LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients wonder whether semaglutide can specifically target belly fat. Semaglutide, a GLP-1 receptor agonist approved by the FDA for chronic weight management, does reduce abdominal fat—but not through spot reduction. Instead, it facilitates overall weight loss by suppressing appetite and reducing caloric intake, which leads to proportional decreases in total body fat, including both visceral and subcutaneous abdominal adiposity. Clinical trials demonstrate significant reductions in waist circumference alongside improvements in metabolic health. Understanding how semaglutide works and what realistic outcomes to expect is essential for patients considering this medication as part of a comprehensive weight management strategy.
Quick Answer: Semaglutide reduces belly fat as part of overall body fat loss but does not specifically target abdominal areas.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. Wegovy (semaglutide 2.4 mg) is also approved for weight management in adolescents aged 12 years and older with obesity (BMI ≥95th percentile for age and sex). Originally developed for type 2 diabetes management, semaglutide mimics the action of endogenous GLP-1, a hormone released by the intestine in response to food intake.
The medication works through multiple complementary mechanisms to promote weight loss. Semaglutide acts on GLP-1 receptors in the brain, particularly in areas that regulate appetite and food intake, leading to reduced hunger and increased feelings of fullness. It slows gastric emptying (an effect that may attenuate with chronic use), which prolongs satiety after meals and reduces overall caloric intake. Additionally, semaglutide may influence food preference and reward pathways in the brain, potentially decreasing cravings for high-calorie foods.
When administered as a once-weekly subcutaneous injection, semaglutide has a half-life of approximately one week, reaching steady-state concentrations after 4-5 weeks. This provides consistent appetite suppression throughout the week. The medication is available in two formulations: Ozempic (approved for type 2 diabetes at doses up to 2.0 mg weekly, not FDA-approved for weight management) and Wegovy (approved specifically for weight management at doses up to 2.4 mg weekly, with a recommended dose escalation schedule starting at 0.25 mg and increasing gradually to minimize side effects).
It is important to understand that semaglutide does not directly "burn" fat or target specific body areas. Rather, it facilitates overall weight loss by helping patients consume fewer calories, which leads to reduction in total body fat, including visceral and subcutaneous abdominal fat.
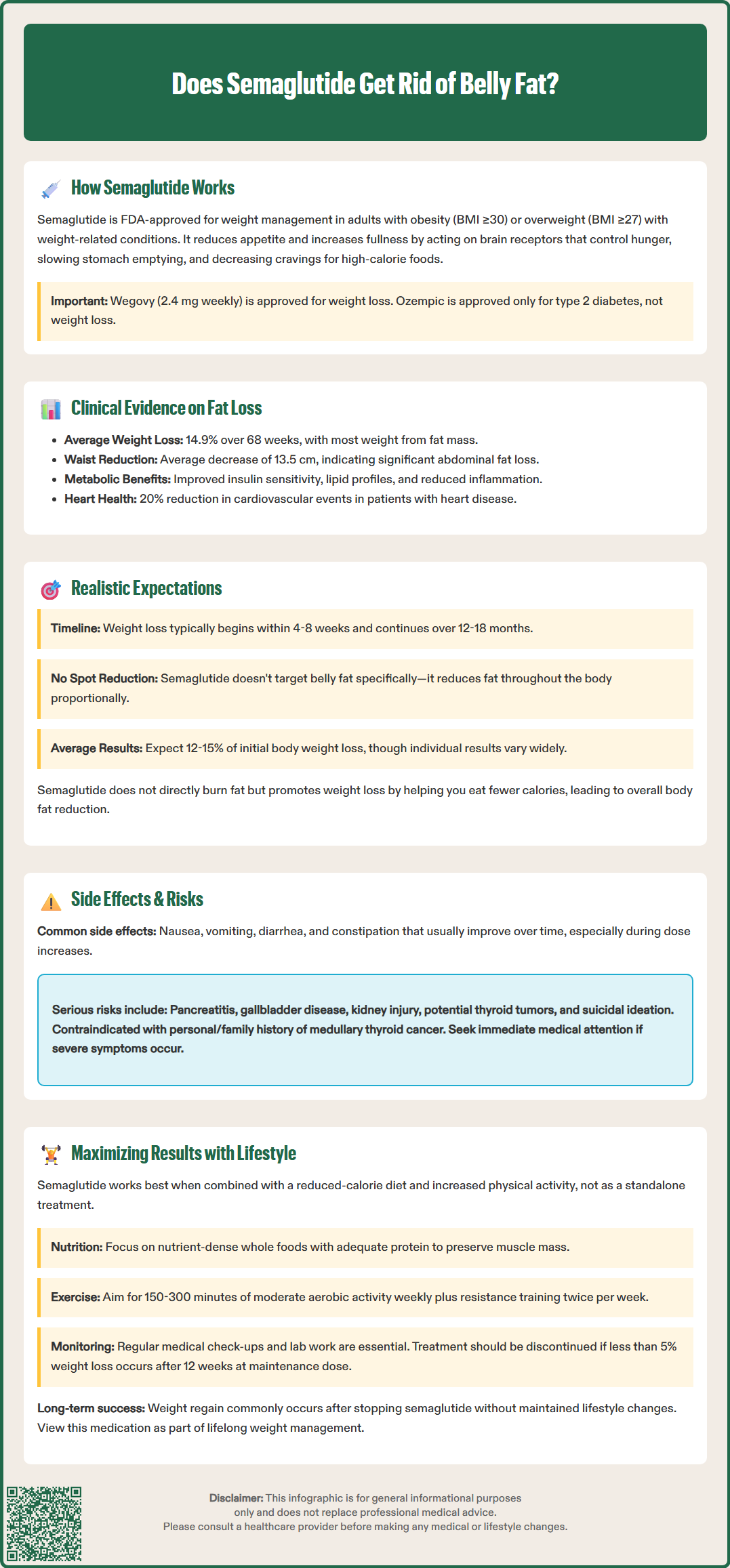
Robust clinical trial data demonstrate that semaglutide produces significant reductions in total body weight and body fat, including abdominal adiposity. The STEP (Semaglutide Treatment Effect in People with obesity) clinical trial program provides the most comprehensive evidence for semaglutide's effects on body composition.
In the STEP 1 trial, adults with obesity who received semaglutide 2.4 mg weekly achieved a mean weight loss of 14.9% of initial body weight over 68 weeks, compared to 2.4% with placebo. Body composition analyses using dual-energy X-ray absorptiometry (DEXA) scans revealed that a majority of the weight lost was fat mass. Importantly, waist circumference—a proxy measure for abdominal fat—decreased by an average of 13.5 cm in the semaglutide group versus 4.1 cm in the placebo group.
Subsequent studies have confirmed reductions in visceral adipose tissue (VAT), the metabolically active fat surrounding internal organs that contributes to cardiometabolic risk. Imaging studies within the STEP program demonstrated significant decreases in both visceral and subcutaneous abdominal fat. These reductions in abdominal adiposity correlate with improvements in metabolic parameters, including insulin sensitivity, lipid profiles, and inflammatory markers.
The SELECT cardiovascular outcomes trial further demonstrated that semaglutide-induced weight loss translates to meaningful clinical benefits, including a 20% reduction in major adverse cardiovascular events in patients with established cardiovascular disease. This led to an FDA label update for Wegovy recognizing its cardiovascular risk reduction benefit. While semaglutide does reduce belly fat as part of overall fat loss, there is no evidence that it preferentially targets abdominal fat over fat in other body regions. The distribution of fat loss generally follows the body's natural pattern of fat mobilization during caloric deficit.
Patients considering semaglutide for weight management should have realistic expectations about the timeline, magnitude, and pattern of fat loss. Weight reduction with semaglutide is gradual and progressive, not immediate. Most patients begin to notice weight loss within the first 4-8 weeks of treatment, with continued loss over 12-18 months as the dose is titrated upward.
Clinical trials indicate that the average weight loss with semaglutide 2.4 mg weekly ranges from 12-15% of initial body weight over 68 weeks. However, individual responses vary considerably. Approximately one-third of patients in the STEP 1 trial achieved weight loss exceeding 20%, while some patients experience more modest results. Factors influencing response include baseline weight, adherence to lifestyle modifications, genetic factors, and concurrent medications.
Regarding belly fat specifically, patients should understand that spot reduction is not physiologically possible. As overall body fat decreases, abdominal fat will reduce proportionally, but the body determines where fat is mobilized based on genetics, hormones, and individual physiology. Some patients may notice changes in facial appearance or extremities before significant abdominal changes become apparent. Waist circumference typically decreases with treatment, with the magnitude varying among individuals.
Common adverse effects include gastrointestinal symptoms—nausea, vomiting, diarrhea, and constipation—which are usually mild to moderate and diminish over time. These effects are most pronounced during dose escalation. Serious adverse effects include pancreatitis, gallbladder disease, acute kidney injury, and increased heart rate. Semaglutide carries a boxed warning about thyroid C-cell tumors observed in rodent studies (though human relevance remains uncertain) and is contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Additional warnings include hypoglycemia risk when used with insulin or sulfonylureas, diabetic retinopathy complications in patients with diabetes, and suicidal ideation. Semaglutide should not be used during pregnancy.
Patients should seek immediate medical attention for severe abdominal pain, persistent vomiting, visual changes, or suicidal thoughts. Weight regain commonly occurs if semaglutide is discontinued without sustained lifestyle changes, as the medication does not permanently alter metabolism or appetite regulation.
Semaglutide is most effective when integrated into a comprehensive weight management program that includes dietary modification and increased physical activity. The FDA approval for Wegovy specifically indicates use "as an adjunct to a reduced-calorie diet and increased physical activity." Clinical trials demonstrating semaglutide's efficacy all included lifestyle intervention components, and real-world outcomes are optimized when patients actively engage in behavioral changes.
Dietary approaches should focus on nutrient-dense, whole foods with adequate protein intake to help preserve lean muscle mass during weight loss. Working with a registered dietitian nutritionist (RDN) is recommended to develop individualized, sustainable eating patterns that align with the appetite changes induced by semaglutide. Small, frequent meals may help manage gastrointestinal side effects. Protein needs vary by individual, and an RDN can help determine appropriate targets based on weight, activity level, and health status.
Physical activity is essential for patients using semaglutide. The US Department of Health and Human Services Physical Activity Guidelines recommend at least 150-300 minutes of moderate-intensity aerobic activity weekly, plus muscle-strengthening activities targeting all major muscle groups at least twice weekly. Resistance training is especially important to minimize loss of muscle mass and maintain metabolic rate during weight loss. Exercise not only enhances fat loss but also improves body composition, cardiovascular fitness, and metabolic health independent of weight changes.
Patients should be monitored regularly by healthcare providers during semaglutide treatment. Initial assessments should include comprehensive metabolic panels, lipid profiles, pregnancy testing when applicable, and screening for contraindications. Follow-up visits should track weight loss progress, assess for adverse effects (including mood changes), evaluate adherence to lifestyle modifications, and adjust treatment as needed. Per US guidelines, clinicians should consider discontinuation if a patient has not lost at least 5% of initial body weight after 12 weeks on the maintenance dose. Semaglutide should not be used concurrently with other semaglutide-containing products or other GLP-1 receptor agonists.
Referral to endocrinology or obesity medicine specialists is appropriate for patients with complex medical histories or suboptimal response to treatment. Long-term success requires viewing semaglutide as one component of lifelong weight management rather than a temporary solution.
Most patients begin noticing weight loss within 4-8 weeks of starting semaglutide, with continued fat reduction over 12-18 months as the dose is gradually increased. Abdominal fat decreases proportionally with overall body fat loss, though the timing and distribution vary by individual genetics and physiology.
Semaglutide does not preferentially target visceral abdominal fat, but clinical trials demonstrate significant reductions in both visceral and subcutaneous abdominal adiposity as part of overall fat loss. Imaging studies show decreased waist circumference and improved metabolic markers associated with reduced visceral fat.
Weight regain, including abdominal fat, commonly occurs after discontinuing semaglutide without sustained lifestyle changes, as the medication does not permanently alter metabolism or appetite regulation. Long-term success requires ongoing dietary modifications and physical activity even after stopping treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.