LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 give you heartburn? Many patients starting GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) wonder about this potential side effect. While nausea and vomiting are the most common gastrointestinal complaints, heartburn and acid reflux can occur in some patients. These medications slow gastric emptying to improve blood sugar control and promote weight loss, but this same mechanism may contribute to reflux symptoms. Understanding the connection between GLP-1 therapy and heartburn—and knowing how to manage it—can help you continue treatment safely and comfortably while achieving your diabetes or weight management goals.
Quick Answer: GLP-1 medications can cause heartburn in some patients, with dyspepsia and GERD reported in approximately 3-9% of users, primarily due to delayed gastric emptying that may promote acid reflux.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, chronic weight management. These agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), among others. Tirzepatide (Mounjaro, Zepbound) is a related but distinct medication that acts as a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor co-agonist. These medications work by mimicking the action of endogenous GLP-1, an incretin hormone released from the intestinal L-cells in response to food intake.
The pharmacological mechanism of GLP-1 receptor agonists involves several key actions. They enhance glucose-dependent insulin secretion from pancreatic beta cells, suppress inappropriate glucagon release from alpha cells, and slow gastric emptying. This delayed gastric emptying is particularly important for glycemic control and weight reduction, as it prolongs the sensation of fullness and reduces postprandial glucose excursions. With long-acting GLP-1 agents, this effect on gastric emptying may attenuate over time (tachyphylaxis). Additionally, these medications act on central appetite regulation centers in the hypothalamus, contributing to reduced caloric intake.
The slowing of gastric motility is dose-dependent and represents both a therapeutic benefit and a potential source of gastrointestinal adverse effects. By keeping food in the stomach longer, these medications help patients feel satisfied with smaller portions and experience more gradual rises in blood glucose after meals. However, this same mechanism can contribute to various upper gastrointestinal symptoms that patients may experience during treatment.
Importantly, GLP-1 receptor agonists are not recommended for patients with severe gastroparesis, as they may further delay gastric emptying and worsen symptoms. Understanding how these medications affect the digestive system is essential for both clinicians and patients, as it provides context for managing potential side effects while maximizing therapeutic benefits for diabetes control and weight management.
While nausea, vomiting, and diarrhea are the most commonly reported gastrointestinal adverse effects with GLP-1-based therapies (occurring in 15-40% of patients depending on the agent and dose), FDA prescribing information for several of these medications does list dyspepsia (indigestion) and, in some cases, gastroesophageal reflux disease (GERD) as reported adverse reactions. For example, clinical trials of semaglutide and tirzepatide report dyspepsia occurring in approximately 3-9% of patients, with GERD and belching/eructation also noted in some product labels.
The relationship between GLP-1 therapy and heartburn is likely related to the medication's effect on gastric emptying. Delayed gastric emptying can increase intragastric pressure and potentially promote gastroesophageal reflux, particularly in patients with pre-existing GERD or those who overeat despite reduced appetite signals. When food remains in the stomach for extended periods, there is increased opportunity for acidic gastric contents to reflux into the esophagus, especially when lying down or bending over.
It is important to note that there is no established direct causative mechanism linking GLP-1 receptor activation to increased gastric acid production or lower esophageal sphincter dysfunction. Most patients who experience heartburn on GLP-1 therapy have identifiable contributing factors, such as large meal portions, eating close to bedtime, or underlying GERD that may have been previously undiagnosed or inadequately managed.
Clinical trial data suggest that gastrointestinal side effects, including any reflux symptoms, typically improve over time as patients develop tolerance to the medication. Most symptoms are most pronounced during dose escalation phases and tend to diminish within 4-8 weeks of maintaining a stable dose. With long-acting GLP-1 agents, the effect on gastric emptying may diminish somewhat over time, which could reduce reflux symptoms in some patients. Patients with pre-existing GERD should be counseled about potential symptom exacerbation and monitored appropriately during GLP-1 initiation.
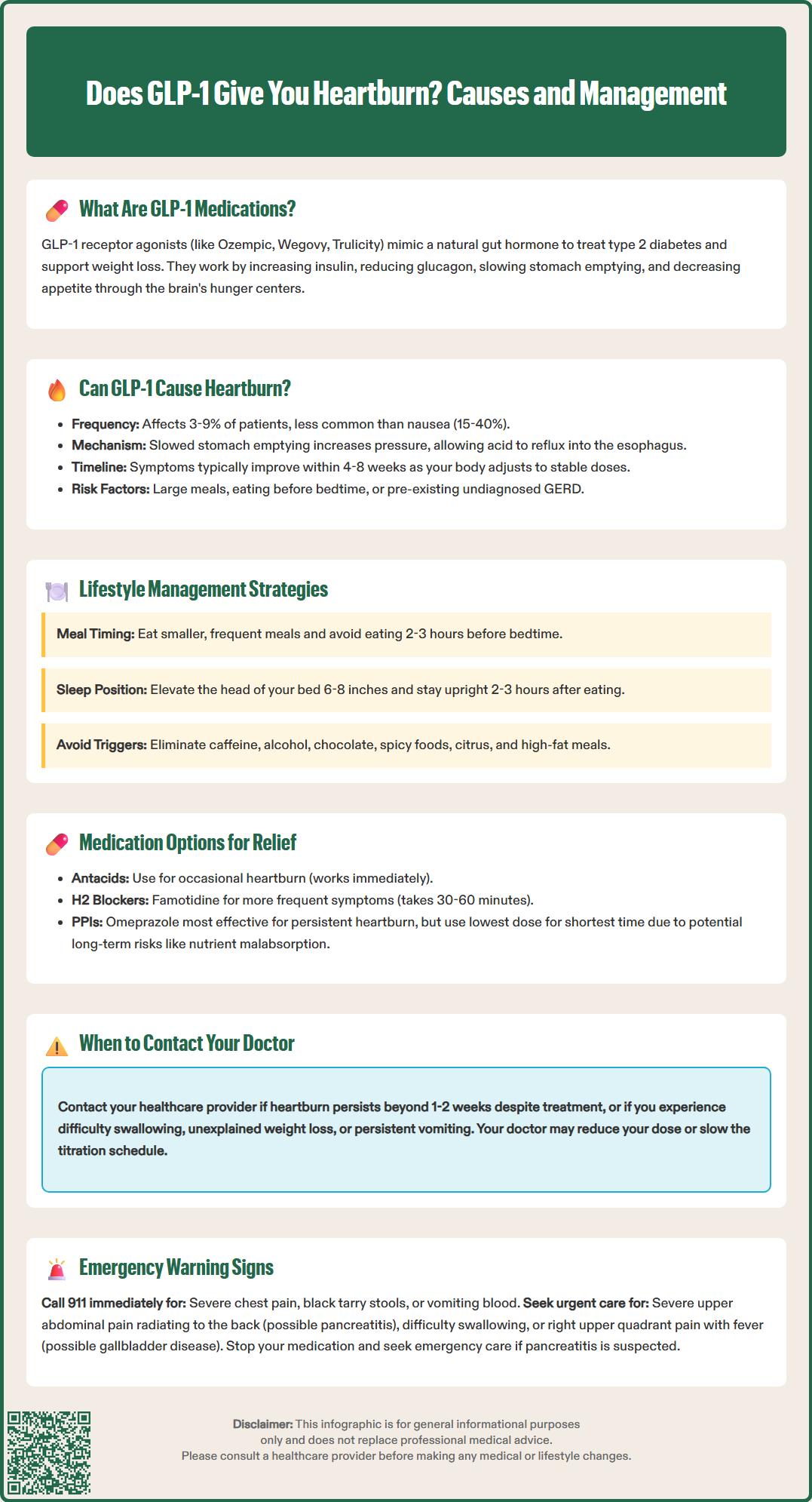
For patients experiencing heartburn while on GLP-1 therapy, several evidence-based management strategies can provide relief without necessitating medication discontinuation. Lifestyle modifications should be the first-line approach and include:
Eating smaller, more frequent meals rather than large portions that overwhelm the already-slowed digestive system
Avoiding eating within 2-3 hours of bedtime to allow adequate time for gastric emptying before lying down
Elevating the head of the bed by 6-8 inches using blocks or a wedge pillow to reduce nocturnal reflux
Identifying and avoiding trigger foods such as caffeine, alcohol, chocolate, spicy foods, citrus, and high-fat meals
Maintaining an upright posture for at least 2-3 hours after meals
Wearing loose-fitting clothing that doesn't compress the abdomen
Pharmacological management may be appropriate for patients with persistent symptoms despite lifestyle modifications. Over-the-counter antacids containing calcium carbonate or magnesium hydroxide can provide rapid, short-term relief for occasional heartburn. For more frequent symptoms, histamine-2 receptor antagonists (H2RAs) such as famotidine may be used, though patients should be counseled that these medications may take 30-60 minutes to provide relief.
Proton pump inhibitors (PPIs) such as omeprazole or esomeprazole represent the most effective option for managing persistent reflux symptoms. For over-the-counter PPIs, patients should follow FDA guidance: take once daily for up to 14 days, not more than 3 courses per year without physician supervision, and seek medical evaluation if symptoms persist beyond 14 days or recur frequently. For persistent GERD symptoms, physicians typically recommend an 8-week PPI trial, followed by step-down to the lowest effective dose.
PPIs should be used at the lowest effective dose for the shortest duration necessary, as long-term use has been associated with (though not proven to cause) potential effects including nutrient malabsorption, increased infection risk, and bone health concerns.
For patients with severe or persistent GI symptoms, temporary dose reduction or holding the GLP-1 medication (under clinician guidance) may be considered. Patients should be reassured that gastrointestinal symptoms often improve with continued therapy as tolerance develops. Slower dose titration schedules may be considered for patients with significant symptoms, allowing more time for adaptation at each dose level before escalation.
While mild heartburn can often be managed with lifestyle modifications and over-the-counter medications, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience severe or persistent heartburn that does not respond to conservative measures or over-the-counter treatments within 1-2 weeks, as this may indicate more significant gastroesophageal pathology requiring investigation.
Red flag symptoms requiring urgent medical attention include:
Severe, persistent abdominal pain, particularly in the upper abdomen or epigastric region, which could indicate pancreatitis (a rare but serious adverse effect of GLP-1 therapy)
Difficulty swallowing (dysphagia) or painful swallowing (odynophagia)
Unintentional weight loss beyond expected therapeutic effects
Persistent vomiting that prevents adequate oral intake or medication administration
Right upper quadrant pain, fever, or yellowing of skin/eyes, which could indicate gallbladder disease (a known risk with weight loss on GLP-1 therapies)
Symptoms of gastroparesis such as early satiety, postprandial fullness, or vomiting undigested food
Call 911 or seek emergency care immediately for:
Severe chest pain that could represent cardiac pathology rather than reflux
Evidence of gastrointestinal bleeding, including black, tarry stools or vomiting blood or coffee-ground material
If you suspect pancreatitis (persistent severe abdominal pain, sometimes radiating to the back, with or without nausea/vomiting), stop taking the GLP-1 medication immediately and seek urgent medical care, as directed in FDA prescribing information.
Patients with persistent heartburn despite optimal PPI therapy or those with alarm symptoms (difficulty swallowing, weight loss, anemia) should be referred for endoscopic evaluation according to clinical guidelines.
Patients with pre-existing gastrointestinal conditions, including GERD, peptic ulcer disease, or gastroparesis, should have closer monitoring during GLP-1 initiation and dose escalation. These individuals may require proactive management strategies and potentially slower titration schedules.
It is also important to contact your healthcare provider if heartburn symptoms significantly impact quality of life or medication adherence. In some cases, switching to a different GLP-1 agent or adjusting the dosing schedule may provide better tolerability. Your doctor can assess whether symptoms represent expected, manageable side effects or indicate a need for further investigation, dose adjustment, or alternative therapeutic approaches.
Heartburn and dyspepsia occur in approximately 3-9% of patients taking GLP-1 medications according to clinical trial data. This is less common than nausea or vomiting, and symptoms typically improve within 4-8 weeks as tolerance develops.
Yes, over-the-counter antacids, H2 blockers like famotidine, or proton pump inhibitors (PPIs) can be used to manage heartburn on GLP-1 therapy. For persistent symptoms, consult your healthcare provider about appropriate PPI use and duration.
Contact your healthcare provider if heartburn persists beyond 1-2 weeks despite lifestyle changes and over-the-counter treatments, or if you experience red flag symptoms including difficulty swallowing, severe abdominal pain, persistent vomiting, or signs of gastrointestinal bleeding.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.