LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Feeling weak on semaglutide is a concern reported by some patients using this GLP-1 receptor agonist for type 2 diabetes or weight management. Semaglutide, marketed as Ozempic and Wegovy, effectively controls blood sugar and promotes weight loss but can cause fatigue through several mechanisms. Reduced caloric intake from appetite suppression, gastrointestinal side effects like nausea and vomiting, dehydration, and rapid weight loss all contribute to weakness. Understanding why this occurs and implementing targeted nutritional and hydration strategies can help patients maintain energy levels while benefiting from treatment. Most cases of weakness are manageable, though certain symptoms require prompt medical evaluation.
Quick Answer: Weakness on semaglutide typically results from reduced caloric intake due to appetite suppression, gastrointestinal side effects causing dehydration and electrolyte imbalances, and rapid weight loss rather than direct medication toxicity.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand name Ozempic) and chronic weight management (Wegovy). While highly effective for glycemic control and weight loss, some patients report experiencing weakness and fatigue during treatment. Understanding the underlying mechanisms can help patients and clinicians address these symptoms appropriately.
The medication works by mimicking the incretin hormone GLP-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, and slows gastric emptying. This delayed gastric emptying is central to semaglutide's appetite-suppressing effects but can also contribute to reduced food intake. When caloric consumption drops significantly—sometimes more rapidly than intended—patients may experience energy deficits that manifest as weakness or fatigue.
Additionally, semaglutide's gastrointestinal effects, including nausea, vomiting, and diarrhea, are among the most commonly reported adverse reactions according to FDA prescribing information. These symptoms can lead to reduced food intake and fluid/electrolyte losses, both of which contribute to feelings of weakness. The delayed gastric emptying may also affect the absorption of certain oral medications taken concurrently.
It is important to note that fatigue is specifically listed as a common adverse reaction in clinical trials for Wegovy (occurring in ≥5% of patients). While the medication does not directly cause muscle weakness through a neuromuscular mechanism, the combination of fatigue, gastrointestinal symptoms, rapid weight loss, and dietary changes associated with semaglutide therapy creates a clinical context where weakness can reasonably occur as a secondary phenomenon.
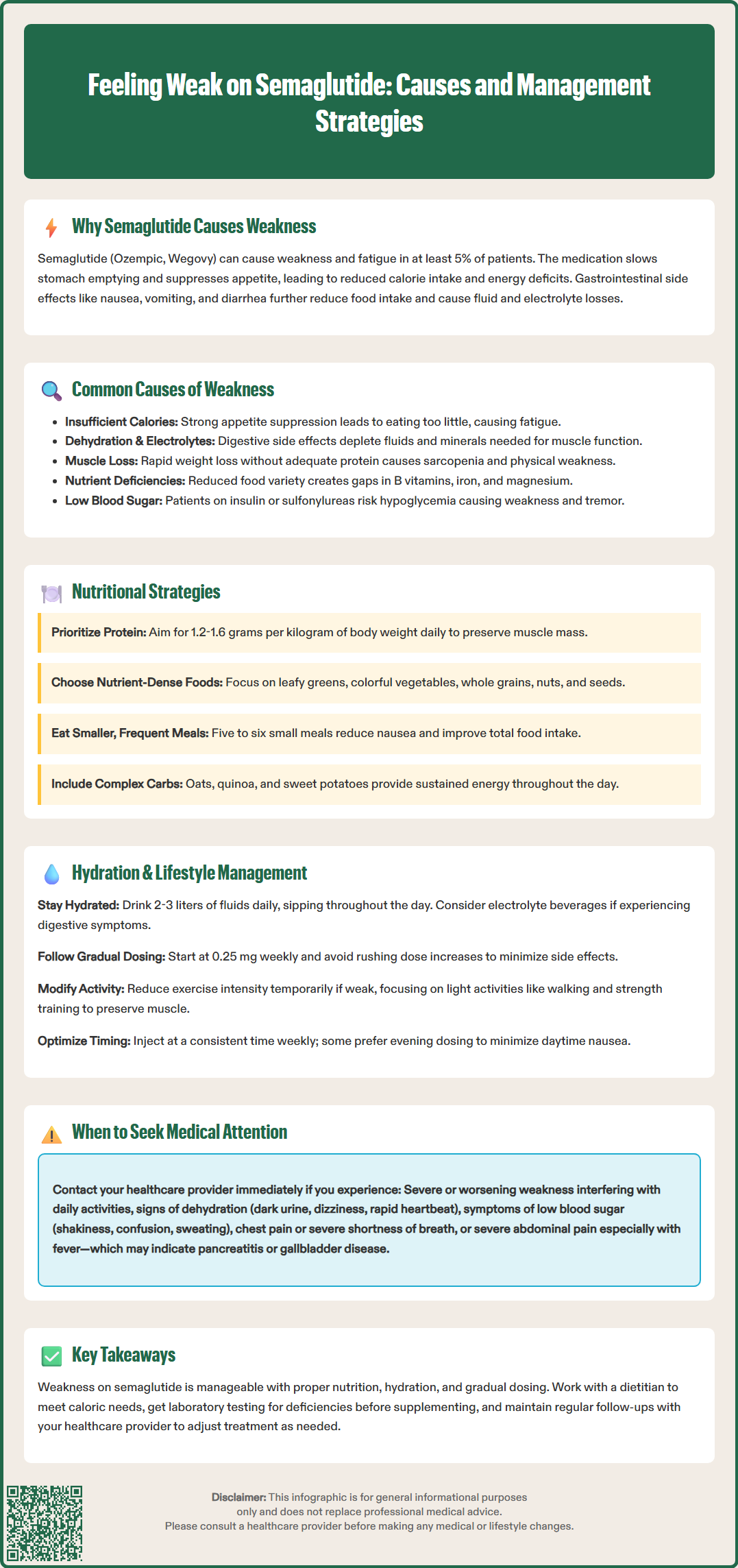
Several interconnected factors contribute to weakness in patients taking semaglutide, most of which relate to the medication's intended effects on appetite and metabolism rather than direct toxicity.
Insufficient Caloric Intake: The most common cause of weakness is inadequate energy consumption. Semaglutide's appetite suppression can be profound, leading some patients to consume significantly fewer calories than their bodies require for daily activities. This energy deficit, while promoting weight loss, can result in fatigue, lightheadedness, and generalized weakness, particularly during the initial weeks of treatment or after dose escalation.
Dehydration and Electrolyte Imbalance: Gastrointestinal side effects—especially nausea, vomiting, and diarrhea—can lead to fluid and electrolyte losses. Dehydration reduces blood volume and can cause orthostatic hypotension (dizziness upon standing), while electrolyte disturbances affect muscle function and energy metabolism. Patients may not recognize mild dehydration as a contributor to their fatigue.
Hypoglycemia: Although semaglutide alone rarely causes hypoglycemia due to its glucose-dependent mechanism, patients taking concurrent insulin or sulfonylureas face increased risk. Low blood sugar episodes can present with weakness, tremor, confusion, and sweating. The American Diabetes Association recommends dose adjustments of these medications when initiating GLP-1 receptor agonists.
Rapid Weight Loss and Muscle Loss: Caloric restriction without adequate protein intake can lead to loss of lean muscle mass alongside fat loss. This sarcopenia contributes to physical weakness and reduced exercise tolerance. Resistance training and adequate protein intake can help preserve muscle mass during weight loss.
Nutrient Deficiencies: Reduced food variety and quantity can lead to deficiencies in essential vitamins and minerals—particularly B vitamins, iron, and magnesium—all of which play crucial roles in energy metabolism and can cause fatigue when depleted.
Underlying Conditions: Persistent fatigue may also be due to coexisting conditions unrelated to semaglutide, such as anemia, thyroid dysfunction, vitamin B12 deficiency, or vitamin D deficiency. These should be evaluated if weakness persists despite addressing nutritional and hydration needs.
While mild fatigue during the initial adjustment period may be manageable with dietary modifications, certain presentations of weakness warrant prompt medical evaluation to rule out serious complications.
Severe or Progressive Weakness: Weakness that worsens over time, interferes with activities of daily living, or is accompanied by muscle pain may indicate significant electrolyte abnormalities or other serious conditions. Patients should seek care if they develop severe muscle pain or marked weakness that impacts daily function.
Signs of Dehydration: Symptoms including decreased urination, dark concentrated urine, persistent dizziness, rapid heartbeat, or confusion indicate significant fluid depletion requiring medical assessment. Severe dehydration can lead to acute kidney injury, a recognized risk with GLP-1 receptor agonists in the setting of volume depletion, as noted in FDA prescribing information.
Hypoglycemic Symptoms: Patients experiencing shakiness, confusion, sweating, or weakness that improves with food intake should check blood glucose levels if possible and contact their healthcare provider. Dose adjustments of concurrent diabetes medications may be necessary.
Cardiovascular Symptoms: Weakness accompanied by chest pain, severe shortness of breath, or palpitations requires emergency evaluation. While semaglutide has demonstrated cardiovascular benefits in clinical trials, individual patients may experience complications unrelated to the medication that require assessment.
Persistent Gastrointestinal Symptoms: Inability to maintain adequate oral intake due to severe nausea or vomiting lasting more than 24-48 hours necessitates medical attention. The FDA prescribing information warns about the risk of acute kidney injury in this setting, and patients may require intravenous fluids or temporary medication discontinuation.
Abdominal Pain: Severe, persistent abdominal pain, especially if radiating to the back and accompanied by vomiting, requires immediate medical attention as it may indicate pancreatitis, a rare but serious adverse effect noted in FDA warnings. Similarly, right upper quadrant pain, fever, or jaundice could signal gallbladder disease, which occurs at higher rates in patients taking semaglutide.
Proactive strategies can minimize weakness and fatigue while maintaining the therapeutic benefits of semaglutide for diabetes management or weight loss.
Gradual Dose Titration: Following the FDA-approved dosing schedule is essential. For Ozempic, this means starting at 0.25 mg weekly for four weeks before increasing to 0.5 mg, with further increases to 1.0 mg and potentially 2.0 mg if needed for glycemic control. Wegovy follows a more gradual escalation: 0.25 mg weekly for 4 weeks, then 0.5 mg, 1.0 mg, 1.7 mg, and finally 2.4 mg, with each step lasting 4 weeks. Rushing dose increases amplifies gastrointestinal side effects and appetite suppression, increasing the risk of inadequate nutrition.
Maintaining Adequate Caloric Intake: Despite reduced appetite, patients should aim to meet individualized caloric requirements. Working with a registered dietitian can help establish appropriate targets that promote healthy weight loss (typically a 500-750 calorie daily deficit) while preventing excessive energy deficits. Caloric needs vary significantly based on age, sex, activity level, and medical conditions.
Hydration Strategies: Patients should maintain adequate fluid intake based on individual needs, typically 2-3 liters daily for most adults, with adjustments for activity level, climate, and medical conditions. Sipping fluids throughout the day may be better tolerated than large volumes at once. Electrolyte-containing beverages can help maintain sodium and potassium balance, particularly if gastrointestinal symptoms are present, though patients with diabetes, hypertension, or kidney disease should be cautious about added sugars and sodium.
Physical Activity Modification: While exercise is important for overall health and muscle preservation, patients experiencing significant weakness may need to temporarily reduce intensity. Light to moderate activity—such as walking—is generally well-tolerated and can actually improve energy levels over time. Strength training helps preserve muscle mass during weight loss.
Medication Timing and Interactions: Taking semaglutide at a consistent time each week and planning injection timing around social events or important activities can help patients manage side effects. Some patients find that injecting in the evening minimizes daytime nausea. Clinicians should review all medications, as semaglutide's effect on gastric emptying may affect the absorption of oral medications, particularly those with a narrow therapeutic index.
Optimizing nutrition becomes particularly important when appetite is suppressed, as patients must obtain essential nutrients from smaller food volumes.
Prioritize Protein Intake: Adequate protein is crucial for preserving lean muscle mass during weight loss. The Dietary Reference Intake recommends a minimum of 0.8 grams of protein per kilogram of body weight daily for adults. During weight loss, higher amounts (1.2-1.6 g/kg) may help preserve lean mass, though this should be individualized based on age, kidney function, and other health factors. Protein-rich foods include lean meats, fish, eggs, Greek yogurt, legumes, and protein supplements if needed. Distributing protein across meals supports muscle protein synthesis better than consuming it all at once.
Focus on Nutrient Density: Every bite should deliver maximum nutritional value. Emphasize whole foods rich in vitamins and minerals: leafy greens, colorful vegetables, fruits, whole grains, nuts, and seeds. These provide B vitamins essential for energy metabolism, iron for oxygen transport, and magnesium for muscle function. Patients struggling with solid food intake might benefit from smoothies incorporating fruits, vegetables, protein powder, and healthy fats.
Strategic Carbohydrate Consumption: While semaglutide improves glycemic control, patients still need adequate carbohydrates for energy. Complex carbohydrates—such as oats, quinoa, sweet potatoes, and whole grain bread—provide sustained energy release and important fiber. Timing carbohydrate intake around physical activity can optimize energy availability when needed most.
Address Micronutrient Needs: Consider laboratory testing to identify specific deficiencies before starting supplements. Common tests include complete blood count, iron studies, vitamin B12, and vitamin D levels. Based on results, a healthcare provider may recommend targeted supplementation or a high-quality multivitamin to cover potential gaps, particularly if food variety is limited.
Small, Frequent Meals: Rather than three large meals, eating five to six smaller portions throughout the day may improve total intake and reduce nausea. Keeping easy-to-digest, protein-rich snacks readily available—such as cheese, nuts, hard-boiled eggs, or protein bars—ensures patients can maintain nutrition even when appetite is minimal.
Fatigue is listed as a common adverse reaction in clinical trials for Wegovy, occurring in ≥5% of patients. Weakness typically results from reduced caloric intake, gastrointestinal side effects, and dehydration rather than direct neuromuscular effects of the medication.
During weight loss on semaglutide, aim for 1.2-1.6 grams of protein per kilogram of body weight daily to help preserve lean muscle mass and prevent weakness. This should be individualized based on age, kidney function, and other health factors in consultation with your healthcare provider.
Seek medical attention if you experience severe or worsening weakness that interferes with daily activities, signs of dehydration (decreased urination, dizziness, confusion), symptoms of low blood sugar, persistent vomiting preventing adequate oral intake, or severe abdominal pain that could indicate pancreatitis.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.