LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does your body get used to tirzepatide over time? This common concern among patients using Mounjaro or Zepbound reflects worries about diminishing effectiveness with long-term use. Tirzepatide is a dual GIP and GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. Current clinical evidence shows that tirzepatide maintains its primary therapeutic effects on glucose control and weight management without true pharmacological tolerance developing. While some patients experience weight plateaus or adaptive changes, these typically reflect normal metabolic adjustments rather than the body becoming resistant to the medication's core mechanisms.
Quick Answer: Clinical evidence shows that the body does not develop true tolerance to tirzepatide's primary glucose-lowering and weight management effects with long-term use.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works through multiple complementary mechanisms that influence metabolic function throughout treatment.
The drug enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it stimulates insulin release primarily when blood glucose levels are elevated. While this mechanism reduces the risk of hypoglycemia compared to some other diabetes medications, the risk increases when tirzepatide is used with insulin or sulfonylureas. Simultaneously, tirzepatide suppresses glucagon secretion from pancreatic alpha cells, which decreases hepatic glucose production. These effects work together to improve glycemic control in patients with type 2 diabetes.
Beyond glucose regulation, tirzepatide significantly affects appetite and satiety through central nervous system pathways. The medication initially slows gastric emptying, which prolongs the feeling of fullness after meals and reduces overall caloric intake. Notably, this gastric emptying effect tends to attenuate over time with continued treatment, while the medication's effects on weight and blood glucose control persist. Tirzepatide also acts on appetite centers in the hypothalamus, decreasing hunger signals and food cravings. These mechanisms contribute to the substantial weight loss observed in clinical trials.
Throughout continued treatment, tirzepatide maintains its primary pharmacological activity. The medication's half-life of approximately 5 days allows for once-weekly dosing, with steady-state concentrations achieved after about 4 weeks of regular administration, according to FDA prescribing information. Understanding these foundational mechanisms helps contextualize questions about whether the body develops tolerance to tirzepatide's effects over extended periods of use.
Current clinical evidence does not support the development of true pharmacological tolerance to tirzepatide's primary effects with long-term use. Tolerance, in medical terms, refers to a diminished response to a drug after repeated administration, requiring higher doses to achieve the same effect. The available data from extended clinical trials suggests that tirzepatide continues to exert its therapeutic effects on glucose control and weight management without requiring dose escalation beyond the standard titration schedule.
The SURPASS clinical trial program, which evaluated tirzepatide for type 2 diabetes over periods extending to 52 weeks and beyond, demonstrated sustained glycemic improvements without evidence of significant tachyphylaxis (rapid tolerance development) for the primary glucose-lowering effects. Participants maintained A1C reductions throughout the study duration, and there was no indication that the medication's glucose-lowering effects diminished over time at stable maintenance doses. Similarly, the SURMOUNT trials examining weight management showed continued weight loss or weight maintenance throughout treatment periods exceeding 72 weeks.
It's important to note that while the primary metabolic effects appear durable, some specific effects do show adaptation. For example, the gastric emptying delay seen with tirzepatide typically attenuates over time with continued treatment, even as weight and glycemic benefits persist. This represents a selective adaptation rather than global tolerance to the medication.
Individual responses to tirzepatide can vary considerably based on factors including baseline metabolic health, adherence to lifestyle modifications, concurrent medications, and underlying physiological changes. What may appear as tolerance is often attributable to other factors such as dietary adaptation, metabolic compensation, or progression of underlying disease rather than true receptor-level tolerance to the medication itself.
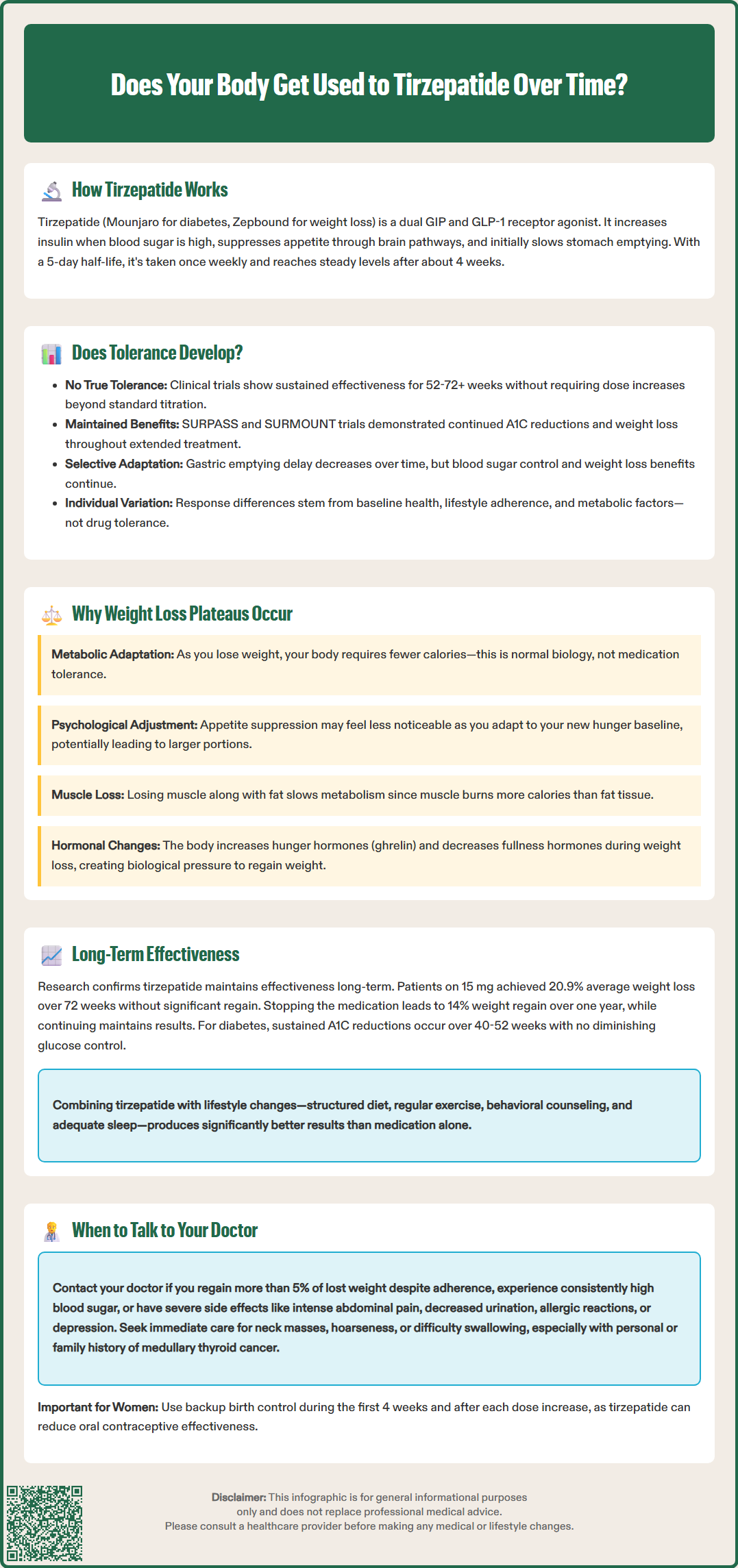
Many patients experience a weight loss plateau during tirzepatide treatment, which can be mistakenly interpreted as the body "getting used to" the medication. However, this plateau phenomenon reflects normal physiological adaptations rather than true drug tolerance. Understanding these mechanisms helps set realistic expectations and guides appropriate management strategies.
Metabolic adaptation is a well-documented response to weight loss, regardless of the method used to achieve it. As body weight decreases, total energy expenditure declines proportionally because there is less body mass to maintain. Additionally, the body may reduce its resting metabolic rate beyond what would be expected from weight loss alone—a phenomenon sometimes called "adaptive thermogenesis." This metabolic compensation means that the same caloric intake that initially produced weight loss may eventually result in weight stability.
Behavioral factors also contribute significantly to weight plateaus. The initial appetite suppression from tirzepatide may feel less pronounced over time, not because the medication stops working, but because patients psychologically adapt to the new baseline of reduced hunger. Some individuals may gradually increase portion sizes or caloric intake as they become accustomed to the medication's effects, partially offsetting its benefits. Additionally, as physical activity becomes easier with weight loss, some patients may inadvertently reduce their activity levels.
Physiological changes in body composition during weight loss also affect the rate of continued weight reduction. As patients lose weight, they lose both fat mass and some lean muscle mass. Since muscle tissue is metabolically more active than fat tissue, this shift can further reduce metabolic rate. Maintaining adequate protein intake and incorporating resistance training can help preserve lean muscle mass during weight loss. The body also increases production of hunger hormones like ghrelin and decreases satiety hormones, creating a biological drive to regain lost weight. These are normal adaptive responses that occur with any significant weight loss, not specific tolerance to tirzepatide.
Long-term clinical trial data provides reassuring evidence about tirzepatide's sustained effectiveness when used as part of a comprehensive treatment approach. The SURMOUNT-1 trial, which followed participants for 72 weeks, demonstrated that patients on the highest dose (15 mg) achieved an average weight loss of 20.9% from baseline, with weight loss continuing throughout most of the study period before stabilizing. Importantly, participants who remained on treatment maintained their weight loss rather than experiencing significant regain.
The SURMOUNT-4 trial specifically examined what happens when tirzepatide is discontinued after initial weight loss. Participants who switched from tirzepatide to placebo regained approximately 14% of their body weight over 52 weeks, while those who continued tirzepatide maintained their weight loss and even achieved modest additional reductions. This finding strongly suggests that tirzepatide continues to work effectively over time and that perceived tolerance may actually reflect the medication's ongoing necessity for weight maintenance.
For glycemic control in type 2 diabetes, the SURPASS trials showed sustained A1C reductions over 40-52 weeks across all dose levels. Many participants achieved A1C levels below 5.7% (normoglycemia), well below the diabetes diagnostic threshold of A1C ≥6.5% per American Diabetes Association standards. These improvements were maintained throughout the study duration, with no evidence of diminishing glucose-lowering effects that would suggest tolerance development.
To optimize long-term effectiveness, research emphasizes the importance of concurrent lifestyle modifications. Patients who combine tirzepatide with structured dietary changes, regular physical activity, behavioral counseling, and adequate sleep tend to achieve better outcomes. The medication works most effectively as part of a comprehensive approach rather than as monotherapy. Additionally, proper dose titration according to FDA-approved schedules helps maximize benefits while minimizing gastrointestinal side effects that might affect adherence.
While tirzepatide generally maintains its effectiveness over time, certain situations warrant a conversation with your healthcare provider about your treatment response. Recognizing when to seek medical guidance ensures optimal outcomes and appropriate management adjustments.
You should contact your doctor if you experience a significant plateau or weight regain (more than 5% of lost weight) despite continued medication adherence and lifestyle efforts. This may indicate the need for dose adjustment, evaluation of concurrent medications that might affect weight (such as certain antidepressants or corticosteroids), or assessment of underlying conditions like hypothyroidism or polycystic ovary syndrome that could impair weight loss. Your provider may also evaluate whether you've reached the maximum approved dose and discuss whether additional interventions might be beneficial.
For patients using tirzepatide for type 2 diabetes management, worsening glycemic control despite consistent medication use requires prompt evaluation. If your home glucose monitoring shows persistently elevated readings or if you develop symptoms of hyperglycemia (increased thirst, frequent urination, blurred vision, fatigue), schedule an appointment. Your doctor may need to check your A1C, assess for disease progression, review other medications, or consider adding complementary diabetes therapies. If you're also taking insulin or sulfonylureas, be aware of increased hypoglycemia risk and discuss potential dose adjustments of these medications.
Adverse effects that warrant immediate medical attention include signs of pancreatitis (severe abdominal pain radiating to the back, nausea, vomiting), gallbladder problems, allergic reactions, or symptoms of acute kidney injury (decreased urination, swelling, fatigue). Additionally, if you notice any new or worsening depression or suicidal thoughts while taking tirzepatide for weight management, seek prompt medical care. Patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not use tirzepatide, and any symptoms such as neck mass, hoarseness, difficulty swallowing, or shortness of breath should be reported immediately.
Women using oral contraceptives should be aware that tirzepatide may reduce their effectiveness, particularly during the first 4 weeks after starting treatment or after each dose increase. Alternative or additional contraceptive methods are recommended during these periods.
Finally, discuss your treatment goals and expectations regularly with your healthcare provider. If you're uncertain whether your response is appropriate, if you're considering discontinuing treatment, or if you have questions about long-term use, open communication ensures you receive personalized guidance based on your individual circumstances and the latest clinical evidence.
No, clinical trials extending beyond 72 weeks show that tirzepatide continues to maintain its glucose-lowering and weight management effects without developing true pharmacological tolerance. Patients who remain on treatment maintain their results, while those who discontinue experience weight regain.
Weight plateaus during tirzepatide treatment typically result from normal metabolic adaptation as your body adjusts to a lower weight, behavioral factors like gradual increases in caloric intake, and changes in body composition. This represents physiological adjustment rather than the medication losing effectiveness.
Contact your healthcare provider if you experience significant weight regain (more than 5% of lost weight), worsening blood glucose control, severe abdominal pain, or other concerning symptoms. Regular discussions about treatment goals and response help ensure optimal outcomes and appropriate management adjustments.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.