LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide make you sleepy? While drowsiness is not a recognized side effect of semaglutide (Ozempic, Wegovy, Rybelsus), fatigue is listed as a common adverse reaction in FDA labeling, particularly for Wegovy. This GLP-1 receptor agonist, approved for type 2 diabetes and chronic weight management, does not cause sedation through direct pharmacological mechanisms. However, many patients report tiredness during treatment due to factors including caloric restriction, gastrointestinal side effects, blood glucose changes, and nutritional adjustments. Understanding why fatigue occurs and how to manage it effectively helps patients maintain treatment benefits while optimizing energy levels and overall well-being.
Quick Answer: Semaglutide does not cause drowsiness, but fatigue is a recognized common side effect, particularly with Wegovy, occurring through indirect mechanisms rather than direct sedation.
Semaglutide, marketed under brand names including Ozempic, Wegovy, and Rybelsus, is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. While drowsiness is not listed as a common adverse effect, fatigue is recognized as a common side effect in clinical trials for Wegovy (semaglutide 2.4 mg).
According to the FDA-approved labels, the most frequently reported adverse reactions include gastrointestinal symptoms such as nausea, vomiting, diarrhea, abdominal pain, and constipation. Fatigue is specifically listed as a common adverse reaction (occurring in ≥5% of patients) in Wegovy clinical trials, though it is less prominently featured in Ozempic labeling.
It is important to distinguish between direct pharmacological effects and indirect consequences of treatment. Semaglutide works by mimicking the incretin hormone GLP-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, and slows gastric emptying. While GLP-1 receptor agonists do have central nervous system effects related to appetite regulation, they do not typically cause sedation or drowsiness as a direct pharmacologic effect.
The relationship between semaglutide and fatigue appears to be multifactorial. Understanding the potential causes of tiredness can help patients and healthcare providers manage this symptom effectively and determine whether further evaluation is necessary.
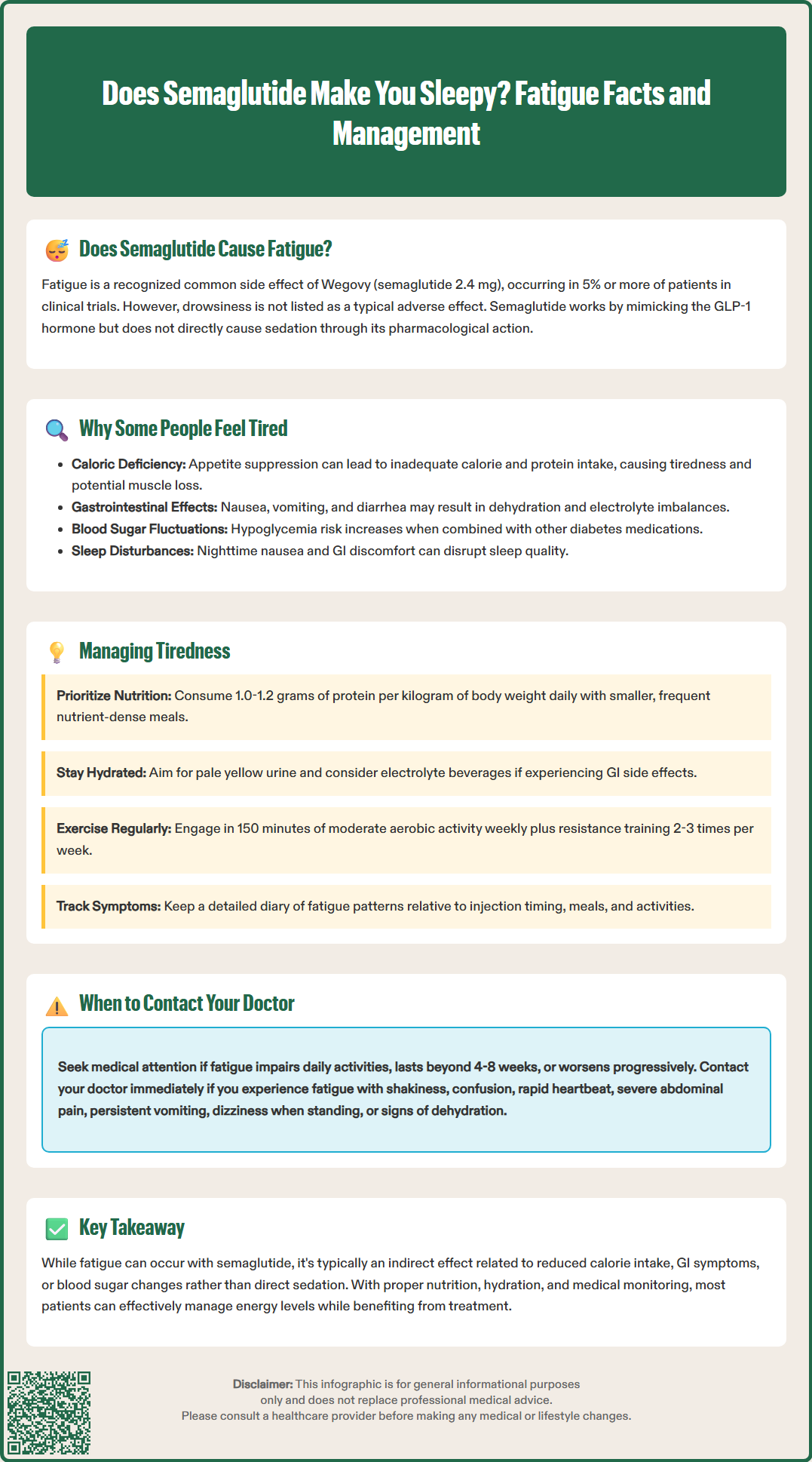
Several mechanisms may explain why some patients experience fatigue while taking semaglutide. Understanding these contributing factors is essential for appropriate management.
Caloric Restriction and Rapid Weight Loss
Semaglutide significantly reduces appetite and food intake through central and peripheral mechanisms. Patients often experience substantial caloric reduction, which can lead to feelings of tiredness, particularly if nutritional intake becomes inadequate. Rapid weight loss—common with semaglutide therapy—can temporarily affect energy levels as the body adapts to metabolic changes. Insufficient protein intake during weight loss may contribute to muscle loss and fatigue.
Gastrointestinal Side Effects
The most common adverse effects of semaglutide are gastrointestinal in nature. Persistent nausea, vomiting, or diarrhea can lead to dehydration and electrolyte imbalances, both of which commonly cause fatigue. Patients experiencing significant gastrointestinal symptoms may also reduce food and fluid intake, compounding the problem.
Blood Glucose Changes
In patients with type 2 diabetes, semaglutide improves glycemic control by lowering blood glucose levels. While hypoglycemia is relatively uncommon with semaglutide monotherapy, it can occur, particularly when combined with insulin or sulfonylureas. Both hypoglycemia and the adjustment period as glucose levels normalize can cause tiredness. Conversely, if diabetes remains poorly controlled despite treatment, hyperglycemia itself causes significant fatigue.
Sleep Disruption
Some patients report sleep disturbances related to gastrointestinal discomfort, particularly nausea that may worsen at night or early morning. Poor sleep quality naturally leads to daytime tiredness and should be considered when evaluating fatigue in patients taking semaglutide.
Other Medical Considerations
Fatigue may also be related to labeled risks such as gallbladder disease or pancreatitis, which can present with malaise along with abdominal pain. If fatigue persists, healthcare providers should consider evaluating for other common causes such as anemia, thyroid disorders, or sleep apnea.
Understanding the full adverse effect profile of semaglutide helps contextualize reports of fatigue and guides clinical management. The FDA prescribing information identifies several categories of side effects that may impact energy levels.
Gastrointestinal Effects
The most frequently reported adverse reactions with semaglutide include:
Nausea (occurring in 15-44% of patients depending on dose and indication)
Vomiting (5-24% of patients)
Diarrhea (8-30% of patients)
Constipation (11-24% of patients)
Abdominal pain (5-20% of patients)
These symptoms typically emerge during dose escalation and often improve over time. However, persistent gastrointestinal symptoms can significantly impact nutritional status, hydration, and overall well-being, potentially contributing to fatigue.
Metabolic and Endocrine Effects
Semaglutide affects multiple metabolic parameters. In patients with type 2 diabetes, improved glycemic control is therapeutic, but the transition period may involve symptoms as the body adjusts. Hypoglycemia risk increases when semaglutide is combined with insulin or insulin secretagogues, requiring dose adjustments of concomitant medications.
Patients with diabetes and retinopathy should be monitored closely, as rapid improvement in glucose control may be associated with temporary worsening of retinopathy.
Other Relevant Adverse Effects
Additional side effects that may indirectly affect energy include:
Fatigue (listed as a common adverse reaction for Wegovy)
Decreased appetite (very common, often therapeutic but may lead to inadequate nutrition)
Headache (reported in clinical trials)
Dizziness (may be related to dehydration or blood pressure changes)
Gallbladder problems (including gallstones, which may present with fatigue and abdominal pain)
While these effects do not constitute direct sedation or drowsiness, their cumulative impact on physical well-being can manifest as reduced energy and increased tiredness. The American Diabetes Association Standards of Care emphasize the importance of monitoring for adverse effects and adjusting treatment as needed to optimize tolerability while maintaining therapeutic benefit.
While mild tiredness during the initial weeks of semaglutide treatment may resolve as the body adjusts, certain presentations of fatigue warrant prompt medical evaluation. Patients should be educated about warning signs that require clinical assessment.
Severe or Persistent Fatigue
Fatigue that significantly impairs daily functioning, persists beyond the initial adjustment period (typically 4-8 weeks), or progressively worsens requires medical evaluation. This may indicate inadequate nutrition, an underlying medical condition, or a need for treatment modification.
Symptoms Suggesting Hypoglycemia
Patients should contact their healthcare provider if fatigue is accompanied by:
Shakiness, trembling, or sweating
Confusion or difficulty concentrating
Rapid heartbeat or palpitations
Extreme hunger
Irritability or mood changes
These symptoms may indicate low blood glucose, particularly in patients taking semaglutide with insulin or sulfonylureas. Dose adjustments of concomitant diabetes medications may be necessary.
Signs of Dehydration or Electrolyte Imbalance
Severe or persistent gastrointestinal side effects can lead to dehydration and potentially acute kidney injury. Warning signs include:
Dizziness upon standing
Decreased urination or dark urine
Dry mouth and increased thirst
Muscle weakness or cramping
Other Concerning Symptoms
Immediate medical attention is warranted if fatigue occurs with:
Severe abdominal pain (may indicate pancreatitis)
Right upper quadrant pain, fever, or yellowing of skin/eyes (signs of gallbladder disease)
Persistent vomiting preventing fluid intake
Visual changes or severe headache (especially in patients with diabetes and retinopathy)
Chest pain or shortness of breath
Signs of allergic reaction (rash, swelling, difficulty breathing)
The American Diabetes Association Standards of Care recommend regular monitoring of patients on GLP-1 receptor agonists, including assessment of tolerability, glycemic control, weight changes, and overall well-being. Patients should maintain open communication with their healthcare team about any concerning symptoms.
For patients experiencing fatigue while taking semaglutide, several evidence-based strategies can help manage this symptom while maintaining the therapeutic benefits of treatment.
Nutritional Optimization
Despite reduced appetite, maintaining adequate nutrition is essential:
Ensure sufficient caloric intake: Work with a healthcare provider or registered dietitian to establish appropriate caloric goals that support gradual, healthy weight loss without excessive restriction
Prioritize protein: During weight loss, aim for approximately 1.0-1.2 grams of protein per kilogram of body weight daily to preserve lean muscle mass (patients with kidney disease should follow their provider's specific recommendations)
Focus on nutrient density: Choose foods rich in vitamins, minerals, and complex carbohydrates to support energy levels
Eat smaller, frequent meals: This approach may be better tolerated given semaglutide's effect on gastric emptying
Hydration and Electrolyte Balance
Adequate fluid intake is crucial, particularly if experiencing gastrointestinal side effects. Aim for sufficient hydration to maintain pale yellow urine, and consider electrolyte-containing beverages if experiencing vomiting or diarrhea. Patients with heart failure, kidney disease, or other conditions requiring fluid restrictions should follow their healthcare provider's specific guidance.
Medication Timing and Dose Adjustment
Injectable semaglutide (Ozempic, Wegovy) is administered once weekly, while oral semaglutide (Rybelsus) is taken daily. Some patients find that side effects peak in the days following injection. Planning rest periods accordingly may help. If side effects are severe, discuss with your healthcare provider whether a slower dose escalation schedule might improve tolerability. The FDA-approved dosing includes gradual titration specifically to minimize adverse effects.
Sleep Hygiene and Physical Activity
Maintaining regular sleep schedules and engaging in appropriate physical activity can improve energy levels. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity weekly, plus resistance training 2-3 times per week as tolerated, adjusted based on individual capacity and medical status.
Monitoring and Follow-up
Regular monitoring of blood glucose levels (for patients with diabetes), body weight, and overall symptom burden helps identify issues early. Keep a symptom diary to discuss with your healthcare provider, noting patterns in fatigue relative to injection timing, meals, and activities. This information guides treatment optimization and helps distinguish between adjustment-period symptoms and those requiring intervention.
Drowsiness is not a recognized side effect of semaglutide. However, fatigue is listed as a common adverse reaction in FDA labeling, particularly for Wegovy, occurring through indirect mechanisms such as caloric restriction and gastrointestinal effects rather than direct sedation.
Tiredness on semaglutide typically results from reduced caloric intake, gastrointestinal side effects causing dehydration, blood glucose changes as your body adjusts, or inadequate protein intake during weight loss. These factors are manageable with proper nutrition, hydration, and medical monitoring.
Contact your healthcare provider if fatigue is severe, persists beyond 4-8 weeks, impairs daily functioning, or occurs with symptoms of hypoglycemia, dehydration, severe abdominal pain, or persistent vomiting. These may indicate a need for treatment adjustment or evaluation of underlying conditions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.