LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
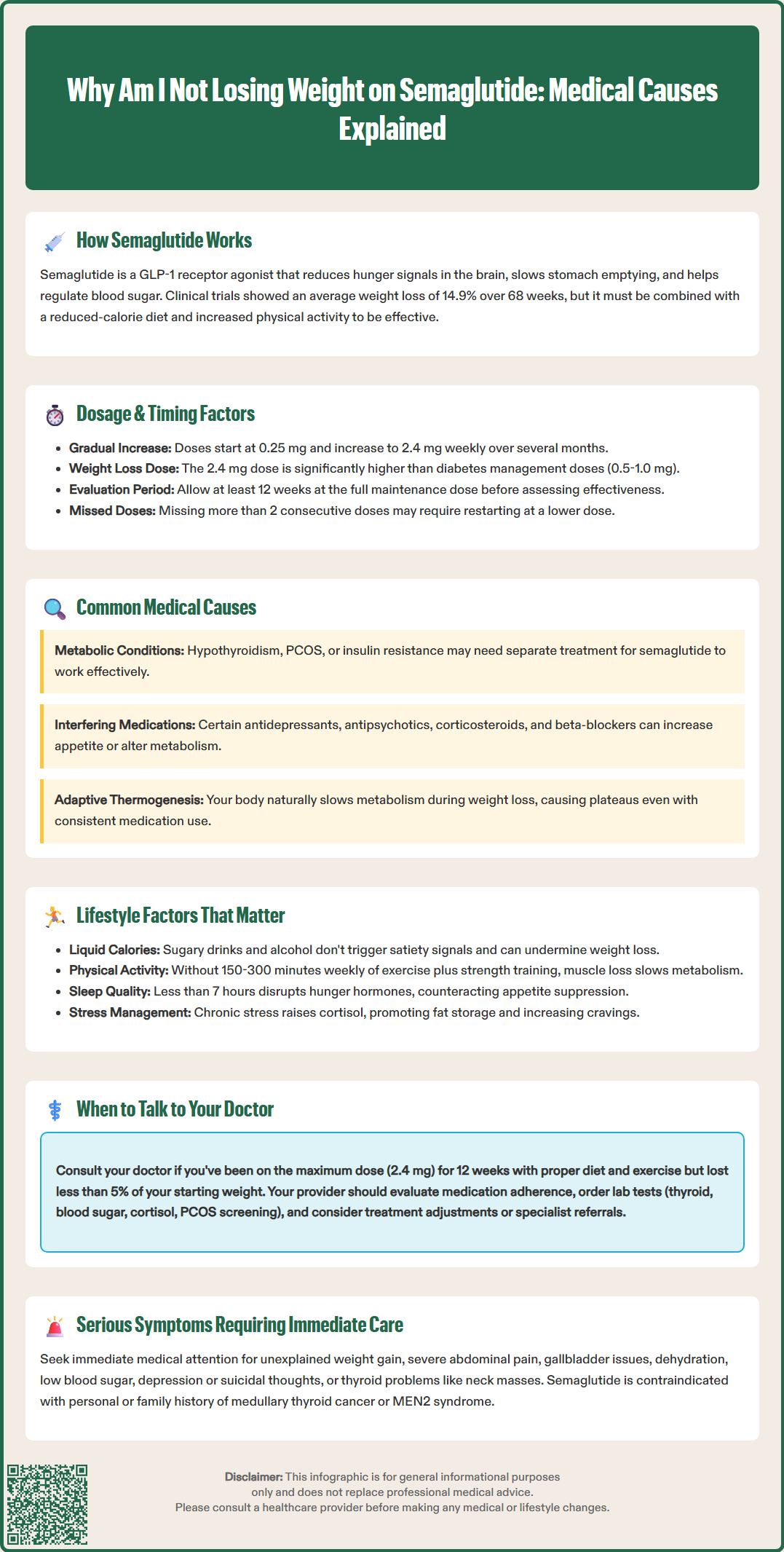
Many patients starting semaglutide for weight management expect consistent results, yet some experience slower progress or weight loss plateaus. Understanding why you're not losing weight on semaglutide involves examining multiple factors, from medication dosing and timing to lifestyle habits and underlying medical conditions. This GLP-1 receptor agonist works through complex mechanisms affecting appetite, digestion, and metabolism, but individual responses vary significantly. While clinical trials demonstrate substantial average weight loss, achieving optimal results requires proper dosing, adequate treatment duration, and comprehensive lifestyle modifications. This article explores common barriers to weight loss on semaglutide and provides evidence-based guidance on maximizing treatment effectiveness.
Quick Answer: Weight loss may not occur on semaglutide due to insufficient dosing, inadequate treatment duration, suboptimal lifestyle modifications, metabolic adaptation, or interfering medications.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics a naturally occurring hormone in the body. While the exact mechanism for weight management is not fully understood, this medication works through multiple pathways to promote weight loss when combined with lifestyle modifications.
Semaglutide affects appetite centers in the brain, specifically the hypothalamus, reducing hunger signals and food cravings. It also delays gastric emptying (though this effect may diminish over time), creating a prolonged sensation of fullness. Additionally, it enhances insulin secretion in response to meals while suppressing glucagon release, which helps regulate blood sugar levels and may indirectly support weight management.
Clinical trials have demonstrated that semaglutide can lead to significant weight loss when used at higher doses specifically approved for obesity management. In the STEP 1 trial, participants using semaglutide 2.4 mg weekly (marketed as Wegovy) lost an average of 14.9% of their body weight over 68 weeks. However, individual responses vary considerably, with some patients experiencing more modest results.
It's important to understand that semaglutide is not a standalone solution. The FDA-approved labeling emphasizes that semaglutide should be used as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbid condition.
Several factors can explain why some individuals don't achieve expected weight loss results with semaglutide therapy. Understanding these reasons can help identify potential barriers and guide appropriate interventions.
Insufficient time on therapy: Weight loss with semaglutide typically occurs gradually. Many patients expect rapid results but may not see significant changes in the first 4-8 weeks. The medication requires time to reach therapeutic levels, and the body needs time to respond. Most clinical trials measured outcomes at 68 weeks, highlighting that this is a long-term intervention.
Suboptimal dosing: Patients may be on a dose intended for diabetes management (0.5-1.0 mg weekly) rather than the higher dose approved for weight loss (2.4 mg weekly). The lower doses, while effective for glycemic control, may not provide sufficient appetite suppression for substantial weight loss. Additionally, some patients may not have completed the full dose escalation schedule, remaining at intermediate doses that are less effective for weight management.
Metabolic adaptation: The body naturally adapts to weight loss by reducing metabolic rate, a phenomenon sometimes called "adaptive thermogenesis." This biological response is expected and can slow or plateau weight loss even when medication and lifestyle factors remain consistent. Some individuals may also have underlying metabolic conditions such as hypothyroidism, polycystic ovary syndrome (PCOS), or insulin resistance that weren't adequately addressed before starting semaglutide.
Medication interactions: Certain medications can interfere with weight loss efforts, including some antidepressants (particularly paroxetine, mirtazapine), antipsychotics (especially olanzapine, quetiapine), mood stabilizers (valproate), antiepileptics (gabapentin, pregabalin), corticosteroids, beta-blockers, and diabetes medications (insulin, sulfonylureas). These medications may counteract semaglutide's weight loss effects through various mechanisms, including increased appetite or altered metabolism.
The dosing strategy for semaglutide significantly influences weight loss outcomes. The medication follows a specific titration schedule designed to minimize gastrointestinal side effects while gradually increasing therapeutic effect.
For weight management, semaglutide typically starts at 0.25 mg weekly for four weeks, then increases to 0.5 mg for four weeks, followed by monthly increases to 1.0 mg, 1.7 mg, and finally the target maintenance dose of 2.4 mg weekly. Some patients and providers may hesitate to advance to higher doses due to side effects, but remaining at lower doses often results in suboptimal weight loss. Clinical data clearly demonstrates a dose-response relationship, with the 2.4 mg dose producing significantly greater weight loss than lower doses.
Timing considerations also matter. Semaglutide can be administered at any time of day, with or without meals, but consistency is important. Taking the medication on the same day each week helps maintain steady drug levels. Some patients anecdotally report better tolerance when taking their injection in the evening, though there is no evidence that timing affects the medication's efficacy.
Missed doses can impact effectiveness. For Wegovy (semaglutide 2.4 mg), if a dose is missed and the next scheduled dose is more than 2 days away, take the missed dose as soon as possible. If the next scheduled dose is less than 2 days away, skip the missed dose and resume at the next scheduled dose. If more than 2 consecutive doses are missed, resume at a lower dose or contact your healthcare provider, as re-titration may be needed to minimize gastrointestinal side effects.
Patients who have been on lower doses for diabetes management and transition to weight loss therapy need adequate time at the higher dose before evaluating effectiveness. A minimum of 12 weeks at the maintenance dose of 2.4 mg is generally recommended before determining whether the medication is working optimally for weight loss.
Importantly, semaglutide should not be used with other GLP-1 receptor agonists or with other semaglutide-containing products.
While semaglutide provides pharmacological support for weight loss, lifestyle factors remain critical determinants of success. The medication enhances the effectiveness of behavioral changes but cannot fully compensate for their absence.
Dietary patterns: Despite reduced appetite, some patients may continue consuming calorie-dense foods or beverages that undermine weight loss efforts. Liquid calories from sugary drinks, alcohol, or high-calorie coffee beverages are particularly problematic because they don't trigger the same satiety signals as solid foods. Additionally, even with smaller portions, choosing foods high in refined carbohydrates and unhealthy fats can prevent a sufficient caloric deficit. The American Diabetes Association and USDA Dietary Guidelines recommend focusing on nutrient-dense, high-fiber foods including vegetables, lean proteins, and whole grains to maximize weight loss while on GLP-1 therapy.
Physical activity levels: Semaglutide reduces appetite and caloric intake, but without adequate physical activity, patients may lose both fat and muscle mass. Preserving lean muscle is essential for maintaining metabolic rate. According to the U.S. Department of Health and Human Services Physical Activity Guidelines, adults should aim for 150-300 minutes of moderate-intensity aerobic activity weekly, plus muscle-strengthening activities on 2 or more days per week. For weight loss maintenance, 200-300 minutes weekly may be more effective.
Sleep and stress: Inadequate sleep (less than 7 hours nightly) disrupts hormones that regulate hunger and satiety, including leptin and ghrelin, potentially counteracting semaglutide's effects. Chronic stress elevates cortisol levels, which can promote fat storage, particularly visceral fat, and increase cravings for high-calorie comfort foods.
Alcohol consumption: Alcohol provides empty calories (7 calories per gram) and can impair judgment around food choices. It may also increase appetite and lead to poor food decisions. Patients serious about weight loss should minimize or eliminate alcohol while on semaglutide therapy.
Knowing when to seek medical guidance about inadequate weight loss on semaglutide is important for optimizing treatment outcomes and identifying potential underlying issues.
Timeline considerations: If you've been at the maximum dose (2.4 mg weekly) for approximately 12 weeks with adherence to dietary and activity recommendations but have lost less than 5% of your starting body weight, this warrants discussion with your healthcare provider. This threshold is clinically significant because weight loss of less than 5% is generally considered a non-response to obesity pharmacotherapy.
Your doctor should evaluate several factors during this consultation. First, they'll review your actual dosing history, adherence patterns, and any missed doses. They'll assess your dietary intake, physical activity levels, and other lifestyle factors that may be limiting results. A thorough medication review is essential to identify any drugs that might interfere with weight loss.
Diagnostic evaluation: Your provider may recommend laboratory testing to rule out underlying conditions affecting weight loss. This typically includes thyroid function tests (TSH, free T4), fasting glucose and hemoglobin A1c, lipid panel, and potentially cortisol levels if Cushing's syndrome is suspected. For women, evaluation for PCOS may be appropriate if other symptoms are present.
Treatment adjustments: Based on this evaluation, your doctor might consider several options: ensuring you're at the optimal dose, addressing any identified medical conditions, adjusting or changing medications that interfere with weight loss, or referring you to specialists such as an endocrinologist, registered dietitian, or obesity medicine specialist.
Red flags requiring immediate attention include:
Unexplained weight gain while on semaglutide
Severe or persistent gastrointestinal symptoms
Signs of pancreatitis (severe abdominal pain radiating to the back)
Symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice)
Signs of dehydration or kidney problems (decreased urination, dizziness)
Hypoglycemia symptoms if taking insulin or sulfonylureas
Depression or suicidal thoughts
Symptoms of thyroid problems (neck mass, difficulty swallowing, persistent hoarseness)
Pregnancy or planning pregnancy (semaglutide should be discontinued at least 2 months before a planned pregnancy)
These situations require prompt medical evaluation rather than waiting for a routine follow-up appointment. Patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2) should not use semaglutide, as this is a contraindication.
Weight loss with semaglutide typically occurs gradually over several months. Most patients should allow at least 12 weeks at the maintenance dose of 2.4 mg weekly before evaluating effectiveness, as clinical trials measured outcomes at 68 weeks.
The FDA-approved dose for weight management is 2.4 mg weekly (Wegovy), which is higher than the 0.5-1.0 mg doses used for diabetes management. Clinical data shows a clear dose-response relationship, with higher doses producing significantly greater weight loss.
Yes, certain medications can interfere with weight loss including some antidepressants (paroxetine, mirtazapine), antipsychotics (olanzapine, quetiapine), corticosteroids, beta-blockers, and diabetes medications like insulin or sulfonylureas. Discuss all medications with your healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.