LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is an FDA-approved medication for type 2 diabetes and chronic weight management that works through dual incretin receptor activation. Despite some patients noticing changes in fluid balance during treatment, tirzepatide is not a diuretic and does not work by increasing urine production like traditional diuretic medications. Understanding this distinction is essential for safe medication use, as tirzepatide and diuretics serve entirely different therapeutic purposes with distinct mechanisms of action, side effect profiles, and clinical applications in medical practice.
Quick Answer: No, tirzepatide is not a diuretic medication and does not work by increasing urine production through direct kidney action.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity), tirzepatide works through its dual incretin receptor activation.
The medication mimics two naturally occurring incretin hormones that regulate glucose homeostasis and appetite. Both GIP and GLP-1 receptor activation enhance insulin secretion in a glucose-dependent manner, meaning insulin is only stimulated when blood glucose levels are elevated, reducing hypoglycemia risk. GLP-1 receptor activation also suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways that reduce appetite and food intake.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg and gradually titrated upward based on glycemic control and tolerability. The maximum approved dose is 15 mg weekly. Clinical trials have demonstrated substantial reductions in hemoglobin A1c levels (up to 2.0% or more) in type 2 diabetes, and in the SURMOUNT trials, significant weight loss (up to approximately 21% at the 15 mg dose) in patients with obesity. The medication's half-life of approximately five days supports once-weekly administration and steady-state concentrations after four weeks of therapy.
Important safety information includes a boxed warning for risk of thyroid C-cell tumors, contraindications in patients with personal/family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), and warnings about pancreatitis and gallbladder disease. When used with insulin or sulfonylureas, tirzepatide may increase hypoglycemia risk.
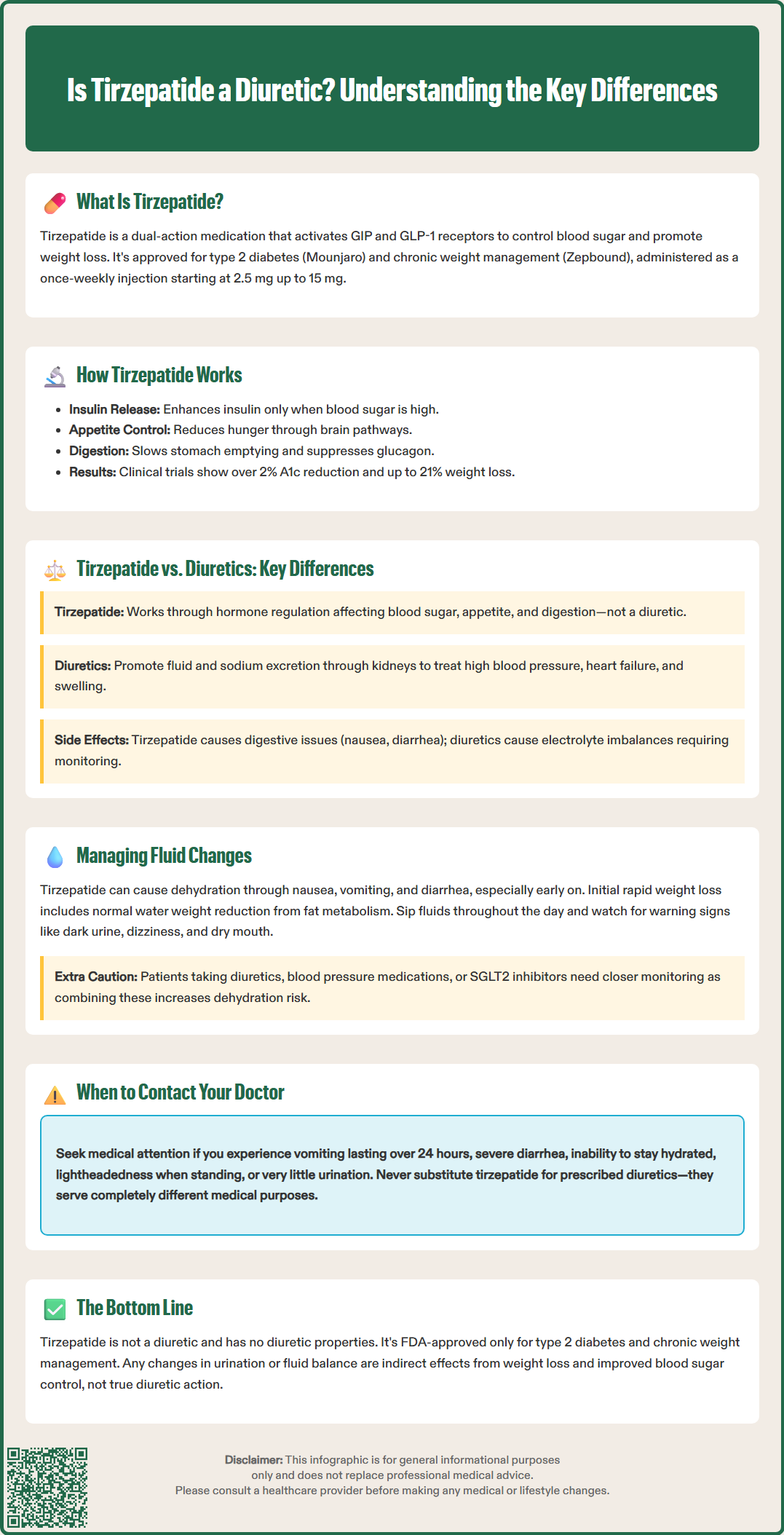
Tirzepatide and diuretic medications are fundamentally different drug classes with distinct mechanisms of action, therapeutic indications, and physiologic effects. Diuretics, commonly known as "water pills," work primarily on the kidneys to increase urine production and sodium excretion, thereby reducing fluid volume in the body. Common diuretic classes include thiazides (hydrochlorothiazide), loop diuretics (furosemide), and potassium-sparing agents (spironolactone), which are prescribed for conditions such as hypertension, heart failure, and edema. Potassium-sparing diuretics can cause hyperkalemia, especially when combined with ACE inhibitors or ARBs.
In contrast, tirzepatide is not a diuretic and does not directly act on renal tubules to promote fluid excretion. Its primary mechanisms involve incretin receptor activation affecting pancreatic hormone secretion, gastric motility, and central appetite regulation. While diuretics intentionally increase urination as their therapeutic effect, any fluid changes associated with tirzepatide occur through indirect metabolic pathways rather than direct renal action.
The clinical applications also differ substantially. Diuretics are cardiovascular medications used to manage fluid overload states and blood pressure, whereas tirzepatide is an antihyperglycemic and anti-obesity agent targeting metabolic dysfunction. Diuretics can cause electrolyte disturbances (hypokalemia, hyponatremia, hypomagnesemia) and volume depletion as predictable pharmacologic effects, requiring regular monitoring of renal function and electrolytes. Tirzepatide's adverse effect profile centers on gastrointestinal symptoms—nausea, vomiting, diarrhea, and constipation—which occur in varying frequencies based on dose and indication, generally more common during dose escalation.
Patients should understand that while both medication types may influence fluid balance, they do so through entirely different physiologic mechanisms and serve distinct therapeutic purposes in clinical practice. Tirzepatide should never be substituted for prescribed diuretic therapy, and any medication changes require physician consultation.
Although tirzepatide is not classified as a diuretic, patients may experience changes in fluid balance during treatment, primarily related to weight loss, dietary modifications, and gastrointestinal side effects. Understanding these changes and implementing appropriate management strategies is essential for safe and effective therapy.
Gastrointestinal-related fluid loss represents the most common mechanism affecting hydration status in tirzepatide users. Nausea, vomiting, and diarrhea—particularly prominent during the first few weeks after initiation or dose increases—can lead to reduced fluid intake and increased losses. Patients should be counseled to:
Maintain adequate hydration based on individual needs (aim for pale yellow urine color, unless on fluid restrictions)
Sip fluids throughout the day rather than consuming large volumes at once
Consider low- or no-sugar oral rehydration solutions if experiencing persistent vomiting or diarrhea (avoid sugar-sweetened sports drinks if you have diabetes)
Monitor for signs of dehydration including dark urine, dizziness, dry mouth, and decreased urination
Weight loss-associated fluid shifts occur as adipose tissue is metabolized and glycogen stores are depleted. Initial rapid weight loss often includes water weight reduction, which typically stabilizes after the first month of therapy. This is a normal physiologic response and differs from pathologic fluid depletion.
Patients taking concurrent medications that affect fluid balance require special consideration. Those prescribed diuretics, ACE inhibitors, ARBs, or SGLT2 inhibitors should have closer monitoring, as the combination may increase dehydration risk. Blood pressure should be checked regularly, and diuretic doses may require adjustment as weight decreases.
Patients should contact their healthcare provider if experiencing persistent vomiting (more than 24 hours), severe diarrhea, inability to maintain oral hydration, symptoms of orthostatic hypotension, or very low urine output. Seek urgent care for severe or persistent abdominal pain (which may indicate pancreatitis), right upper quadrant pain with fever or jaundice (possible gallbladder disease), or syncope.
Patients taking insulin or sulfonylureas should monitor blood glucose more frequently during illness or reduced intake and discuss medication adjustments with their healthcare provider to prevent hypoglycemia.
No, tirzepatide is definitively not a diuretic medication. There is no official pharmacologic classification of tirzepatide as a diuretic, nor does it possess diuretic properties through its mechanism of action. This distinction is important for both clinical practice and patient understanding, as the two drug classes serve entirely different therapeutic purposes and carry different risk profiles.
Tirzepatide's FDA-approved indications are for improving glycemic control in adults with type 2 diabetes mellitus (as an adjunct to diet and exercise) and for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. The medication works through dual incretin receptor agonism affecting glucose metabolism, insulin secretion, and appetite regulation—none of which involve direct renal tubular effects on sodium and water reabsorption that characterize true diuretic agents.
The confusion may arise because some patients notice changes in urination patterns or fluid balance during tirzepatide therapy. However, these observations reflect indirect effects rather than diuretic action. Weight loss naturally reduces total body water content, improved glycemic control in diabetic patients may reduce osmotic diuresis from glucosuria, and gastrointestinal side effects can temporarily affect hydration status. None of these mechanisms constitute diuretic pharmacology.
From a prescribing perspective, tirzepatide should not be considered or used as a substitute for diuretic therapy when diuretics are medically indicated for conditions such as heart failure, hypertension, or edema. Conversely, patients requiring both metabolic management with tirzepatide and cardiovascular management with diuretics can safely receive both medication classes concurrently, with appropriate clinical oversight and monitoring of volume status, renal function, and blood pressure. Healthcare providers should educate patients about this distinction to prevent medication errors and ensure appropriate expectations regarding therapeutic effects. Any questions about medication classification or appropriate use should be directed to the prescribing physician or clinical pharmacist.
Of note, tirzepatide is not recommended during pregnancy and should be discontinued if pregnancy occurs.
Tirzepatide does not directly increase urination like diuretic medications. Any changes in urination patterns typically result from improved blood sugar control reducing osmotic diuresis or from weight loss naturally affecting fluid balance, not from diuretic action on the kidneys.
No, tirzepatide cannot replace diuretic therapy. Tirzepatide treats type 2 diabetes and obesity through metabolic pathways, while diuretics manage cardiovascular conditions like heart failure, hypertension, and edema through direct kidney action. Never discontinue prescribed diuretics without physician consultation.
Yes, tirzepatide can be safely taken with diuretics under appropriate medical supervision. However, patients require closer monitoring of hydration status, blood pressure, and renal function, as the combination may increase dehydration risk, particularly during gastrointestinal side effects or dose escalation periods.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.