical activity levels significantly impact outcomes. The US Department of Health and Human Services Physical Activity Guidelines recommend 150-300 minutes of moderate-intensity activity weekly for general health, with higher volumes (>250 minutes/week) often needed for significant weight loss. Resistance training 2-3 times weekly helps preserve metabolic rate by maintaining muscle mass.
Alcohol consumption provides empty calories (7 kcal/g) that don't trigger satiety mechanisms and can impair judgment regarding food choices. Even moderate alcohol intake can substantially reduce the caloric deficit necessary for weight loss, potentially explaining poor treatment response in otherwise adherent patients.
Recognizing when weight loss injections aren't providing adequate benefit requires honest assessment and timely medical consultation to explore alternative or adjunctive strategies.
Specific triggers for medical consultation include achieving less than 5% body weight reduction after reaching the maintenance dose (for Wegovy, after 12 weeks at 2.4 mg as per FDA labeling), prolonged weight loss plateau despite adherence, or intolerable side effects preventing dose escalation to therapeutic levels. Additionally, weight regain while maintaining consistent dosing warrants evaluation for underlying causes or treatment modifications.
During the consultation, expect comprehensive review of medication administration technique, dietary patterns, physical activity levels, sleep quality, and stress management. Your physician should assess for previously undiagnosed conditions affecting weight, review all current medications for potential interactions or weight-promoting effects, and verify appropriate dosing and injection technique.
Alternative pharmacological options include switching to a different FDA-approved weight management medication, as individual response varies between agents. Combination therapy with medications like phentermine/topiramate (Qsymia) or naltrexone/bupropion (Contrave) may benefit some patients, though evidence for combining these with GLP-1 agonists remains limited.
Non-pharmacological interventions deserve consideration when medications prove insufficient. Referral to registered dietitians specializing in weight management, behavioral psychology for eating disorder assessment, or structured weight management programs may address non-pharmacological barriers. For patients with BMI ≥35 kg/m² (regardless of comorbidities) or BMI 30-34.9 kg/m² with metabolic disease, bariatric surgery consultation may be appropriate, according to 2022 American Society for Metabolic and Bariatric Surgery guidelines.
Important safety considerations: Never increase doses beyond prescribed amounts without medical supervision, don't combine weight loss medications without physician approval, and report concerning symptoms immediately. These include severe abdominal pain, persistent nausea/vomiting, or signs of pancreatitis. These medications are contraindicated during pregnancy and in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Use caution with history of pancreatitis, gallbladder disease, or diabetic retinopathy, and stay hydrated to reduce acute kidney injury risk.
According to FDA labeling for Wegovy (semaglutide), patients should be evaluated after 12 weeks at the maintenance dose (2.4 mg weekly), with discontinuation considered if less than 5% body weight reduction has been achieved. Meaningful weight loss typically requires 3-6 months of therapy at therapeutic doses.
Yes, certain medications promote weight gain and can counteract GLP-1 effects, including antipsychotics (olanzapine, clozapine), mood stabilizers (valproate, lithium), some antidepressants (mirtazapine, paroxetine), corticosteroids, and diabetes medications like insulin or sulfonylureas.
Underlying conditions that can impair treatment response include hypothyroidism, polycystic ovary syndrome (PCOS), Cushing's syndrome, obstructive sleep apnea, and psychiatric conditions like binge eating disorder. Thyroid function testing and comprehensive metabolic assessment should be current before attributing treatment failure solely to the medication.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.