LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Glucagon-like peptide-1 (GLP-1) receptor agonists have transformed type 2 diabetes and obesity management through proven effects on glucose control and weight reduction. As patients and clinicians explore these medications' broader metabolic impacts, questions arise about potential effects on cortisol—the stress hormone linked to central weight gain and insulin resistance. While GLP-1 therapies offer substantial benefits through well-established mechanisms, their influence on cortisol levels remains unclear. This article examines current evidence regarding GLP-1 and cortisol regulation, clarifies what these medications can and cannot do, and outlines appropriate approaches for managing cortisol-related metabolic concerns.
Quick Answer: GLP-1 receptor agonists are not established to directly lower cortisol levels in humans based on current clinical evidence.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) is an incretin hormone naturally produced by intestinal L-cells in response to nutrient intake. This peptide plays a crucial role in glucose homeostasis by stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. These physiological actions have made GLP-1 receptor agonists—synthetic medications that mimic endogenous GLP-1—valuable therapeutic agents for type 2 diabetes and obesity management.
FDA-approved GLP-1 receptor agonists include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications work primarily through pancreatic and central nervous system pathways. By binding to GLP-1 receptors in the hypothalamus, they reduce appetite and promote satiety, leading to significant weight reduction in clinical trials—with newer agents achieving approximately 15% weight loss in obesity without diabetes (semaglutide) and up to 21% (tirzepatide), with somewhat lower reductions typically seen in patients with type 2 diabetes.
Beyond glycemic control, emerging research suggests GLP-1 may influence multiple metabolic pathways, including inflammation, cardiovascular function, and potentially neuroendocrine regulation. Several GLP-1 receptor agonists have demonstrated cardiovascular benefits in specific populations, with varying magnitudes of risk reduction for major adverse cardiovascular events in landmark trials. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, and diarrhea, which typically diminish over time. Important safety considerations include risk of thyroid C-cell tumors (contraindicated in MEN2 or personal/family history of medullary thyroid carcinoma), pancreatitis, gallbladder disease, hypoglycemia when used with insulin or secretagogues, and potential worsening of diabetic retinopathy in some patients. Understanding GLP-1's broader metabolic effects remains an active area of investigation, particularly regarding its potential interactions with stress hormones like cortisol.
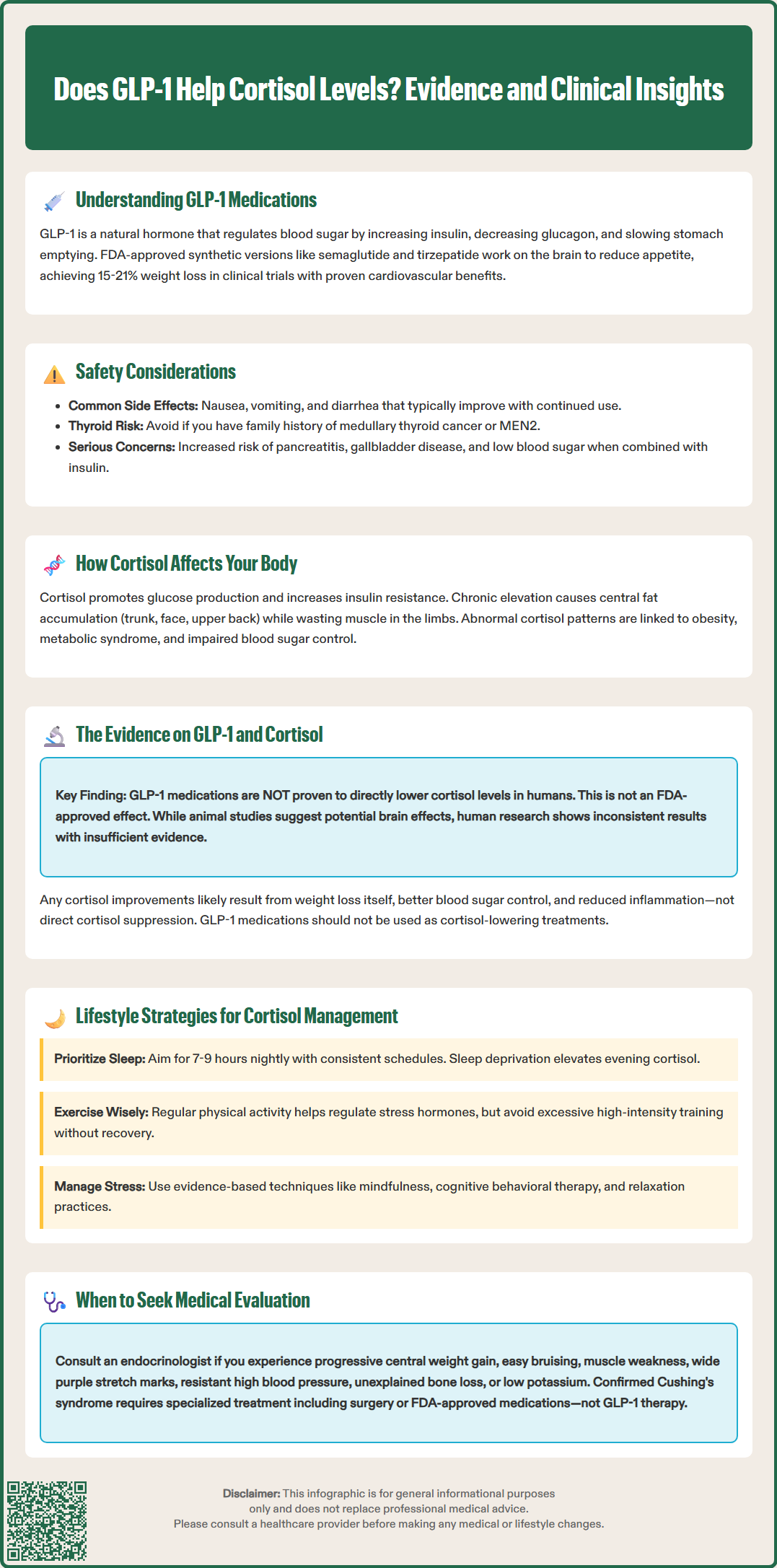
Cortisol, the primary glucocorticoid hormone produced by the adrenal cortex, serves essential functions in metabolism, immune regulation, and stress response. Released in a diurnal pattern with peak levels in early morning, cortisol influences carbohydrate, protein, and lipid metabolism through multiple mechanisms. It promotes gluconeogenesis in the liver, increases insulin resistance in peripheral tissues, and facilitates lipolysis while paradoxically promoting central adiposity when chronically elevated.
Chronic hypercortisolism—whether from endogenous Cushing's syndrome or exogenous glucocorticoid therapy—produces a characteristic metabolic phenotype. Patients develop central obesity with fat redistribution to the trunk, face, and dorsocervical region, alongside muscle wasting in the extremities. This occurs because cortisol preferentially stimulates adipocyte differentiation and lipid accumulation in visceral depots while promoting protein catabolism in skeletal muscle. Additionally, elevated cortisol impairs glucose tolerance and frequently causes secondary diabetes through increased hepatic glucose production and peripheral insulin resistance.
Observational studies have associated alterations in cortisol patterns, such as flattened diurnal curves or elevated evening levels, with obesity, metabolic syndrome, and cardiovascular risk, though these findings do not establish causality. While some research has examined hair cortisol concentrations as a potential marker of chronic stress, this is not a recommended clinical test in US practice. The hypothalamic-pituitary-adrenal (HPA) axis function often changes with chronic psychological stress, sleep deprivation, and depression—conditions themselves linked to weight gain and metabolic disease. Understanding cortisol's metabolic impact is clinically relevant because interventions targeting stress physiology might theoretically complement pharmacological weight management strategies, though the relationship between GLP-1 therapies and cortisol regulation requires careful examination of available evidence.
Currently, there is no established clinical evidence that GLP-1 receptor agonists directly lower cortisol levels in humans. The FDA-approved labeling for semaglutide, liraglutide, tirzepatide, and other GLP-1 medications does not list cortisol reduction as a mechanism of action or therapeutic effect. While these agents profoundly impact metabolic health through well-characterized pathways, their influence on HPA axis function and cortisol secretion remains inadequately studied in clinical populations.
Limited preclinical research has explored potential interactions between GLP-1 signaling and stress hormone pathways. Some animal studies suggest GLP-1 receptors exist in brain regions involved in stress response, including the hypothalamus and amygdala, raising theoretical possibilities for neuroendocrine modulation. However, translating these findings to human cortisol regulation requires substantial caution. The few human studies examining cortisol in patients receiving GLP-1 therapy have shown inconsistent results, with limited data quality and sample sizes preventing definitive conclusions about effects on basal cortisol levels or diurnal patterns.
One important consideration is that successful weight loss—regardless of method—may indirectly influence cortisol metabolism. Obesity itself is associated with altered cortisol clearance and tissue-specific cortisol activation through 11β-hydroxysteroid dehydrogenase type 1. Weight reduction can normalize some of these abnormalities, potentially improving metabolic outcomes through cortisol-independent mechanisms. Additionally, improvements in glycemic control, inflammation, and psychological well-being associated with GLP-1 therapy might secondarily affect stress physiology without directly suppressing cortisol secretion.
Clinicians should counsel patients that while GLP-1 medications offer proven benefits for diabetes and weight management, they should not be considered cortisol-lowering agents. Patients with suspected hypercortisolism require appropriate endocrine evaluation according to Endocrine Society guidelines, typically including at least two abnormal screening tests (24-hour urinary free cortisol, late-night salivary cortisol, or low-dose dexamethasone suppression testing) before confirmatory testing and specialist referral.
For patients with confirmed pathological hypercortisolism (Cushing's syndrome), definitive treatment depends on etiology and may include transsphenoidal surgery for pituitary adenomas, adrenalectomy for adrenal tumors, or medical therapy. FDA-approved medications for Cushing's syndrome include osilodrostat (Isturisa), levoketoconazole (Recorlev), pasireotide (Signifor), and mifepristone (Korlym)—the latter specifically indicated for hyperglycemia secondary to Cushing's syndrome. Ketoconazole is sometimes used off-label in the US. These conditions require endocrinologist management and cannot be adequately addressed through lifestyle modification alone.
However, for individuals with stress-related cortisol dysregulation—common in obesity and metabolic syndrome—evidence-based lifestyle interventions form the foundation of management. Sleep optimization is particularly important, as sleep deprivation elevates evening cortisol and disrupts normal diurnal rhythm. Adults should target 7-9 hours of quality sleep nightly, with consistent sleep-wake schedules. Regular physical activity helps regulate HPA axis function, though very high-intensity exercise without adequate recovery may temporarily increase cortisol levels in some individuals.
Stress management techniques with demonstrated efficacy include mindfulness-based stress reduction, cognitive behavioral therapy, and relaxation practices. These interventions can modestly reduce cortisol reactivity and improve diurnal patterns in stressed populations. Nutritional approaches emphasizing whole foods, adequate protein, and limited ultra-processed foods support overall metabolic health, though no specific diet directly lowers cortisol in a clinically meaningful way.
For patients pursuing weight management with GLP-1 therapy, addressing concurrent stress and sleep issues optimizes treatment outcomes. The American Diabetes Association recommends comprehensive lifestyle counseling alongside pharmacotherapy. Clinicians should screen for depression and anxiety disorders, which frequently coexist with obesity and may benefit from specific treatment. When cortisol-related symptoms persist despite lifestyle modification—including progressive central weight gain, easy bruising, proximal muscle weakness, wide purple striae, resistant hypertension, unexplained osteoporosis, or hypokalemia—formal endocrine evaluation is warranted to exclude pathological hypercortisolism requiring specialized intervention. Importantly, patients taking prescribed glucocorticoids should never stop them abruptly and should work with their healthcare provider on appropriate tapering when indicated.
Currently, there is no established clinical evidence that GLP-1 receptor agonists directly lower cortisol levels in humans. FDA labeling for these medications does not list cortisol reduction as a mechanism of action or therapeutic effect.
Chronically elevated cortisol promotes central obesity by stimulating fat accumulation in visceral depots while causing muscle wasting in the extremities. It also increases insulin resistance and hepatic glucose production, frequently leading to impaired glucose tolerance or diabetes.
Seek endocrine evaluation if you experience progressive central weight gain with easy bruising, proximal muscle weakness, wide purple striae, resistant hypertension, unexplained osteoporosis, or hypokalemia. These symptoms may indicate pathological hypercortisolism requiring specialized testing and treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.