LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist prescribed for type 2 diabetes and chronic weight management. Many patients wonder whether tirzepatide shows up on blood tests during routine medical care. While the medication itself is not detected by standard laboratory panels, understanding what blood work can and cannot reveal about tirzepatide is important for patients and healthcare providers. This article explains how tirzepatide interacts with common blood tests, what metabolic changes may be observed, and essential information to share with your doctor before laboratory work.
Quick Answer: Tirzepatide does not appear on routine blood tests, but specialized research assays can detect it in clinical trial settings.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a prescription medication approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity (marketed as Zepbound). It is the first dual incretin receptor agonist, activating both glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors.
The medication works by targeting two key incretin hormone pathways simultaneously. By activating GIP receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner. The GLP-1 receptor activation contributes to glucose control by stimulating insulin release, suppressing glucagon secretion when blood glucose is elevated, and slowing gastric emptying. This dual action results in improved glycemic control and significant weight reduction.
Tirzepatide is administered as a once-weekly subcutaneous injection, starting at 2.5 mg for 4 weeks (an initiation dose), then typically increasing to 5 mg, with possible further increases to 7.5, 10, 12.5, or 15 mg based on clinical response and tolerability. In clinical trials, tirzepatide demonstrated reductions in hemoglobin A1c of up to 2.5% and weight loss of approximately 15-21% of body weight at higher doses after 72 weeks of treatment, with results varying by dose and patient population.
Common adverse effects include gastrointestinal symptoms such as nausea, diarrhea, vomiting, and constipation, which typically diminish over time. Tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients should be monitored for signs of pancreatitis, gallbladder disease, and hypoglycemia (particularly when used with insulin or sulfonylureas). Tirzepatide is not indicated for type 1 diabetes and should be used with caution in patients with gastroparesis.
Tirzepatide does not appear on routine blood tests ordered in standard clinical practice, including complete blood counts, comprehensive metabolic panels, lipid panels, or hemoglobin A1c measurements. There is no standard clinical laboratory test that specifically detects or measures tirzepatide levels in the bloodstream as part of routine medical care.
However, specialized research assays and immunoassays can detect tirzepatide in blood samples. These tests are typically used only in clinical trial settings, pharmacokinetic studies, or specialized research environments to measure drug concentrations and assess bioavailability. Such testing requires specific antibodies or mass spectrometry techniques and is not available through standard commercial laboratories used in everyday medical practice.
What healthcare providers can observe through blood work are the metabolic effects of tirzepatide rather than the drug itself. Patients taking tirzepatide may show:
Improved glycemic markers: Lower fasting glucose and reduced hemoglobin A1c levels
Potential lipid profile changes: Possible decreases in triglycerides and changes in cholesterol parameters
Liver function parameters: Possible changes in liver enzymes in patients with fatty liver disease
Kidney function monitoring: Serum creatinine and estimated glomerular filtration rate should be tracked, particularly if dehydration occurs
It is important to note that tirzepatide has no known interference with standard laboratory assays and is not included in standard drug screening tests, which typically focus on substances of abuse and controlled medications. Mild elevations in pancreatic enzymes (lipase, amylase) can occur with tirzepatide use without clinical pancreatitis and should be interpreted in the appropriate clinical context. Regular monitoring of metabolic parameters is recommended per American Diabetes Association Standards of Care for patients on diabetes or weight management medications.
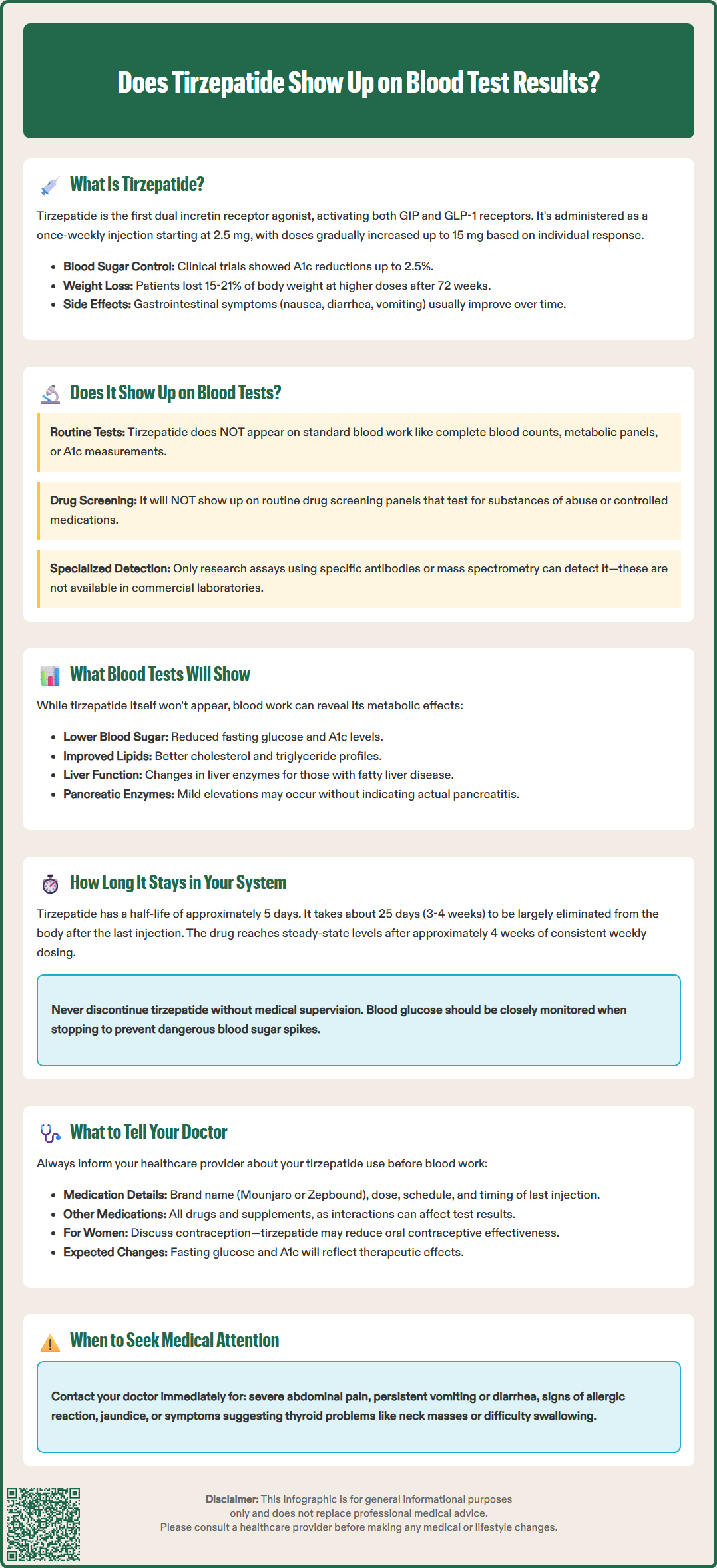
Understanding the pharmacokinetics of tirzepatide helps clarify its duration in the body and implications for blood testing. Tirzepatide has a half-life of approximately 5 days (approximately 120 hours), which is the time required for half of the drug concentration to be eliminated from the bloodstream. This extended half-life is what enables the convenient once-weekly dosing schedule.
Based on standard pharmacokinetic principles, it takes approximately five half-lives for a medication to be essentially eliminated from the body. For tirzepatide, this means the drug would be largely cleared from your system in approximately 25 days (roughly 3-4 weeks) after the last injection. However, measurable concentrations may persist slightly longer, and the metabolic effects of the medication—such as improved blood glucose control—may continue beyond complete drug elimination.
Several factors influence tirzepatide's pharmacokinetics:
Elimination pathway: Tirzepatide is primarily eliminated through proteolytic breakdown in the body, not through renal excretion
Dose and duration of treatment: Higher doses and longer treatment periods result in greater drug accumulation
Body weight: Body weight is a known covariate that can modestly affect drug exposure
Steady-state concentrations: With weekly dosing, tirzepatide reaches steady-state levels after approximately 4 weeks of consistent administration
According to FDA prescribing information, no dose adjustment is required for patients with renal impairment (including end-stage renal disease) or hepatic impairment, as these conditions do not significantly affect tirzepatide clearance.
For patients discontinuing tirzepatide, blood glucose levels should be monitored closely as the medication's glucose-lowering effects diminish. The American Diabetes Association recommends regular monitoring when adjusting or stopping diabetes medications to prevent hyperglycemia. Patients should not abruptly discontinue tirzepatide without medical supervision, particularly if it is being used as part of a comprehensive diabetes management plan.
Full medication disclosure is essential for accurate interpretation of blood test results and safe medical care. Before any blood work, patients should inform their healthcare provider that they are taking tirzepatide, including the dose, frequency, and duration of treatment. While tirzepatide itself does not appear on standard blood tests, this information helps clinicians interpret results in the appropriate clinical context.
Key information to discuss with your doctor includes:
Current tirzepatide dose and schedule: Specify whether you are taking Mounjaro or Zepbound and your current weekly dose
Duration of treatment: How long you have been on the medication and any recent dose adjustments
Other medications: All prescription drugs, over-the-counter medications, and supplements, as drug interactions may affect blood test results
Recent side effects: Gastrointestinal symptoms, changes in appetite, or any concerning symptoms
Timing of last injection: When you administered your most recent dose relative to the blood draw
Contraception status: Women of childbearing potential should discuss contraception, as tirzepatide may reduce oral contraceptive effectiveness (backup contraception is recommended for 4 weeks after initiation and each dose increase)
Certain blood tests require special consideration in patients taking tirzepatide. Fasting blood glucose and hemoglobin A1c tests will reflect the medication's therapeutic effects. Lipase and amylase levels may be monitored if there is concern for pancreatitis. Kidney function tests should be reviewed regularly, particularly if dehydration occurs.
Patients should never discontinue tirzepatide before blood work unless specifically instructed by their physician. Stopping the medication can lead to rapid deterioration in glycemic control and may complicate the interpretation of test results.
Importantly, patients should seek immediate medical attention for warning signs such as:
Severe, persistent abdominal pain (possible pancreatitis)
Right upper quadrant pain, fever, or jaundice (possible gallbladder disease)
Severe, persistent vomiting or diarrhea leading to dehydration
Signs of allergic reaction including rash, swelling, or difficulty breathing
Unusual neck mass, difficulty swallowing, hoarseness, or shortness of breath (thyroid concerns)
Maintaining open communication ensures accurate diagnosis, appropriate monitoring, and optimal therapeutic outcomes while taking this medication.
No, tirzepatide is not included in standard drug screening tests, which typically focus on substances of abuse and controlled medications. It does not interfere with routine laboratory assays.
Tirzepatide has a half-life of approximately 5 days and is largely eliminated from the body in 3-4 weeks after the last injection. Specialized research assays could potentially detect it during this period, though such testing is not performed in routine clinical practice.
No, patients should never discontinue tirzepatide before blood work unless specifically instructed by their physician. Stopping the medication can lead to rapid deterioration in glycemic control and may complicate interpretation of test results.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.