LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 receptor agonists, including semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound), are increasingly prescribed for type 2 diabetes and weight management. Many patients and clinicians wonder: does GLP-1 affect liver enzymes? Evidence shows these medications typically improve liver enzyme levels rather than harm them, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). Clinical trials demonstrate reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST)—key markers of liver health—often correlating with decreased hepatic fat accumulation. Understanding how GLP-1 therapy influences liver function helps guide appropriate patient selection and monitoring strategies.
Quick Answer: GLP-1 receptor agonists typically improve liver enzyme levels, reducing elevated ALT and AST in patients with metabolic liver disease rather than causing harm.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications that mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestinal tract. These medications work by binding to GLP-1 receptors located throughout the body, including the pancreas, brain, and gastrointestinal tract, with indirect effects on the liver.
The primary mechanism of action involves enhancing glucose-dependent insulin secretion from pancreatic beta cells while simultaneously suppressing inappropriate glucagon release. This dual effect helps regulate blood glucose levels without causing significant hypoglycemia, as the insulin response diminishes when blood sugar normalizes. GLP-1 receptor agonists also slow gastric emptying, which moderates the postprandial glucose spike and promotes satiety through central nervous system pathways.
In the liver, GLP-1 receptor agonists primarily exert indirect effects through improved insulin sensitivity, reduced glucagon secretion, and weight loss. These medications help decrease hepatic glucose production and reduce hepatic steatosis (fat accumulation in liver cells). While some preclinical studies suggest direct hepatic effects, the clinical benefits on liver health appear largely mediated through these indirect metabolic improvements.
Currently approved GLP-1 receptor agonists in the United States include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Bydureon BCise). Tirzepatide (Mounjaro, Zepbound) is a dual GLP-1/GIP receptor agonist with similar effects. Each agent differs in molecular structure, half-life, and dosing frequency, but all share the core mechanism of GLP-1 receptor activation that influences multiple organ systems, including indirect effects on hepatic function. Generally, no dose adjustment is required for mild to moderate hepatic impairment with these medications.
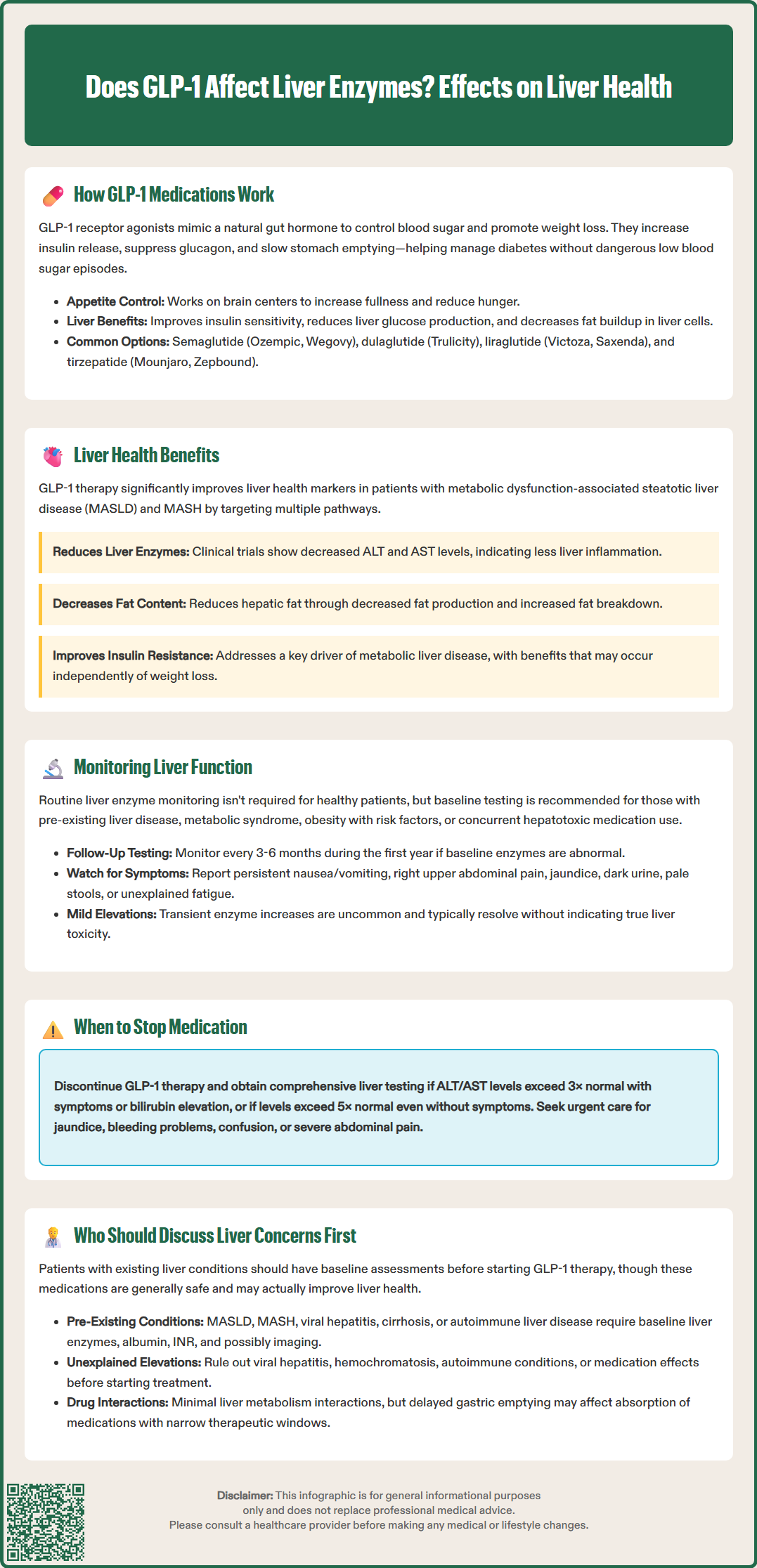
Emerging evidence demonstrates that GLP-1 receptor agonists may provide significant benefits for liver health, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as non-alcoholic fatty liver disease or NAFLD) and its inflammatory subtype, metabolic dysfunction-associated steatohepatitis (MASH, formerly NASH). Clinical trials have shown improvements in liver enzyme levels, hepatic fat content, and markers of liver inflammation in patients treated with these medications.
Multiple studies indicate that GLP-1 therapy can reduce elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels—key biomarkers of hepatocellular injury. A meta-analysis of randomized controlled trials found that GLP-1 receptor agonists significantly decreased ALT levels compared to placebo or other glucose-lowering agents. These reductions often correlate with decreased hepatic steatosis as measured by imaging studies or liver biopsy. The magnitude of enzyme improvement typically parallels the degree of weight loss achieved, though some hepatic benefits may occur independent of weight reduction.
The mechanisms underlying these hepatoprotective effects include reduced hepatic lipogenesis (fat production), enhanced fatty acid oxidation, and decreased inflammatory cytokine production. GLP-1 receptor agonists improve insulin resistance—a central driver of metabolic liver disease. Preclinical studies suggest potential anti-inflammatory and anti-fibrotic actions, though human data on fibrosis improvement remain limited.
For patients with MASH, clinical trials have demonstrated histological improvements in liver inflammation and ballooning degeneration. However, effects on advanced fibrosis remain under investigation, with phase 2 trials of semaglutide showing MASH resolution without confirmed fibrosis improvement. The American Association for the Study of Liver Diseases (AASLD) acknowledges the potential role of GLP-1 receptor agonists in managing MASLD, particularly in patients with concurrent type 2 diabetes or obesity. It is important to note that GLP-1 receptor agonists are not FDA-approved specifically for the treatment of MASLD or MASH, though they may be used off-label in appropriate patients.
Routine monitoring of liver enzymes is not universally required for all patients initiating GLP-1 receptor agonist therapy, as these medications are not typically associated with drug-induced liver injury. However, baseline and periodic assessment may be appropriate in specific clinical contexts, particularly for patients with known or suspected liver disease.
The FDA-approved prescribing information for GLP-1 receptor agonists does not mandate routine liver function testing in otherwise healthy individuals. However, clinical judgment should guide monitoring decisions based on individual patient characteristics. Baseline liver enzyme assessment is reasonable for patients with:
Pre-existing liver disease or elevated baseline transaminases
Metabolic syndrome or clinical features suggesting MASLD
Concurrent use of other potentially hepatotoxic medications
Obesity (BMI ≥30 kg/m²) with additional metabolic risk factors
History of excessive alcohol consumption
For patients with abnormal baseline liver enzymes, periodic monitoring every 3-6 months during the first year of therapy allows clinicians to assess treatment response and detect any unexpected changes. Significant improvements in ALT and AST levels may indicate beneficial effects on underlying hepatic steatosis, while stable or worsening enzymes warrant further investigation to identify alternative causes of liver dysfunction.
It is important to note that mild, transient elevations in liver enzymes during GLP-1 therapy initiation are uncommon but may occur. These typically resolve without intervention and do not necessarily indicate hepatotoxicity. However, patients should be advised to report symptoms suggestive of liver injury, including:
Persistent nausea or vomiting unrelated to expected GI side effects
Right upper quadrant abdominal pain (which may also indicate gallbladder disease, a known risk with GLP-1 therapy)
Jaundice (yellowing of skin or eyes)
Dark urine or pale stools
Unexplained fatigue or malaise
Clinicians should maintain a low threshold for investigating these symptoms with comprehensive liver function tests, including ALT, AST, alkaline phosphatase, bilirubin, albumin, and INR/prothrombin time. Consider holding medication and obtaining prompt evaluation if ALT/AST exceed 3× upper limit of normal with symptoms or bilirubin elevation, or if levels exceed 5× upper limit of normal even without symptoms.
Certain patient populations warrant thorough discussion of liver-related considerations before initiating GLP-1 receptor agonist therapy. While these medications are generally safe and may even benefit liver health, individualized assessment ensures appropriate patient selection and monitoring strategies.
Patients with established liver disease should engage in detailed conversations with their healthcare providers. This includes individuals with:
Diagnosed MASLD or MASH, where GLP-1 therapy may offer therapeutic benefits but requires monitoring
Chronic viral hepatitis (hepatitis B or C), particularly if transaminases are elevated
Autoimmune hepatitis or other inflammatory liver conditions
Cirrhosis or advanced fibrosis, where specialist consultation may be appropriate despite generally not requiring dose adjustment
History of drug-induced liver injury from other agents
For these patients, baseline comprehensive liver assessment—including liver enzymes, synthetic function tests (albumin, INR), and potentially imaging or non-invasive fibrosis markers (such as FIB-4 or ELF)—helps establish a reference point for monitoring treatment effects. Consultation with a hepatologist is appropriate for patients with advanced liver disease, decompensation signs, or uncertain diagnoses.
Patients taking multiple medications should discuss potential interactions, though GLP-1 receptor agonists have minimal hepatic metabolism interactions. The primary concern is delayed gastric emptying affecting absorption of some oral drugs, particularly those with narrow therapeutic windows. For example, tirzepatide carries a specific warning regarding potential reduced effectiveness of oral contraceptives. Those consuming alcohol regularly should receive counseling about the combined metabolic effects on the liver and the importance of moderation or cessation.
Individuals with unexplained elevated liver enzymes discovered during routine screening should undergo appropriate diagnostic evaluation before starting GLP-1 therapy. While these medications may improve enzyme levels in patients with metabolic liver disease, alternative causes—including viral hepatitis, hemochromatosis, autoimmune conditions, or medication effects—must be excluded.
Patients should understand that GLP-1 receptor agonists are not contraindicated in liver disease and may actually provide hepatic benefits. However, informed decision-making requires discussion of monitoring plans, expected outcomes, and circumstances that would prompt further evaluation or referral to specialty care. Urgent medical attention is warranted for jaundice, significant coagulopathy, confusion, or severe abdominal pain during treatment.
GLP-1 receptor agonists are not typically associated with drug-induced liver injury and generally do not cause liver damage. In fact, clinical evidence shows these medications often improve liver health markers, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD).
Routine liver enzyme monitoring is not required for otherwise healthy patients taking GLP-1 medications. However, baseline and periodic testing may be appropriate for those with pre-existing liver disease, metabolic syndrome, obesity with metabolic risk factors, or unexplained elevated liver enzymes.
GLP-1 receptor agonists improve liver enzymes primarily through indirect mechanisms including enhanced insulin sensitivity, reduced hepatic fat accumulation, weight loss, and decreased inflammatory cytokine production. These effects help reduce hepatic steatosis and liver inflammation, leading to lower ALT and AST levels.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.