LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide give you dry mouth? This question concerns many patients prescribed this GLP-1 receptor agonist for type 2 diabetes or weight management. While dry mouth is not listed as a common side effect in FDA prescribing information for Ozempic, Wegovy, or Rybelsus, some patients report experiencing oral dryness during treatment. Understanding whether this symptom stems directly from semaglutide's mechanism, indirect factors like reduced fluid intake, or concurrent medications helps patients and clinicians address concerns appropriately and maintain treatment adherence.
Quick Answer: Dry mouth is not listed as a common side effect in FDA prescribing information for semaglutide, though some patients report experiencing it during treatment.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist with FDA-approved indications that vary by brand name: Ozempic and Rybelsus are approved for type 2 diabetes mellitus, while Wegovy is approved for chronic weight management. Semaglutide works by mimicking the action of the naturally occurring hormone GLP-1. This mechanism enhances glucose-dependent insulin secretion, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying, which collectively improves glycemic control and promotes weight loss.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, reflecting its mechanism of action on the digestive system. According to the FDA prescribing information, these include nausea, vomiting, diarrhea, abdominal pain, and constipation. Nausea is particularly prevalent, affecting approximately 15-20% of patients taking Ozempic and up to 44% of patients taking Wegovy during clinical trials. These gastrointestinal effects are generally dose-dependent and can be minimized through gradual dose escalation.
Other documented side effects include injection site reactions (for subcutaneous formulations), fatigue, and headache. More serious but less common adverse effects include pancreatitis, gallbladder disease, and acute kidney injury associated with severe gastrointestinal adverse effects and dehydration. The FDA prescribing information includes a boxed warning regarding the potential risk of thyroid C-cell tumors (observed in rodent studies, though human relevance remains uncertain) and a contraindication for patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Understanding the full spectrum of potential side effects helps patients and clinicians distinguish between expected medication responses and symptoms requiring further evaluation.
Dry mouth, medically termed xerostomia, is not listed as a common or characteristic side effect in the official FDA prescribing information for semaglutide products. The pivotal clinical trials that led to FDA approval—including the SUSTAIN trials for diabetes management and the STEP trials for weight management—did not identify dry mouth as a statistically significant adverse event occurring at notably higher rates in semaglutide-treated patients compared to placebo groups. This distinguishes semaglutide from some medications that may contribute to dry mouth, such as SGLT2 inhibitors (which can cause dehydration through increased urination) or anticholinergic medications (which directly reduce salivary flow).
However, anecdotal reports from patients and post-marketing surveillance data in the FDA Adverse Event Reporting System (FAERS) suggest that some individuals taking semaglutide do experience dry mouth symptoms. These reports, while not constituting official recognition of a causal relationship, warrant acknowledgment in clinical practice. The absence of dry mouth from formal adverse effect profiles does not definitively exclude the possibility that some patients may experience this symptom, as individual responses to medications can vary considerably based on genetic factors, concurrent medications, and underlying health conditions.
It is important to distinguish between a direct pharmacological effect and secondary causes of dry mouth that may coincide with semaglutide treatment. The medication's effects on appetite, fluid intake patterns, and metabolic changes could indirectly contribute to oral dryness in susceptible individuals. Additionally, patients taking semaglutide often have comorbid conditions or take multiple medications that may independently cause xerostomia. Therefore, while there is no established direct link between semaglutide and dry mouth, clinicians should remain attentive to patient-reported symptoms and investigate potential contributing factors comprehensively.
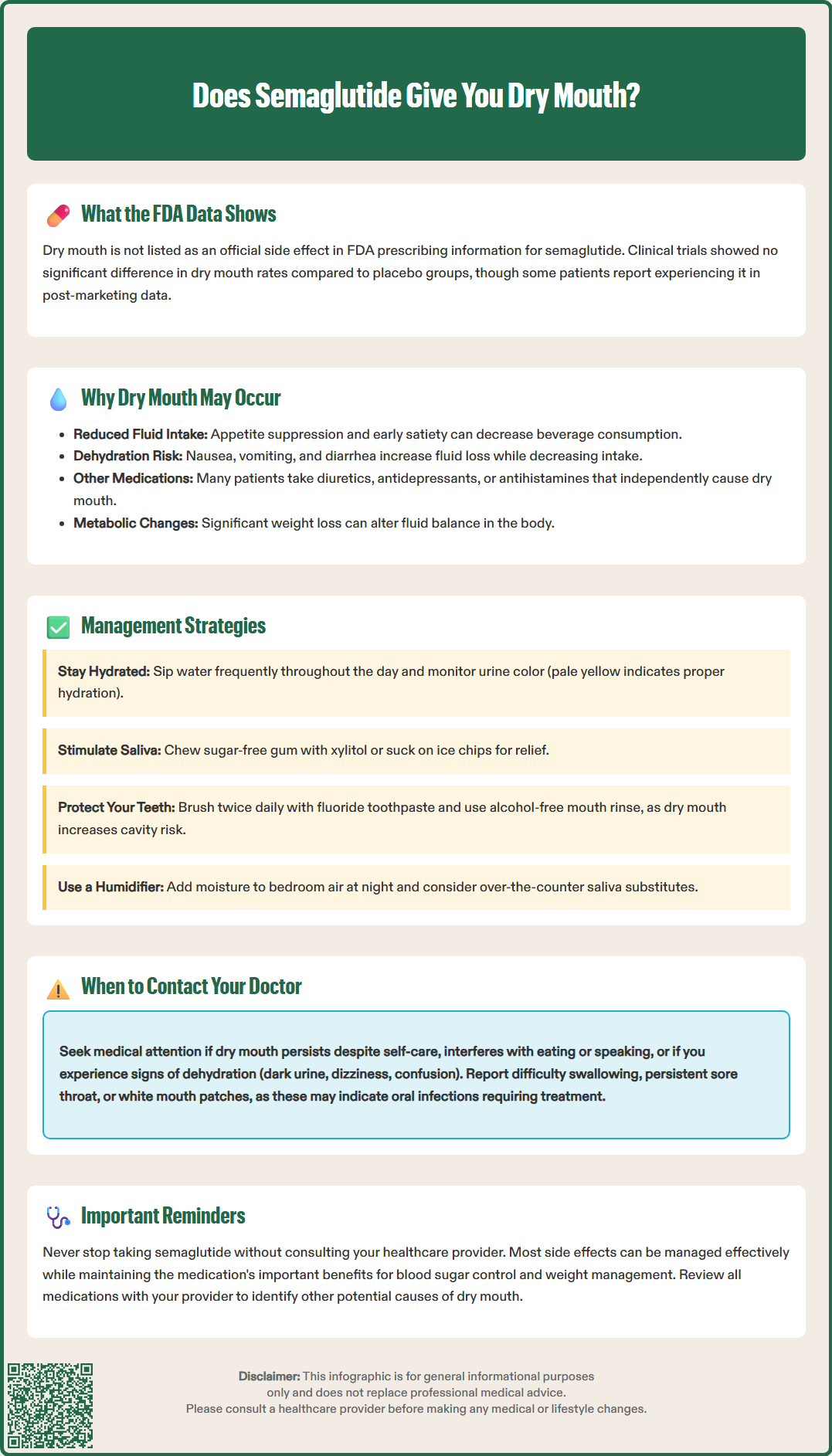
While there is no established direct effect of semaglutide on salivary gland function through its GLP-1 receptor mechanism, several indirect pathways may explain why some patients report dry mouth during treatment. The medication's pronounced effect on appetite suppression and early satiety can lead to reduced overall fluid intake. Patients experiencing nausea, vomiting, or diarrhea—common side effects, especially during dose initiation or escalation—may inadvertently decrease their consumption of both food and beverages while experiencing increased fluid losses, resulting in dehydration that manifests as oral dryness.
Dehydration represents another plausible mechanism, especially in patients achieving significant weight loss. Semaglutide's effects on body composition and metabolism can alter fluid balance, and the accompanying dietary changes may affect overall hydration status. Patients who do not consciously increase fluid intake to compensate for these physiological changes may experience symptoms of dehydration, including dry mouth, concentrated urine, and fatigue.
Polypharmacy considerations are particularly relevant in the patient populations typically prescribed semaglutide. Many individuals with type 2 diabetes or obesity take multiple medications that independently cause xerostomia, including antihypertensives (particularly diuretics), antidepressants, antihistamines, and other medications with anticholinergic properties. The temporal association between starting semaglutide and noticing dry mouth may lead patients to attribute the symptom to the new medication, when in fact it may result from the cumulative anticholinergic burden of their medication regimen. Additionally, uncontrolled hyperglycemia itself causes dry mouth through osmotic diuresis, though semaglutide's glucose-lowering effects should theoretically improve rather than worsen this symptom in patients with diabetes.
If you experience dry mouth while taking semaglutide, several evidence-based strategies can provide relief and prevent complications associated with chronic xerostomia. The cornerstone of management is maintaining adequate hydration. Aim to consume sufficient water throughout the day, distributed as regular small amounts rather than large volumes at once. Carrying a water bottle and taking frequent small sips can help maintain oral moisture and compensate for any reduction in fluid intake related to appetite changes. Monitor your urine color—pale yellow indicates adequate hydration. If you have kidney disease, heart failure, or other conditions requiring fluid restriction, consult your healthcare provider for individualized hydration guidance.
Stimulating saliva production through non-pharmacological methods can be highly effective. Sugar-free gum or lozenges containing xylitol not only promote salivary flow but also help prevent dental caries, a significant risk in patients with chronic dry mouth. Xylitol has been shown to reduce caries risk by decreasing levels of cariogenic bacteria and stimulating saliva production. Sucking on ice chips or frozen fruit pieces can provide temporary relief while contributing to overall fluid intake. Some patients find relief using over-the-counter saliva substitutes or oral moisturizing gels, which are available at most pharmacies and can be particularly helpful at night when xerostomia symptoms often worsen.
Optimizing oral hygiene becomes especially important when experiencing dry mouth, as saliva plays a crucial protective role against dental decay and periodontal disease. Brush teeth at least twice daily with fluoride toothpaste, and consider using an alcohol-free fluoride-containing mouth rinse. A humidifier in the bedroom may alleviate nighttime symptoms by maintaining moisture in the air you breathe during sleep. If you smoke, cessation is strongly recommended, as tobacco use independently causes and exacerbates dry mouth while increasing risks of oral cancer and periodontal disease. Review your complete medication list with your healthcare provider to identify any other drugs that may contribute to xerostomia, as dose adjustments or alternative medications may be possible in some cases. For severe, persistent dry mouth, prescription medications that stimulate saliva production (sialogogues) may be considered after evaluation by your healthcare provider.
While mild dry mouth is generally manageable with self-care measures, certain circumstances warrant prompt medical evaluation to rule out more serious underlying conditions or complications. Contact your healthcare provider if dry mouth persists despite adequate hydration and home management strategies, or if it significantly interferes with eating, speaking, or sleeping. Severe or worsening xerostomia may indicate an underlying condition requiring investigation, such as Sjögren's syndrome, uncontrolled diabetes, or medication interactions that need addressing.
Seek medical attention if you develop signs of dehydration beyond dry mouth, including dark-colored urine, dizziness upon standing, decreased urination, confusion, or rapid heartbeat. These symptoms may indicate inadequate fluid intake or excessive fluid loss and require assessment of your hydration status and potentially your semaglutide dose. If you experience severe gastrointestinal symptoms that prevent adequate oral intake, contact your provider promptly, as you may need to delay dose escalation or temporarily adjust your treatment.
Contact your healthcare provider immediately if you develop severe, persistent abdominal pain (especially if accompanied by vomiting), as this could indicate pancreatitis—a rare but serious potential complication of GLP-1 receptor agonists. Similarly, report right upper quadrant pain, which might suggest gallbladder disease, another recognized adverse effect of semaglutide. Additionally, if you experience difficulty swallowing, persistent sore throat, or a burning sensation in your mouth, these symptoms could indicate oral candidiasis (thrush) or other infections that are more common in individuals with reduced salivary flow and require specific treatment.
Oral health complications should prompt dental evaluation. If you notice increased dental cavities, gum inflammation, persistent bad breath despite good oral hygiene, or white patches in your mouth, schedule an appointment with your dentist. Chronic xerostomia significantly increases the risk of dental disease, and early intervention can prevent serious complications. Your healthcare provider can also assess whether dry mouth might be related to inadequate glycemic control or other aspects of your diabetes management that may need adjustment.
Finally, never discontinue semaglutide without consulting your healthcare provider, even if you attribute bothersome symptoms to the medication. Your clinician can help determine whether dry mouth is truly related to semaglutide, investigate alternative causes, adjust your treatment regimen if necessary, or provide additional management strategies. The benefits of semaglutide for glycemic control and weight management are substantial, and most side effects can be effectively managed without discontinuing this valuable therapeutic option.
No, dry mouth is not listed as a common side effect in FDA prescribing information for semaglutide products. The most common adverse effects are gastrointestinal, including nausea, vomiting, and diarrhea.
Dry mouth during semaglutide treatment may result from indirect factors such as reduced fluid intake due to appetite suppression, dehydration from gastrointestinal side effects, or concurrent medications that cause xerostomia rather than a direct effect of semaglutide itself.
Maintain adequate hydration by sipping water throughout the day, use sugar-free xylitol gum to stimulate saliva production, optimize oral hygiene with fluoride toothpaste and alcohol-free mouth rinse, and consider using a bedroom humidifier at night.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.