LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do you have to stay on GLP-1 for life? For most patients, GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) require long-term use to maintain their benefits. These medications treat chronic conditions—type 2 diabetes and obesity—that typically need ongoing management. Clinical evidence shows that stopping GLP-1 therapy usually leads to weight regain and worsening blood sugar control. Treatment duration depends on your medical indication, individual response, and health goals. Understanding what happens when you stop these medications helps you and your healthcare provider make informed decisions about your long-term treatment plan.
Quick Answer: Most patients require long-term GLP-1 therapy because stopping these medications typically results in weight regain and worsening blood sugar control, as they treat chronic conditions like type 2 diabetes and obesity.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and now widely prescribed for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity). Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist that works through similar but expanded mechanisms. These medications mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestines in response to food intake.
The mechanism of action involves several physiological pathways that contribute to both glycemic control and weight loss. GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion while suppressing inappropriate glucagon release. This dual action helps normalize blood glucose levels without causing significant hypoglycemia in most patients, though the risk increases when combined with insulin or sulfonylureas. Additionally, these medications slow gastric emptying, which prolongs the sensation of fullness after meals and reduces appetite through central nervous system effects on satiety centers in the hypothalamus.
For weight management specifically, the FDA has approved several GLP-1 medications at higher doses than those used for diabetes treatment. The weight loss achieved varies by medication: liraglutide typically produces 5-8% weight loss, semaglutide approximately 15%, and tirzepatide up to 21% of initial body weight. Clinical trials have demonstrated that weight reduction occurs gradually over 12 to 18 months, with most patients reaching maximum effect within this timeframe. Some GLP-1 medications have demonstrated cardiovascular protective effects in specific populations—liraglutide, semaglutide injection, and dulaglutide have shown cardiovascular outcome benefits, with Wegovy (semaglutide) recently receiving an FDA indication for cardiovascular risk reduction in adults with established cardiovascular disease and either overweight or obesity.
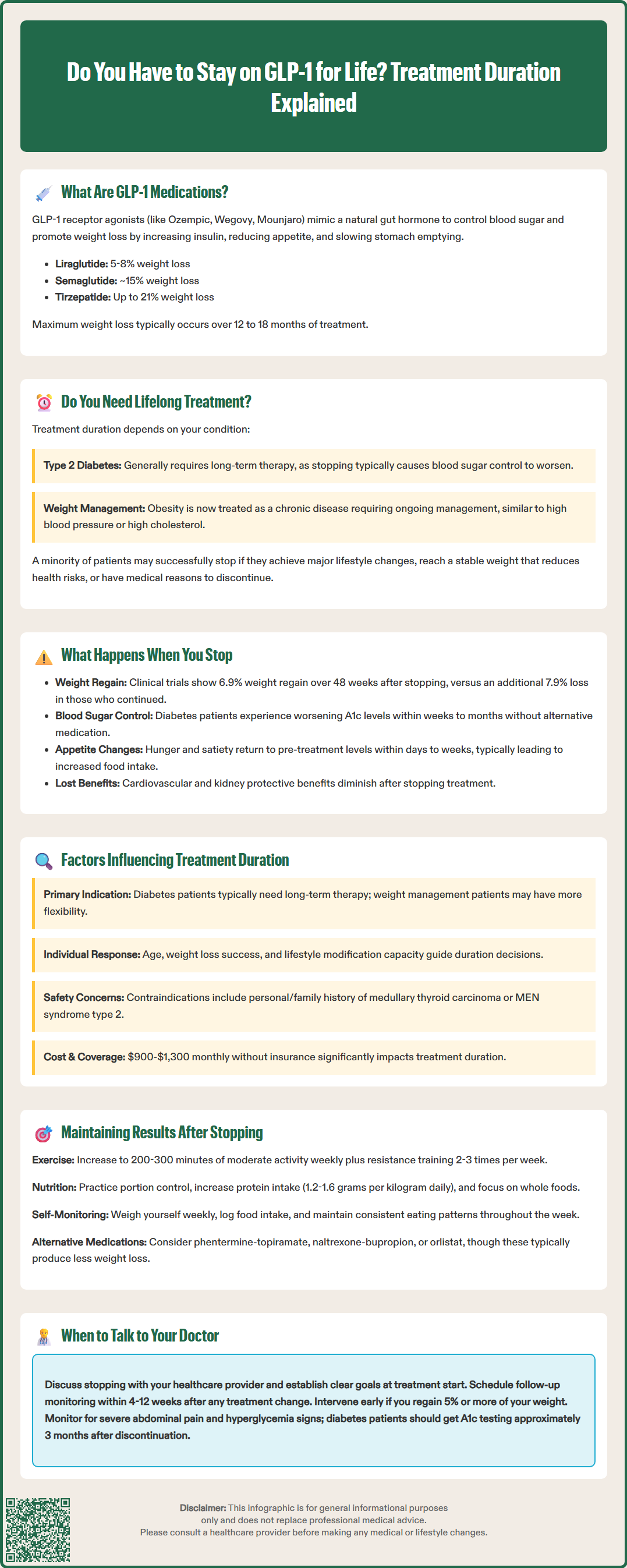
The question of lifelong GLP-1 therapy does not have a universal answer, as treatment duration depends on the indication, individual patient circumstances, and treatment goals. For patients with type 2 diabetes, GLP-1 medications are generally considered long-term therapy as part of individualized disease management. Diabetes is a progressive condition, and discontinuing effective glucose-lowering therapy typically results in deterioration of glycemic control. The American Diabetes Association guidelines support continued use of medications that effectively manage blood glucose and provide additional benefits such as weight loss and cardiovascular protection, with regular reassessment of treatment goals and tolerability.
For weight management in patients without diabetes, the situation is more nuanced but current evidence suggests that obesity should also be treated as a chronic condition requiring ongoing management. Clinical trials examining medication discontinuation have consistently demonstrated significant weight regain after stopping GLP-1 therapy. The STEP 4 trial, which specifically examined semaglutide withdrawal, showed that participants who stopped the medication regained 6.9% of body weight over 48 weeks, while those who continued treatment lost an additional 7.9%. Similarly, the SURMOUNT-4 trial showed substantial weight regain following tirzepatide discontinuation.
Some patients may successfully transition off GLP-1 medications if they achieve substantial lifestyle modifications, reach a stable weight that significantly reduces health risks, or experience circumstances that make continued treatment inappropriate. However, this represents a minority of cases. The current medical consensus, reflected in obesity medicine guidelines from organizations such as the American Gastroenterological Association and Obesity Medicine Association, treats obesity as a chronic disease requiring long-term pharmacological management in most cases, similar to hypertension or hyperlipidemia. Patients considering discontinuation should engage in thorough discussions with their healthcare providers about realistic expectations and alternative management strategies, with follow-up monitoring within 4-12 weeks after any treatment change.
Discontinuation of GLP-1 medications typically results in predictable physiological changes as the pharmacological effects wear off. The timeline varies depending on the specific medication's half-life—shorter-acting agents like liraglutide (half-life approximately 13 hours) clear more quickly than longer-acting options like semaglutide (half-life approximately one week). Within days to weeks of stopping treatment, patients generally experience return of appetite to pre-treatment levels, faster gastric emptying, and loss of the medication's effects on satiety signaling. These changes often lead to increased food intake and gradual weight regain.
For patients with type 2 diabetes, stopping GLP-1 therapy without alternative glucose-lowering medication typically results in worsening glycemic control. Hemoglobin A1c levels generally rise within weeks to months, returning toward pre-treatment values unless significant lifestyle changes have been maintained. Patients may notice return of hyperglycemia symptoms such as increased thirst, frequent urination, and fatigue. Severe hyperglycemia requiring urgent medical attention can occur in some patients, particularly those with poorly controlled diabetes before treatment. The cardiovascular and renal protective benefits observed with certain GLP-1 medications also diminish after discontinuation.
Weight regain following GLP-1 discontinuation occurs gradually but consistently in most patients. Research from the STEP trials (semaglutide) and SURMOUNT-4 (tirzepatide) shows that without ongoing pharmacotherapy or substantial behavioral interventions, significant weight regain occurs within the first year after stopping treatment. This weight regain is not due to medication "dependence" in the traditional sense, but rather reflects the underlying biology of obesity as a chronic condition. The body's metabolic adaptations to weight loss—including decreased energy expenditure, increased hunger hormones, and reduced satiety signals—persist long after weight reduction, making weight maintenance challenging without continued intervention. Some patients report changes in appetite or food cravings during the transition period, though these effects are generally temporary and related to the physiological adjustments rather than withdrawal symptoms.
Patients discontinuing GLP-1 medications should monitor for signs of gallbladder problems (severe abdominal pain, especially after meals), pancreatitis (persistent severe abdominal pain, sometimes with vomiting), or significant hyperglycemia. Regular follow-up with healthcare providers, including A1c testing approximately 3 months after discontinuation for patients with diabetes, is recommended.
Several clinical and individual factors should inform decisions about GLP-1 treatment duration. The primary indication for therapy is paramount—patients using these medications for type 2 diabetes management typically require long-term treatment as part of comprehensive disease management, whereas those using GLP-1 agents solely for weight management may have more flexibility depending on their response and circumstances. The presence of obesity-related complications such as obstructive sleep apnea, metabolic dysfunction-associated steatotic liver disease (MASLD, formerly NAFLD), or cardiovascular disease may justify longer treatment duration given the health benefits of sustained weight loss.
Patient-specific factors including age, comorbidities, and ability to implement lifestyle modifications significantly influence appropriate treatment duration. Younger patients who achieve substantial weight loss and demonstrate capacity for sustained dietary and exercise changes may be candidates for medication discontinuation with close monitoring. Conversely, patients with long-standing obesity, multiple previous weight loss attempts, or significant metabolic dysfunction may benefit from indefinite therapy. The degree of weight loss achieved also matters—patients who reach a healthy weight range and maintain it for an extended period while on medication may attempt discontinuation differently than those who achieve modest weight reduction.
Safety considerations are critical in determining treatment duration. GLP-1 medications carry important warnings and contraindications, including a boxed warning for thyroid C-cell tumors in rodents (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2). Other safety concerns include risks of pancreatitis, gallbladder disease, and diabetic retinopathy complications (particularly with semaglutide). These medications are contraindicated during pregnancy and breastfeeding. Ongoing risk-benefit assessment is essential.
Practical considerations including medication cost, insurance coverage, side effect tolerance, and patient preferences play important roles in treatment duration decisions. GLP-1 medications are expensive, with monthly costs ranging from $900 to $1,300 without insurance coverage. Medicare traditionally excludes coverage for weight management medications, though Wegovy's cardiovascular risk reduction indication may enable Part D coverage for eligible patients with established cardiovascular disease. Some patients experience persistent gastrointestinal side effects that may limit long-term tolerability.
Healthcare providers should engage patients in shared decision-making regarding treatment duration, establishing clear goals at treatment initiation and regularly reassessing the need for continued therapy. For patients with severe obesity (BMI ≥40 or ≥35 with obesity-related complications), referral for evaluation of bariatric surgery may be appropriate according to American Society for Metabolic and Bariatric Surgery guidelines.
For patients who discontinue GLP-1 medications, several evidence-based strategies can help maintain weight loss and metabolic improvements, though success rates vary considerably. Comprehensive lifestyle interventions remain the cornerstone of weight maintenance and should be intensified before and after medication discontinuation. This includes structured dietary approaches such as portion control, increased protein intake (1.2 to 1.6 grams per kilogram of body weight daily, with caution in chronic kidney disease), and emphasis on whole foods with high satiety value. Regular physical activity is particularly crucial for weight maintenance, with guidelines recommending at least 200 to 300 minutes of moderate-intensity exercise weekly plus resistance training 2-3 days per week for individuals maintaining significant weight loss—substantially more than the 150 minutes recommended for general health per the Physical Activity Guidelines for Americans.
Behavioral strategies proven effective for weight maintenance include consistent self-monitoring of weight (at least weekly), food logging, regular meal patterns, and cognitive behavioral techniques to address emotional eating and environmental triggers. Many patients benefit from ongoing support through registered dietitians, health coaches, or structured weight management programs. The National Weight Control Registry, which tracks individuals who have successfully maintained significant weight loss, identifies common characteristics including high levels of physical activity, regular breakfast consumption, consistent eating patterns across weekdays and weekends, and frequent self-weighing.
Alternative pharmacological options may be considered for patients who cannot continue GLP-1 therapy but require ongoing medication support. These include other FDA-approved weight management medications such as phentermine-topiramate (Qsymia), naltrexone-bupropion (Contrave), or orlistat (Xenical, Alli), though these agents generally produce less weight loss than GLP-1 medications. Phentermine is FDA-approved only for short-term use (up to 12 weeks). For patients with type 2 diabetes, alternative glucose-lowering medications such as SGLT2 inhibitors or metformin provide metabolic benefits, though with less pronounced weight effects. Some patients may benefit from transitioning to lower doses of GLP-1 medications rather than complete discontinuation, though this approach requires further research to establish optimal dosing strategies.
Metabolic and bariatric surgery represents a more definitive intervention for eligible patients with severe obesity who cannot maintain results with pharmacotherapy alone. According to ASMBS/IFSO guidelines, surgery may be considered for patients with BMI ≥40 kg/m² or BMI ≥35 kg/m² with obesity-related complications. Procedures such as sleeve gastrectomy or Roux-en-Y gastric bypass produce substantial, durable weight loss through both mechanical and hormonal mechanisms, including increased endogenous GLP-1 production. Patients considering GLP-1 discontinuation should work closely with their healthcare team to develop individualized maintenance plans, establish realistic expectations about weight trajectory, and implement close monitoring for weight regain. Early intervention at the first signs of significant regain—typically defined as 5% or more weight increase—allows for timely adjustment of strategies and consideration of medication resumption if needed.
Most patients experience significant weight regain after stopping GLP-1 medications, with clinical trials showing regain of substantial weight within the first year. This occurs because appetite returns to pre-treatment levels and the body's metabolic adaptations to weight loss persist, making weight maintenance challenging without continued intervention.
While possible, maintaining results after stopping GLP-1 therapy is challenging and requires intensive lifestyle modifications including 200-300 minutes of weekly exercise, consistent dietary changes, regular self-monitoring, and often ongoing behavioral support. Some patients may benefit from transitioning to alternative weight management medications or lower GLP-1 doses rather than complete discontinuation.
The timeline depends on the medication's half-life—shorter-acting agents like liraglutide clear within days, while longer-acting options like semaglutide take approximately one week. Within days to weeks, patients typically experience return of appetite, faster stomach emptying, and gradual weight regain as the medication's effects diminish.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.