LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide lower your immune system? This is a common concern among patients prescribed this medication for type 2 diabetes or weight management. Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is a GLP-1 receptor agonist that works primarily on metabolic pathways rather than immune function. Current clinical evidence from large-scale trials does not support claims that semaglutide suppresses immunity or increases infection risk. Understanding how this medication works and what the research shows can help patients make informed decisions about their treatment. This article examines the scientific evidence regarding semaglutide's effects on immune function, infection risk, and important safety considerations.
Quick Answer: Semaglutide does not lower or suppress immune system function based on current clinical evidence from large-scale trials and FDA safety data.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes and chronic weight management. It mimics the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. By binding to GLP-1 receptors throughout the body, semaglutide enhances insulin secretion when blood glucose levels are elevated, suppresses glucagon release, and slows gastric emptying.
These mechanisms work together to improve glycemic control in people with diabetes and promote weight loss by reducing appetite and caloric intake. Semaglutide is available in injectable forms as once-weekly subcutaneous injections under brand names including Ozempic (for type 2 diabetes) and Wegovy (for weight management), as well as an oral formulation called Rybelsus (for type 2 diabetes). The injectable forms have a half-life of approximately one week, allowing for sustained therapeutic effects between doses.
Importantly, semaglutide's primary targets are metabolic pathways rather than immune system components. GLP-1 receptors are found in pancreatic beta cells, the gastrointestinal tract, areas of the brain involved in appetite regulation, and to some extent in cardiovascular, renal, and certain immune cells. However, semaglutide is not designed as an immunomodulatory agent. Understanding this mechanism is essential when evaluating concerns about potential immune system effects, as the drug's pharmacological action centers on glucose metabolism and satiety signaling rather than direct immune function modulation. Semaglutide is not indicated for type 1 diabetes or diabetic ketoacidosis.
Current clinical evidence does not support the claim that semaglutide suppresses or lowers immune system function. Large-scale randomized controlled trials, including the SUSTAIN and STEP trial programs involving thousands of participants, have not identified immunosuppression as an adverse effect of semaglutide therapy. The FDA-approved prescribing information for Ozempic, Wegovy, and Rybelsus does not list immune system impairment among the drug's known risks or warnings.
Infection rates observed in clinical trials of semaglutide have been comparable to those seen with placebo or active comparators. Common infections such as upper respiratory tract infections, urinary tract infections, and gastroenteritis occurred at similar frequencies across treatment groups. This pattern suggests that semaglutide does not meaningfully alter susceptibility to routine infections. Post-marketing surveillance has not revealed signals indicating increased infection risk or compromised immune responses.
Some laboratory studies have explored GLP-1 receptor expression on immune cells and potential anti-inflammatory properties of GLP-1 agonists. Preliminary research suggests these medications may have modest anti-inflammatory effects in certain contexts, which differs fundamentally from immunosuppression. These preliminary findings remain of uncertain clinical relevance and do not suggest altered infection susceptibility. Anti-inflammatory activity, if confirmed in humans, could potentially benefit conditions characterized by chronic inflammation, such as cardiovascular disease and metabolic syndrome.
It is important to distinguish between immunosuppression—which impairs the body's defense mechanisms—and the metabolic changes associated with weight loss and improved glycemic control. Patients losing significant weight may experience various physiological adjustments, but these do not constitute immune system suppression. Rare hypersensitivity reactions including anaphylaxis and angioedema have been reported with semaglutide, but these immune-mediated reactions do not indicate immunosuppression.
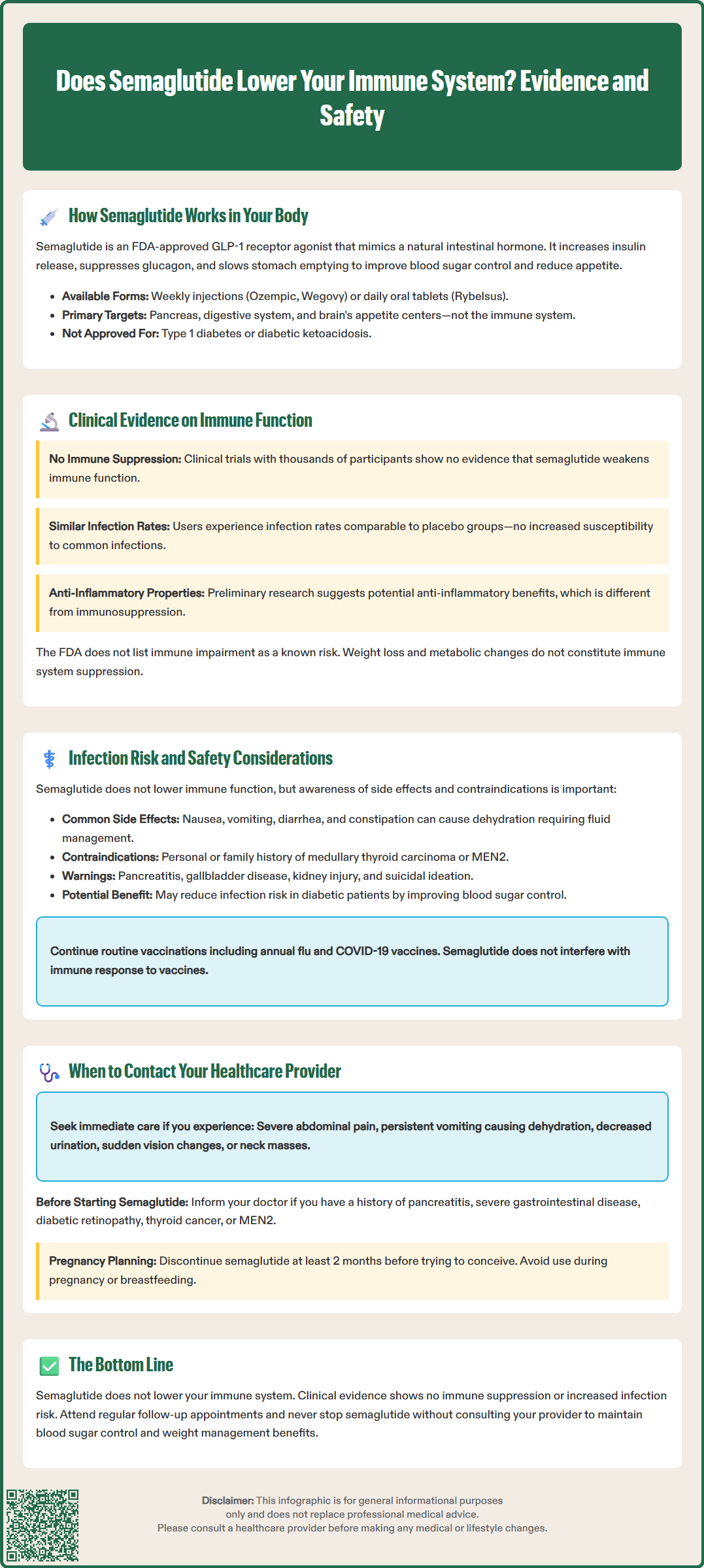
While semaglutide does not lower immune system function, several important safety considerations warrant attention. The most common adverse effects are gastrointestinal, including nausea, vomiting, diarrhea, and constipation. These symptoms typically diminish over time but can occasionally lead to dehydration if severe. Dehydration may indirectly affect overall health and should be managed promptly with adequate fluid intake and, when necessary, medical intervention.
Semaglutide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. It is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Wegovy specifically includes a warning about suicidal behavior and ideation. Other serious adverse effects include pancreatitis, gallbladder disease, acute kidney injury, and diabetic retinopathy complications (particularly with rapid improvement in blood glucose). Hypoglycemia risk increases when semaglutide is used with insulin or sulfonylureas. Caution is advised in patients with severe gastroparesis or significant gastrointestinal disease.
Patients with type 2 diabetes may have baseline factors that influence infection susceptibility independent of semaglutide therapy. Poorly controlled diabetes itself is associated with increased infection risk due to impaired neutrophil function, reduced cellular immunity, and compromised wound healing. Achieving better glycemic control with semaglutide may actually reduce infection risk over time by addressing these underlying metabolic abnormalities. The American Diabetes Association emphasizes that optimal glucose management is a cornerstone of infection prevention in people with diabetes.
Semaglutide is not recommended during pregnancy or breastfeeding, and should be discontinued at least 2 months before a planned pregnancy. Healthcare providers should conduct a thorough medical history before initiating semaglutide, identifying patients with conditions that genuinely affect immune function, such as HIV/AIDS, active cancer treatment, chronic corticosteroid use, or immunosuppressive therapy. Routine vaccinations, including annual influenza and COVID-19 vaccines, remain appropriate and important for patients taking semaglutide.
Patients taking semaglutide should maintain open communication with their healthcare team and seek medical advice for specific symptoms or concerns. Contact your provider if you experience signs of serious adverse effects, including severe or persistent abdominal pain (which may indicate pancreatitis or gallbladder problems), persistent nausea and vomiting leading to inability to maintain hydration, or symptoms of acute kidney injury such as decreased urination, swelling, or unusual fatigue.
Other important reasons to contact your healthcare provider include symptoms of hypoglycemia (especially if taking insulin or sulfonylureas), such as shakiness, dizziness, sweating, confusion, or extreme hunger; sudden vision changes which could indicate retinopathy complications; and any neck mass or persistent hoarseness that could relate to thyroid concerns. While semaglutide does not compromise immune function, patients should report any infections that are unusually severe, prolonged, or recurrent, as such patterns may indicate underlying health issues requiring evaluation.
Patients should also contact their provider before starting semaglutide if they have a history of pancreatitis, severe gastrointestinal disease, diabetic retinopathy, medullary thyroid carcinoma, or MEN2. Those planning pregnancy should discuss discontinuing semaglutide at least 2 months before attempting conception. For patients planning surgery or medical procedures, inform your surgical team about semaglutide use. Current guidance from U.S. medical societies suggests that most patients can continue semaglutide perioperatively, but individual risk assessment and possibly a liquid diet 24 hours before procedures may be recommended.
Routine follow-up appointments are essential for monitoring treatment response, adjusting doses, and screening for complications. The American Diabetes Association Standards of Care recommends regular assessment of glycemic control, weight trends, and medication tolerance in patients receiving GLP-1 receptor agonists. Patients should not discontinue semaglutide without consulting their healthcare provider, as this could lead to loss of glycemic control or weight regain. If you have questions about semaglutide and your overall health, including any concerns about infection risk or immune function, schedule a consultation with your prescribing physician or endocrinologist for personalized guidance based on your complete medical history.
No, clinical trials have not shown increased infection susceptibility with semaglutide. Infection rates in semaglutide trials were comparable to placebo groups, indicating the medication does not meaningfully alter your body's ability to fight routine infections.
Serious side effects include pancreatitis (severe abdominal pain), gallbladder disease, acute kidney injury, thyroid tumors (boxed warning), and diabetic retinopathy complications. Contact your healthcare provider immediately if you experience severe persistent abdominal pain, decreased urination, vision changes, or neck masses.
No, routine vaccinations including annual influenza and COVID-19 vaccines remain appropriate and important for patients taking semaglutide. The medication does not suppress immune function or interfere with vaccine effectiveness.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.