LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients starting GLP-1 medications like Ozempic, Wegovy, or Mounjaro wonder whether they'll need lifelong treatment. The answer depends on why you're taking them. For type 2 diabetes, GLP-1 receptor agonists are typically long-term therapies, similar to blood pressure or cholesterol medications. For weight management, the FDA labels these drugs as treatments for chronic obesity, intended for continued use. Most patients experience weight regain and worsening blood sugar control after stopping. However, individual factors—including treatment response, side effects, cost, and personal goals—influence how long you'll take these medications. Understanding what happens when you stop can help you make informed decisions with your healthcare provider.
Quick Answer: Most patients require long-term GLP-1 therapy because diabetes and obesity are chronic conditions, and discontinuation typically causes weight regain and worsening blood sugar control.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and now widely prescribed for chronic weight management. These medications include semaglutide (Ozempic, Wegovy, Rybelsus), tirzepatide (Mounjaro, Zepbound)—which is actually a dual GIP/GLP-1 receptor agonist—dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). While most are injectable, oral semaglutide (Rybelsus) is available for type 2 diabetes treatment.
The mechanism of action involves several physiological pathways. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they promote insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications, though this risk increases when combined with insulin or sulfonylureas. Simultaneously, these drugs suppress glucagon secretion, which prevents the liver from releasing excess glucose into the bloodstream.
Beyond glycemic control, these medications slow gastric emptying (though this effect may diminish over time), which prolongs the feeling of fullness after meals. They also act on appetite centers in the hypothalamus, reducing hunger signals and food cravings. This dual effect on satiety and appetite makes them particularly effective for weight management. Most formulations are administered once weekly, though some require daily dosing.
The FDA has approved various GLP-1 receptor agonists for different indications, including glycemic control in type 2 diabetes and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. Some medications (Wegovy, Saxenda) are also approved for weight management in adolescents aged 12 and older. Important safety considerations include contraindications for patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), and warnings regarding pancreatitis, gallbladder disease, and diabetic retinopathy complications.
The duration of GLP-1 therapy depends primarily on the indication for which it was prescribed. For type 2 diabetes management, these medications are generally considered long-term treatments, similar to other chronic disease medications like antihypertensives or statins. The American Diabetes Association (ADA) Standards of Care emphasize that diabetes is a progressive condition requiring ongoing pharmacological management in most patients, and discontinuing effective therapy typically results in deterioration of glycemic control. However, significant weight loss may lead to diabetes remission in some patients, requiring ongoing monitoring but potentially less medication.
When prescribed for weight management, the FDA-approved labels for medications like Wegovy and Zepbound indicate they are intended for chronic weight management, with continued use as long as benefits outweigh risks. The labels specify evaluation after approximately 12 weeks at the maintenance dose, with discontinuation recommended if less than 5% weight loss is achieved. Clinical trials supporting their approval typically lasted 68 to 72 weeks, but extension studies have followed patients for longer periods. The underlying principle, supported by guidelines from the Endocrine Society, American Association of Clinical Endocrinology, and American Gastroenterological Association, is that obesity is a chronic metabolic disease requiring ongoing medical management.
Some patients and clinicians explore whether GLP-1 medications can be used as a "bridge" to establish healthier habits, with the hope of discontinuing therapy once weight loss goals are achieved and lifestyle modifications are firmly established. However, there is limited evidence supporting this approach as a standard practice. Current medical consensus suggests that most patients will require continued pharmacotherapy to maintain weight loss and metabolic improvements.
Individual circumstances vary considerably. Some patients may achieve sufficient lifestyle changes or undergo bariatric surgery that reduces their need for medication. Others may experience side effects that necessitate discontinuation. The decision about treatment duration should be made collaboratively between patient and physician, considering individual response, tolerability, cost, insurance coverage, and personal goals.
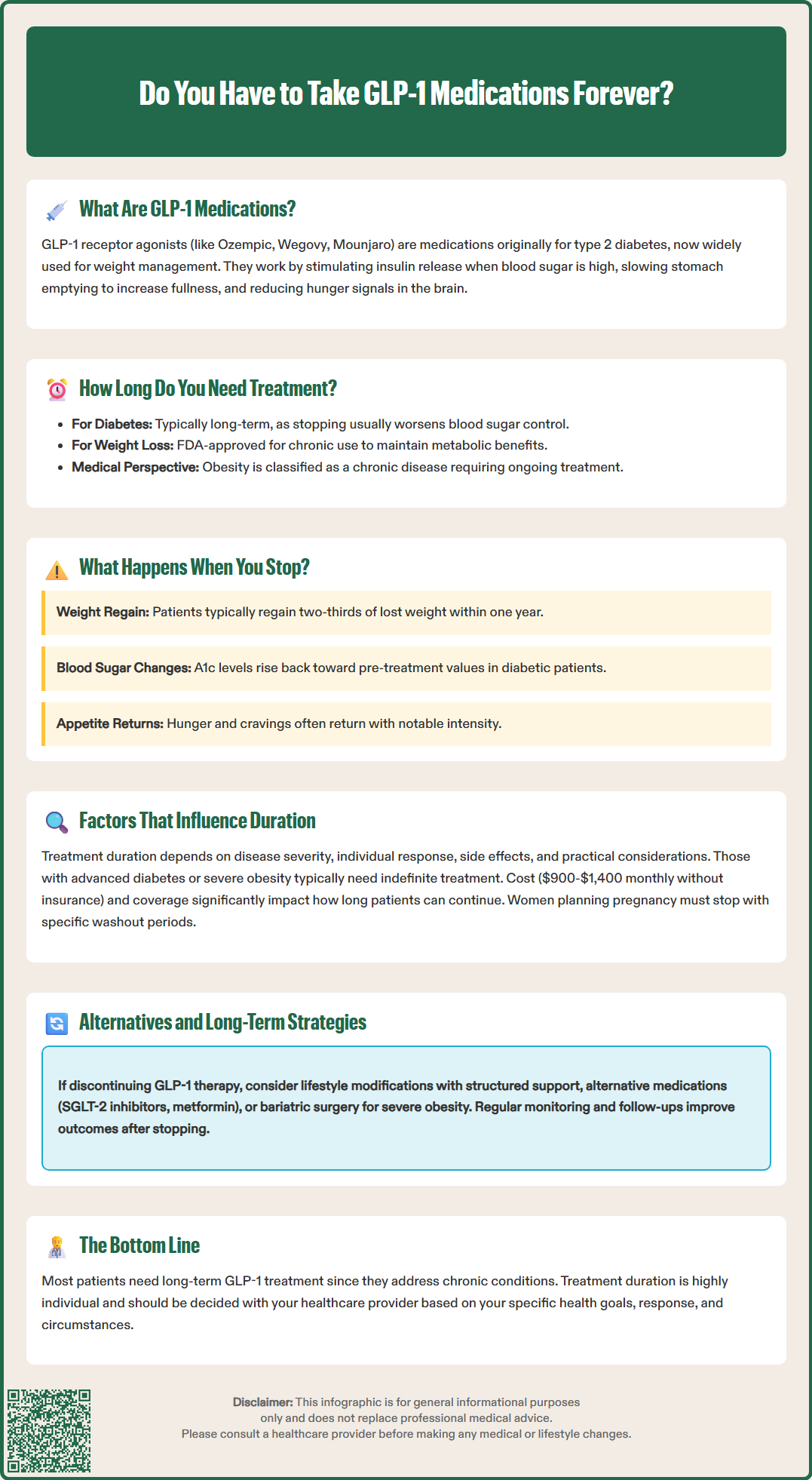
Discontinuing GLP-1 receptor agonists typically results in a reversal of many therapeutic benefits, though the timeline and extent vary among individuals. Clinical studies consistently demonstrate that most patients experience weight regain after stopping these medications. In the STEP 1 trial extension phase, participants who discontinued semaglutide regained approximately two-thirds of their lost weight within one year. Similarly, the SURMOUNT-4 trial showed significant weight regain after tirzepatide discontinuation. This occurs because the medication's effects on appetite suppression, satiety, and metabolic rate cease once the drug is cleared from the system.
For patients with type 2 diabetes, stopping GLP-1 therapy usually leads to worsening glycemic control. Hemoglobin A1c levels tend to rise within weeks to months after discontinuation, returning toward pre-treatment values. The rate of deterioration depends on the underlying severity of diabetes, beta-cell function, and whether other diabetes medications are continued. Some patients may maintain improved glucose control if they have made substantial lifestyle modifications or if their diabetes was mild at baseline, but this represents a minority of cases.
Physiologically, the body returns to its baseline state once GLP-1 receptor stimulation ceases. Gastric emptying normalizes, appetite-regulating hormones return to pre-treatment patterns, and the metabolic advantages conferred by weight loss begin to diminish as weight is regained. While most patients return to their baseline state, individual responses vary, and some may experience more pronounced hunger or cravings during the adjustment period. Patients often report that hunger and cravings return with notable intensity, which can be psychologically challenging.
Patients who stop these medications should work closely with their healthcare provider to monitor weight, blood glucose, and other metabolic parameters. Adjustments to other diabetes medications may be necessary to maintain glycemic control. Regular follow-up appointments are important to assess for any changes in health status and consider alternative or additional interventions to maintain health improvements achieved during treatment.
Multiple clinical and personal factors determine how long an individual might take GLP-1 medications. Disease severity plays a crucial role—patients with more advanced type 2 diabetes or higher degrees of obesity typically require longer treatment durations and may need indefinite therapy. Those with mild metabolic dysfunction who respond well to lifestyle interventions may have more flexibility in treatment duration.
Treatment response and tolerability significantly influence continuation decisions. Patients who experience substantial weight loss or excellent glycemic control with minimal side effects are more likely to continue long-term therapy. Conversely, those with inadequate response (less than 5% weight loss after 12-16 weeks at therapeutic doses) should discontinue per FDA labeling. Gastrointestinal side effects like nausea, vomiting, or diarrhea are common but often improve with proper titration; persistent severe symptoms may necessitate discontinuation. Rare but serious adverse effects, including pancreatitis, gallbladder disease, or severe gastrointestinal adverse events, may require stopping treatment.
Cost and access represent major practical considerations in the United States. GLP-1 medications can cost $900-$1,400 monthly without insurance coverage. Insurance authorization requirements, formulary restrictions, and prior authorization denials affect many patients. While some individuals use these medications intermittently based on financial constraints, this approach lacks robust evidence and may compromise outcomes.
Patient goals and preferences matter considerably. Some patients view these medications as temporary tools to jumpstart weight loss, while others accept them as long-term management for a chronic condition. Personal values regarding medication use, injection tolerance, and lifestyle modification confidence all influence treatment duration decisions. Pregnancy planning also affects duration—medication-specific washout periods apply (approximately 2 months for semaglutide, 1 month for tirzepatide/dulaglutide, and immediate discontinuation for liraglutide when pregnancy is recognized).
Comorbidity management may extend or shorten treatment duration. Patients who achieve remission of obesity-related conditions like sleep apnea or fatty liver disease may feel motivated to continue therapy. Conversely, development of other health conditions or medication interactions might necessitate discontinuation. Patients with a personal or family history of medullary thyroid carcinoma or MEN2 syndrome should not use these medications at all. Regular monitoring and shared decision-making between patient and clinician remain essential throughout the treatment course.
For patients who discontinue GLP-1 medications or seek complementary approaches, several evidence-based alternatives exist. Lifestyle modification remains foundational, though it requires intensive support to be effective long-term. Structured programs incorporating dietary counseling, physical activity guidance, and behavioral therapy can help maintain weight loss. The CDC-recognized Diabetes Prevention Program demonstrated that intensive lifestyle intervention reduces diabetes incidence, though weight regain over time is common without ongoing support. Medical nutrition therapy provided by registered dietitian nutritionists offers personalized guidance.
Other pharmacological options include different weight management medications such as phentermine-topiramate (Qsymia), naltrexone-bupropion (Contrave), and orlistat (Xenical, Alli). For diabetes management, alternatives include SGLT-2 inhibitors, DPP-4 inhibitors (which should not be combined with GLP-1 medications), metformin, and insulin when necessary. These medications have different mechanisms, side effect profiles, and efficacy levels. Some patients benefit from combination therapy or sequential medication trials to find optimal regimens.
Bariatric surgery represents the most effective long-term intervention for severe obesity, with sustained weight loss and metabolic improvements exceeding those achieved with medications alone. The 2022 ASMBS/IFSO guidelines support consideration of metabolic surgery for patients with BMI ≥35 kg/m² or ≥30 kg/m² with obesity-related comorbidities. Procedures like sleeve gastrectomy and Roux-en-Y gastric bypass alter gut hormone profiles in ways that partially overlap with GLP-1 medications.
Maintenance strategies for those who stop GLP-1 therapy should include regular monitoring of weight, blood glucose, and metabolic parameters. Establishing accountability through frequent follow-up visits, support groups, or digital health tools can improve outcomes. Some clinicians suggest intermittent or reduced-dose GLP-1 therapy as a maintenance strategy, though this approach remains investigational and lacks robust evidence. Realistic goal-setting is crucial—maintaining even 5-10% weight loss provides significant health benefits, even if it represents partial regain from peak weight loss.
Patients should be aware of red flags requiring medical attention, including severe persistent abdominal pain (possible pancreatitis), severe or persistent vomiting leading to dehydration, symptoms of gallbladder disease, vision changes, or allergic reactions.
Ultimately, the question of whether you must take GLP-1 medications forever has no universal answer. These drugs treat chronic conditions that typically require ongoing management, and most patients will experience disease recurrence after discontinuation. However, individual circumstances, treatment goals, and personal preferences should guide decisions about treatment duration in consultation with qualified healthcare providers.
Most patients regain weight after stopping GLP-1 medications, with clinical trials showing approximately two-thirds of lost weight returns within one year. These drugs treat chronic conditions requiring ongoing management, though individual circumstances and consultation with your healthcare provider should guide discontinuation decisions.
Hemoglobin A1c levels typically rise within weeks to months after discontinuing GLP-1 therapy, returning toward pre-treatment values. Your healthcare provider may need to adjust other diabetes medications to maintain glycemic control after stopping.
Alternatives include intensive lifestyle modification programs, other weight management medications like phentermine-topiramate or naltrexone-bupropion, different diabetes medications such as SGLT-2 inhibitors, and bariatric surgery for severe obesity. Your healthcare provider can help determine the most appropriate approach based on your individual circumstances.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.