LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide for sleep apnea represents an emerging area of clinical interest as researchers investigate whether this GLP-1 receptor agonist can improve obstructive sleep apnea (OSA) through substantial weight loss. While semaglutide is FDA-approved for chronic weight management in adults with obesity, it does not currently have specific approval for treating sleep apnea. Given that approximately 70% of OSA patients are overweight or obese, and weight reduction of 10-15% can significantly improve breathing during sleep, medications that promote meaningful weight loss may offer adjunctive benefits alongside standard treatments like CPAP therapy.
Quick Answer: Semaglutide is not FDA-approved for sleep apnea but may indirectly improve obstructive sleep apnea through its approved weight loss effects in adults with obesity.
Obstructive sleep apnea (OSA) is a common breathing disorder characterized by repeated episodes of partial or complete upper airway collapse during sleep, leading to intermittent hypoxemia and sleep fragmentation. The condition affects approximately 30 million adults in the United States, though many cases remain undiagnosed. Patients typically present with loud snoring, witnessed apneas, excessive daytime sleepiness, morning headaches, and difficulty concentrating.
Obesity represents the single most important modifiable risk factor for OSA, with approximately 70% of OSA patients being overweight or obese. Excess adipose tissue in the neck and pharyngeal regions contributes to airway narrowing, while abdominal obesity increases mechanical load on the respiratory system and reduces lung volumes. The relationship is bidirectional—OSA itself may promote weight gain through sleep disruption, hormonal dysregulation, and reduced physical activity due to daytime fatigue.
The severity of OSA is quantified using the apnea-hypopnea index (AHI), which measures the number of breathing interruptions per hour of sleep. According to American Academy of Sleep Medicine (AASM) criteria, mild OSA is defined as 5-14 events per hour, moderate as 15-29 events per hour, and severe as 30 or more events per hour. Standard treatment includes positive airway pressure therapy (PAP, with CPAP being most common) as first-line for moderate to severe OSA, oral appliances, positional therapy, weight loss interventions, upper airway surgery, and hypoglossal nerve stimulation in selected patients. CPAP adherence can be challenging, with variable discontinuation rates across different populations.
Weight reduction of 10-15% can significantly improve OSA severity and may achieve remission in some patients with mild to moderate disease, as demonstrated in studies like Sleep AHEAD. Patients with concerning symptoms such as drowsy driving, near-miss accidents, uncontrolled daytime sleepiness affecting safety, or refractory hypertension should be promptly referred to a sleep medicine specialist. This connection between weight loss and respiratory improvement has generated interest in pharmacological weight loss interventions, particularly glucagon-like peptide-1 (GLP-1) receptor agonists, as potential adjunctive options for OSA management.
Semaglutide is a long-acting GLP-1 receptor agonist that mimics the action of endogenous GLP-1, an incretin hormone released from intestinal L-cells in response to food intake. The medication was initially developed for type 2 diabetes management but has demonstrated remarkable efficacy for weight reduction. Semaglutide is available in two formulations: a once-weekly subcutaneous injection (Wegovy for chronic weight management, Ozempic for diabetes) and a daily oral tablet (Rybelsus for diabetes only, not indicated for weight management).
The mechanism of action involves multiple pathways that collectively promote weight loss. Semaglutide activates GLP-1 receptors in the hypothalamus and brainstem, reducing appetite and increasing satiety signals. It slows gastric emptying, prolonging the feeling of fullness after meals. Additionally, the medication influences reward pathways in the brain, potentially reducing food cravings and hedonic eating behaviors. In controlled clinical studies, these effects have been associated with reduced caloric intake, though the magnitude varies among individuals.
Clinical trials have demonstrated substantial weight loss with semaglutide therapy. The STEP (Semaglutide Treatment Effect in People with obesity) trial program showed that patients receiving semaglutide 2.4 mg weekly achieved average weight reductions of 12-15% over 68 weeks, compared to 2-3% with placebo. Approximately one-third of participants lost 20% or more of their initial body weight. These results represent weight loss magnitudes that approach those of some bariatric procedures, though typically less than what is achieved with bariatric surgery.
Beyond weight reduction, semaglutide improves multiple cardiometabolic parameters including glycemic control, blood pressure, lipid profiles, and inflammatory markers. The medication reduces hemoglobin A1c by 1-2% in patients with diabetes and has demonstrated cardiovascular benefits in high-risk populations in trials such as SUSTAIN-6 and SELECT. Some of these metabolic improvements may occur partly independently of weight loss, as suggested by mediation analyses from cardiovascular outcome trials, potentially reflecting effects on insulin sensitivity and vascular health that may be relevant for patients with obesity-related comorbidities like sleep apnea.
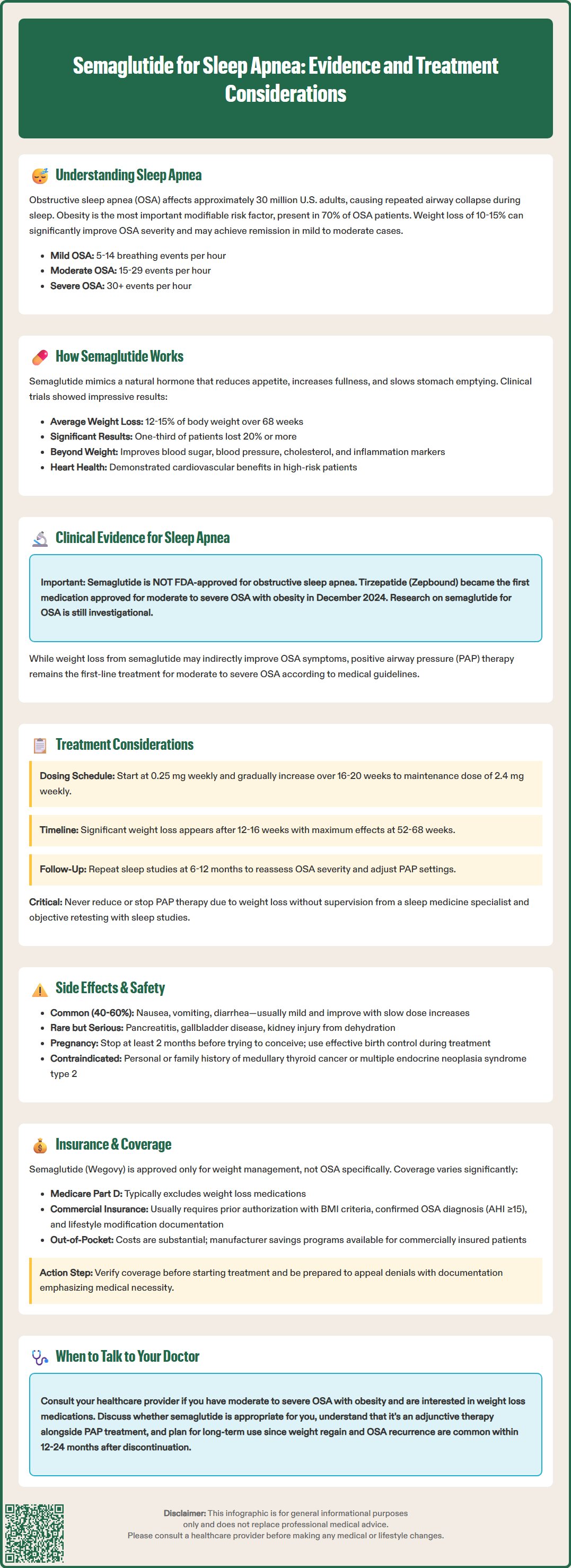
As of 2025, semaglutide is not FDA-approved for obstructive sleep apnea. In December 2024, tirzepatide (Zepbound) became the first medication to receive FDA approval specifically for moderate to severe OSA in adults with obesity, based on the SURMOUNT-OSA clinical trials.
Research on semaglutide's effects on OSA is ongoing, with several clinical trials investigating its impact on sleep-disordered breathing. Preliminary data and press releases suggest potential benefits, though published peer-reviewed results from dedicated OSA trials with semaglutide are still emerging. Any discussion of semaglutide for OSA should be considered investigational and not based on an FDA-approved indication.
The weight loss achieved with semaglutide may indirectly benefit OSA, as substantial weight reduction is known to improve respiratory parameters in many patients with obesity and sleep-disordered breathing. However, the specific magnitude of AHI improvement with semaglutide should not be assumed to match that of other medications like tirzepatide, which has demonstrated significant reductions in AHI in its pivotal trials.
It is important to emphasize that positive airway pressure therapy (PAP) remains the first-line treatment for moderate to severe OSA according to AASM guidelines. Any consideration of reducing or discontinuing PAP therapy due to weight loss should occur only under the supervision of a sleep medicine specialist and following objective reassessment with polysomnography or home sleep apnea testing. The relationship between weight loss and OSA improvement varies considerably between individuals, and some patients may continue to require PAP therapy despite significant weight reduction.
Semaglutide for weight management should be considered as part of a comprehensive approach to patients with both obesity and OSA. According to current guidelines, PAP therapy remains first-line treatment for moderate to severe OSA. Semaglutide may be used as an adjunctive therapy for its FDA-approved indication of chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity.
Treatment initiation follows a gradual dose escalation protocol to minimize gastrointestinal side effects. Per the Wegovy Prescribing Information, the typical regimen begins with 0.25 mg weekly for four weeks, increasing monthly through 0.5 mg, 1.0 mg, 1.7 mg, and finally to the target maintenance dose of 2.4 mg weekly. This escalation period spans approximately 16-20 weeks. Patients should receive concurrent lifestyle counseling emphasizing nutrition, physical activity, and behavioral strategies to optimize outcomes and maintain weight loss long-term.
Realistic expectations regarding timeline and magnitude of improvement are essential. Significant weight loss typically becomes apparent after 12-16 weeks, with maximal effects observed at 52-68 weeks of continuous therapy. OSA improvements generally parallel weight reduction, though respiratory benefits may lag behind weight loss by several weeks. Patients should undergo repeat sleep studies (polysomnography or home sleep apnea testing) after achieving stable weight loss, typically at 6-12 months, to reassess OSA severity and guide adjustments to PAP settings or other therapies.
Substantial weight change (≥10% of body weight) warrants re-evaluation of OSA severity per AASM recommendations. Referral to a sleep medicine specialist is appropriate for titration of PAP therapy and comprehensive OSA management. Patients with BMI ≥35 kg/m² with comorbidities or BMI ≥40 kg/m² should also be considered for bariatric surgery evaluation.
Long-term treatment planning must address the chronic nature of both obesity and OSA. Clinical trial data suggest that weight regain and OSA recurrence are common after semaglutide discontinuation, with many patients returning toward baseline within 12-24 months. Therefore, semaglutide should generally be viewed as a long-term therapy rather than a short-term intervention. Ongoing monitoring should include assessment of weight trends, OSA symptoms, cardiovascular risk factors, and medication adherence at regular intervals, typically every 3-6 months after stabilization.
Semaglutide's safety profile is well-established from extensive clinical trial experience, though patients with sleep apnea warrant specific considerations. The most common adverse effects are gastrointestinal, occurring in 40-60% of patients and including nausea, vomiting, diarrhea, constipation, and abdominal discomfort. These symptoms are typically mild to moderate, most pronounced during dose escalation, and tend to diminish over time. Slow titration and dietary modifications (smaller, more frequent meals; avoiding high-fat foods) can help minimize GI intolerance.
More serious but less common adverse effects include:
Pancreatitis: Rare cases have been reported. Patients should be counseled to seek immediate medical attention for severe, persistent abdominal pain radiating to the back.
Gallbladder disease: Rapid weight loss increases cholelithiasis risk. Symptoms of biliary colic warrant evaluation.
Hypoglycemia: Risk is low with semaglutide monotherapy but increases when combined with insulin or sulfonylureas in diabetic patients.
Acute kidney injury: Typically related to severe dehydration from vomiting or diarrhea. Adequate hydration is essential.
Diabetic retinopathy complications: Rapid glycemic improvement may temporarily worsen retinopathy in patients with pre-existing disease. Ophthalmology follow-up is recommended for patients with diabetic retinopathy.
According to the Wegovy Prescribing Information, semaglutide is not recommended during pregnancy. The medication should be discontinued when pregnancy is recognized and at least 2 months before a planned pregnancy. Women of childbearing potential should use effective contraception during treatment.
The medication carries a boxed warning regarding thyroid C-cell tumors based on rodent studies, though human relevance remains uncertain. Semaglutide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2.
For perioperative management, the American Society of Anesthesiologists provides guidance on GLP-1 receptor agonists, which may be relevant for OSA patients undergoing procedures. Patients should discuss medication timing with their healthcare providers before surgery.
Regarding psychiatric effects, the FDA conducted a review in 2024 and did not find a clear causal association between GLP-1 receptor agonists and suicidal ideation, though monitoring for mood changes is still advised. Regular follow-up allows early identification and management of adverse effects, optimizing both safety and treatment adherence.
The FDA approval landscape for GLP-1 receptor agonists impacts insurance coverage for patients with OSA and obesity. As of 2025, tirzepatide (Zepbound) is FDA-approved for moderate to severe obstructive sleep apnea in adults with obesity, making it the first medication approved for this indication. Semaglutide (Wegovy) is FDA-approved for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, but does not have a specific OSA indication.
Insurance coverage varies substantially by indication, payer, and policy type. Medicare Part D plans traditionally exclude coverage for weight loss medications under the statutory "lifestyle drug" exclusion, though medications with FDA-approved non-obesity indications (such as tirzepatide for OSA) may have different coverage pathways. Some Medicare Advantage plans offer coverage for FDA-approved weight loss medications. Medicaid coverage varies by state, with coverage policies for GLP-1 receptor agonists continuing to evolve.
Commercial insurance coverage is highly variable. Many plans require prior authorization with documentation of:
BMI criteria matching FDA-approved indications
For OSA-specific coverage (with tirzepatide), documented OSA diagnosis with polysomnography or home sleep testing showing AHI ≥15
Participation in lifestyle modification programs
Absence of contraindications
Even with approval, coverage may include quantity limits, step therapy requirements (trying other weight loss medications first), or annual spending caps. Out-of-pocket costs for patients without coverage are substantial, making affordability a significant barrier. Manufacturers offer savings programs that may reduce costs for commercially insured patients who qualify, though eligibility criteria apply and these programs typically exclude government insurance beneficiaries. Patients should verify current terms and eligibility by visiting manufacturer websites or contacting their patient assistance programs directly.
Patients and clinicians should verify coverage before initiating therapy and be prepared to submit appeals with supporting documentation emphasizing medical necessity and potential cost savings from reduced OSA-related complications. As evidence and indications evolve, coverage policies may change, though access challenges are likely to persist given the medications' high cost and the prevalence of obesity and sleep apnea in the population.
No, semaglutide is not FDA-approved for obstructive sleep apnea. It is FDA-approved for chronic weight management in adults with obesity or overweight with weight-related comorbidities, and may indirectly benefit OSA through weight loss.
No, CPAP therapy remains first-line treatment for moderate to severe OSA. Any consideration of reducing or discontinuing CPAP should occur only under sleep medicine specialist supervision following objective reassessment with sleep studies after achieving stable weight loss.
Weight reduction of 10-15% can significantly improve OSA severity and may achieve remission in some patients with mild to moderate disease. Semaglutide produces average weight reductions of 12-15% over 68 weeks in clinical trials, though individual responses vary.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.