LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 cause muscle pain? This question arises frequently as GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) become increasingly prescribed for type 2 diabetes and weight management. While muscle pain is not listed as a common side effect in FDA prescribing information, some patients report muscle discomfort during treatment. Understanding whether these symptoms result from direct drug effects, rapid weight loss, or other factors is essential for patients and clinicians. This article examines the evidence linking GLP-1 medications to muscle pain, explores potential mechanisms, and provides guidance on when to seek medical attention and how to manage symptoms effectively.
Quick Answer: Muscle pain is not a recognized common side effect of GLP-1 receptor agonists based on FDA prescribing information and clinical trial data, though some patients report muscle discomfort likely related to rapid weight loss and muscle mass reduction rather than direct drug toxicity.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for chronic weight management. These agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, though these medications are often collectively referred to as incretin-based therapies.
The primary mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release. Additionally, these medications slow gastric emptying and act on central nervous system pathways to promote satiety, contributing to their weight loss effects. In clinical trials, specific agents have demonstrated significant benefits in glycemic control, with some (liraglutide, semaglutide, and dulaglutide) showing cardiovascular risk reduction in dedicated outcome trials.
The most commonly reported adverse effects are gastrointestinal in nature. According to FDA prescribing information, nausea occurs in 15–44% of patients depending on the specific agent and dose, with vomiting, diarrhea, constipation, and abdominal pain also frequently reported. These symptoms typically emerge during dose escalation and often diminish over several weeks as tolerance develops. Other recognized adverse effects include injection site reactions, increased heart rate, pancreatitis, and gallbladder disease. Severe gastrointestinal symptoms may lead to dehydration and acute kidney injury in some patients.
These medications carry a boxed warning regarding thyroid C-cell tumor risk observed in rodent studies and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Hypoglycemia risk is generally low when used as monotherapy but increases when combined with insulin or sulfonylureas.
While gastrointestinal symptoms dominate the adverse effect profile, patients and clinicians have increasingly questioned whether these medications might contribute to musculoskeletal complaints, including muscle pain, weakness, or discomfort. Understanding the relationship between these medications and muscle-related symptoms requires careful examination of available evidence and clinical experience.
Muscle pain (myalgia) is not listed as a common adverse effect in the FDA-approved prescribing information for most GLP-1 receptor agonists. Systematic reviews of clinical trial data do not identify myalgia as occurring at significantly higher rates in GLP-1-treated patients compared to placebo groups. However, this does not definitively exclude the possibility of muscle-related symptoms in individual patients, as clinical trials may not capture all real-world experiences, particularly uncommon or delayed adverse effects.
Post-marketing surveillance and case reports have documented isolated instances of patients reporting muscle pain, cramping, or weakness while taking GLP-1 medications, though establishing a direct causal relationship remains challenging. The FDA Adverse Event Reporting System (FAERS) contains reports of musculoskeletal complaints associated with GLP-1 use, but such reports do not prove causation and may reflect coincidental associations or other contributing factors.
More concerning from a clinical perspective is the potential for lean mass loss associated with rapid weight reduction. Studies examining body composition changes during GLP-1 therapy, including the STEP trials (semaglutide) and SURMOUNT-1 (tirzepatide), have demonstrated that approximately 25–40% of total weight lost may come from lean body mass, including skeletal muscle, rather than exclusively from fat mass. This proportional muscle loss is consistent with weight loss from any cause, including dietary restriction or bariatric surgery, but the rapidity of weight loss with these medications may make this effect more clinically apparent.
There is no established pharmacological mechanism by which GLP-1 receptor activation would directly cause muscle pain or damage. GLP-1 receptors are expressed primarily in pancreatic islets, the gastrointestinal tract, kidney, heart, and certain brain regions, with limited expression in skeletal muscle tissue. Unlike statins, which can cause myopathy through effects on muscle cell membranes and mitochondrial function, GLP-1 agonists do not have a known direct myotoxic mechanism. Therefore, when muscle symptoms occur in patients taking these medications, clinicians should consider indirect mechanisms and alternative explanations rather than assuming direct drug-induced muscle toxicity.
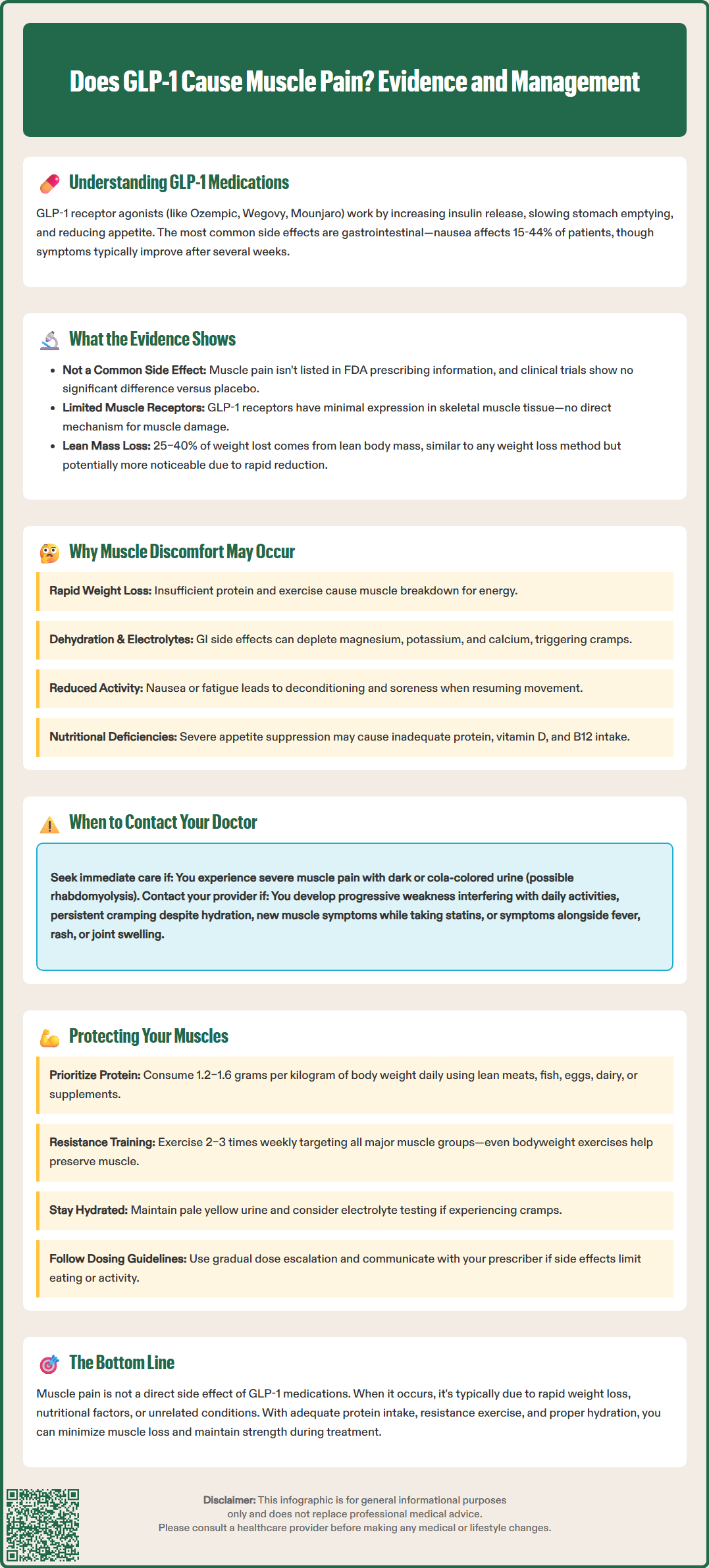
Several indirect mechanisms may explain why some patients report muscle pain or weakness while taking GLP-1 medications, even in the absence of direct myotoxicity. Understanding these contributing factors is essential for appropriate clinical assessment and management.
Rapid weight loss and muscle catabolism represent the most plausible explanation for muscle-related symptoms. When caloric intake decreases substantially—as commonly occurs with GLP-1 therapy due to appetite suppression and early satiety—the body mobilizes both fat and muscle tissue for energy. Without adequate protein intake and resistance exercise, muscle loss accelerates. Patients may experience this as generalized weakness, reduced exercise tolerance, or muscle discomfort, particularly during physical activity. The muscle loss is not due to direct drug toxicity but rather to the metabolic consequences of significant caloric restriction.
Dehydration and electrolyte disturbances may contribute to muscle cramping and discomfort. Gastrointestinal side effects, particularly nausea, vomiting, and diarrhea, can lead to reduced fluid intake and increased losses. Dehydration affects muscle function and may precipitate cramping. Additionally, rapid weight loss can alter electrolyte balance, with potential effects on neuromuscular function. Magnesium, potassium, and calcium imbalances have all been associated with muscle cramping and weakness. Note that magnesium levels are not included in standard comprehensive metabolic panels and require separate testing.
Reduced physical activity often accompanies the initial weeks of GLP-1 therapy when gastrointestinal symptoms are most prominent. Patients feeling nauseated or fatigued may decrease their usual exercise routines, leading to deconditioning. When they resume activity, they may experience muscle soreness or weakness that reflects deconditioning rather than drug-induced myopathy.
Nutritional deficiencies can develop when appetite suppression leads to inadequate intake of essential nutrients. Insufficient protein consumption impairs muscle protein synthesis and repair. Deficiencies in vitamin D, vitamin B12, or other micronutrients may contribute to muscle weakness or discomfort. Vitamin B12 deficiency is particularly relevant in patients also taking metformin, which can reduce B12 absorption over time. These nutritional concerns are particularly relevant in patients experiencing prolonged or severe appetite suppression.
Clinicians should also consider alternative diagnoses when evaluating muscle complaints in patients taking GLP-1 medications. Hypothyroidism, vitamin D deficiency, inflammatory myopathies, fibromyalgia, and other musculoskeletal conditions may coincidentally present during GLP-1 therapy. Additionally, patients taking multiple medications should be evaluated for potential drug interactions or additive effects, particularly if they are also taking statins, which have well-established myopathic potential.
While mild muscle discomfort during weight loss may not require immediate medical attention, certain features warrant prompt clinical evaluation to exclude serious underlying conditions. Patients should be counseled to contact their healthcare provider if they experience specific warning signs.
Severe or progressive muscle weakness that interferes with daily activities—such as difficulty climbing stairs, rising from a chair, or lifting objects—requires medical assessment. Progressive proximal muscle weakness (affecting shoulders and hips more than hands and feet) may indicate an inflammatory myopathy or other serious neuromuscular condition that requires investigation beyond simply attributing symptoms to GLP-1 therapy.
Muscle pain accompanied by dark urine is a critical warning sign of rhabdomyolysis, a potentially life-threatening condition involving rapid muscle breakdown. While rhabdomyolysis has not been established as a recognized complication of GLP-1 medications, any patient presenting with severe muscle pain and dark or cola-colored urine requires emergency medical attention. Patients should go to the emergency room or call 911 if they experience these symptoms, especially if accompanied by confusion or inability to keep fluids down. Rhabdomyolysis can lead to acute kidney injury and requires immediate intervention, including measurement of creatine kinase (CK) levels and assessment of renal function.
Persistent muscle cramping that does not respond to hydration and electrolyte repletion, or cramping that significantly disrupts sleep or daily function, warrants medical evaluation. While occasional muscle cramps are common and often benign, persistent or severe cramping may indicate electrolyte imbalances, peripheral neuropathy, or other underlying conditions requiring specific treatment.
Patients should also seek medical advice if muscle symptoms are accompanied by systemic features such as fever, unexplained weight loss beyond what is expected from GLP-1 therapy, rash, joint swelling, or other concerning signs that might suggest inflammatory or autoimmune conditions. Additionally, any new or worsening symptoms that cause significant concern or impair quality of life merit discussion with a healthcare provider.
Patients taking statins who develop new muscle symptoms while on GLP-1 therapy should contact their prescriber promptly, as this combination may increase the risk of muscle-related adverse effects in some individuals.
Before the appointment, patients should document the timing, location, and character of their muscle symptoms, any associated factors (such as relationship to exercise or time of day), and any other new symptoms. This information helps clinicians determine whether symptoms are likely related to GLP-1 therapy, represent expected consequences of weight loss, or suggest an alternative diagnosis requiring specific investigation.
For patients experiencing muscle discomfort or weakness while taking GLP-1 medications, several evidence-based strategies can help minimize symptoms while maintaining the therapeutic benefits of treatment.
Optimizing protein intake is the most important intervention to preserve muscle mass during weight loss. Current evidence suggests that patients losing weight should consume adequate protein daily, with targets typically ranging from 1.2–1.6 grams of protein per kilogram of body weight, individualized based on age, activity level, and kidney function. Patients with chronic kidney disease require individualized protein recommendations from a registered dietitian. High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and plant-based protein supplements. Consuming adequate protein supports muscle protein synthesis and helps offset the catabolic effects of caloric restriction. Patients struggling with appetite suppression may benefit from protein supplementation through shakes or powders to meet their targets without excessive volume of food.
Resistance exercise training is essential for maintaining muscle mass and strength during weight loss. The U.S. Department of Health and Human Services Physical Activity Guidelines and American College of Sports Medicine recommend resistance training at least two to three times weekly, targeting all major muscle groups. Even modest resistance exercise—using body weight, resistance bands, or light weights—can significantly reduce muscle loss during caloric restriction. Patients should be encouraged to work with physical therapists or exercise professionals to develop appropriate programs, particularly if they are deconditioned or have mobility limitations.
Adequate hydration and electrolyte balance help prevent muscle cramping and support overall muscle function. Patients should maintain adequate fluid intake based on individual needs, with attention to urine color (pale yellow indicates adequate hydration). Those experiencing significant gastrointestinal symptoms may benefit from oral rehydration solutions containing electrolytes. For muscle cramping, clinicians should first assess for electrolyte abnormalities, including magnesium, calcium, and potassium, before considering supplementation. Magnesium supplementation should be individualized based on laboratory results rather than routinely recommended, particularly in patients with kidney disease.
Gradual dose escalation of GLP-1 medications, following FDA-approved titration schedules, helps minimize gastrointestinal side effects that may indirectly contribute to muscle symptoms through reduced intake and activity. Patients should not rush dose increases and should communicate with their prescribers if side effects are limiting their ability to maintain adequate nutrition or physical activity.
If muscle symptoms are severe or persistent despite these interventions, clinicians should consider laboratory evaluation including creatine kinase, comprehensive metabolic panel with separate magnesium and calcium testing, thyroid function tests, vitamin D levels, and vitamin B12 levels to exclude alternative diagnoses. For suspected inflammatory conditions, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be appropriate. In select cases, temporary dose reduction or treatment interruption may be necessary while investigating symptoms, though this decision should be made collaboratively between patient and provider, weighing the benefits of continued therapy against symptom burden. Referral to neurology or rheumatology may be appropriate if initial evaluation suggests inflammatory or neuromuscular pathology beyond the expected effects of weight loss.
No established mechanism exists for GLP-1 receptor agonists to directly cause muscle damage or toxicity. Unlike statins, these medications do not have known myotoxic effects on muscle cells.
Muscle weakness typically results from loss of lean body mass during rapid weight loss, with approximately 25–40% of total weight lost coming from muscle rather than fat. Inadequate protein intake, reduced physical activity, and dehydration may also contribute.
Consume adequate protein (1.2–1.6 grams per kilogram of body weight daily) and perform resistance exercise training at least two to three times weekly targeting all major muscle groups. These strategies help preserve muscle mass during weight loss.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.