LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Will semaglutide give me energy? This common question reflects patients' experiences with this FDA-approved medication for type 2 diabetes and weight management. Semaglutide (Ozempic, Wegovy, Rybelsus) is a GLP-1 receptor agonist that works by mimicking natural hormones to regulate blood sugar and reduce appetite. While it doesn't directly boost energy like a stimulant, many patients report feeling more energetic through indirect effects. Understanding how semaglutide affects your body, what changes to expect, and when energy improvements typically occur helps set realistic expectations for treatment outcomes.
Quick Answer: Semaglutide does not directly provide energy but may improve energy levels indirectly through better blood sugar control, weight loss, and improved metabolic health over several months of treatment.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Ozempic, Rybelsus) and chronic weight management (Wegovy) at different doses. This medication mimics the action of naturally occurring GLP-1, a hormone released by your intestines after eating. By binding to GLP-1 receptors throughout your body, semaglutide triggers several important metabolic effects.
The primary mechanism involves enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it stimulates insulin release only when blood sugar levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications. Simultaneously, semaglutide suppresses glucagon secretion, a hormone that raises blood sugar, further contributing to improved glycemic control.
Beyond glucose regulation, semaglutide slows gastric emptying, particularly during initial treatment (this effect may diminish over time with chronic therapy). This delayed emptying prolongs the feeling of fullness after meals and reduces appetite through central nervous system pathways. The medication should be avoided in patients with severe gastroparesis. The appetite suppression is the primary mechanism behind its effectiveness for weight loss. The medication also appears to influence areas of the brain involved in reward and food intake regulation.
It is important to understand that semaglutide does not directly provide energy or act as a stimulant. Unlike caffeine or amphetamines, it does not increase metabolic rate or directly boost energy levels through central nervous system stimulation. Any changes in energy that patients experience are typically indirect effects related to weight loss, improved blood sugar control, or changes in eating patterns rather than a direct pharmacological action on energy production.
Note: Semaglutide carries an FDA boxed warning about the risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Many patients report feeling more energetic after starting semaglutide, though this is not a direct effect of the medication itself. These improvements in energy levels typically result from several interconnected factors related to metabolic health and weight management.
Improved glycemic control is often the first contributor to better energy levels. When blood sugar levels stabilize within a healthier range, patients with type 2 diabetes frequently experience reduced fatigue. The extreme fluctuations between hyperglycemia and relative hypoglycemia can cause significant tiredness, brain fog, and lethargy. As semaglutide helps maintain more consistent glucose levels, many people notice they feel more alert and capable throughout the day.
Weight loss represents another significant factor in improved energy. Carrying excess weight places considerable strain on the cardiovascular system, joints, and overall metabolism. Clinical trials show that patients on Wegovy (semaglutide 2.4 mg) achieve average weight loss of approximately 15% in non-diabetic populations (somewhat lower in those with type 2 diabetes), though individual results vary. As weight decreases, patients typically experience:
Reduced joint pain and improved mobility
Potential improvements in sleep quality and sleep-disordered breathing (though semaglutide is not FDA-approved to treat sleep apnea)
Possible improvements in cardiovascular function and stamina as a result of weight reduction
Enhanced ability to engage in physical activity
Additionally, improved self-efficacy and mood can contribute to perceived energy increases. Successfully managing weight and diabetes often leads to better mental health and increased motivation to engage in healthy behaviors. This psychological boost can translate into feeling more energetic and engaged in daily activities. However, it's important to monitor for mood changes during treatment, as depression and suicidal ideation have been reported with semaglutide and require medical attention.
It is worth noting that these energy improvements typically develop gradually over weeks to months as metabolic changes occur, rather than immediately after starting treatment.
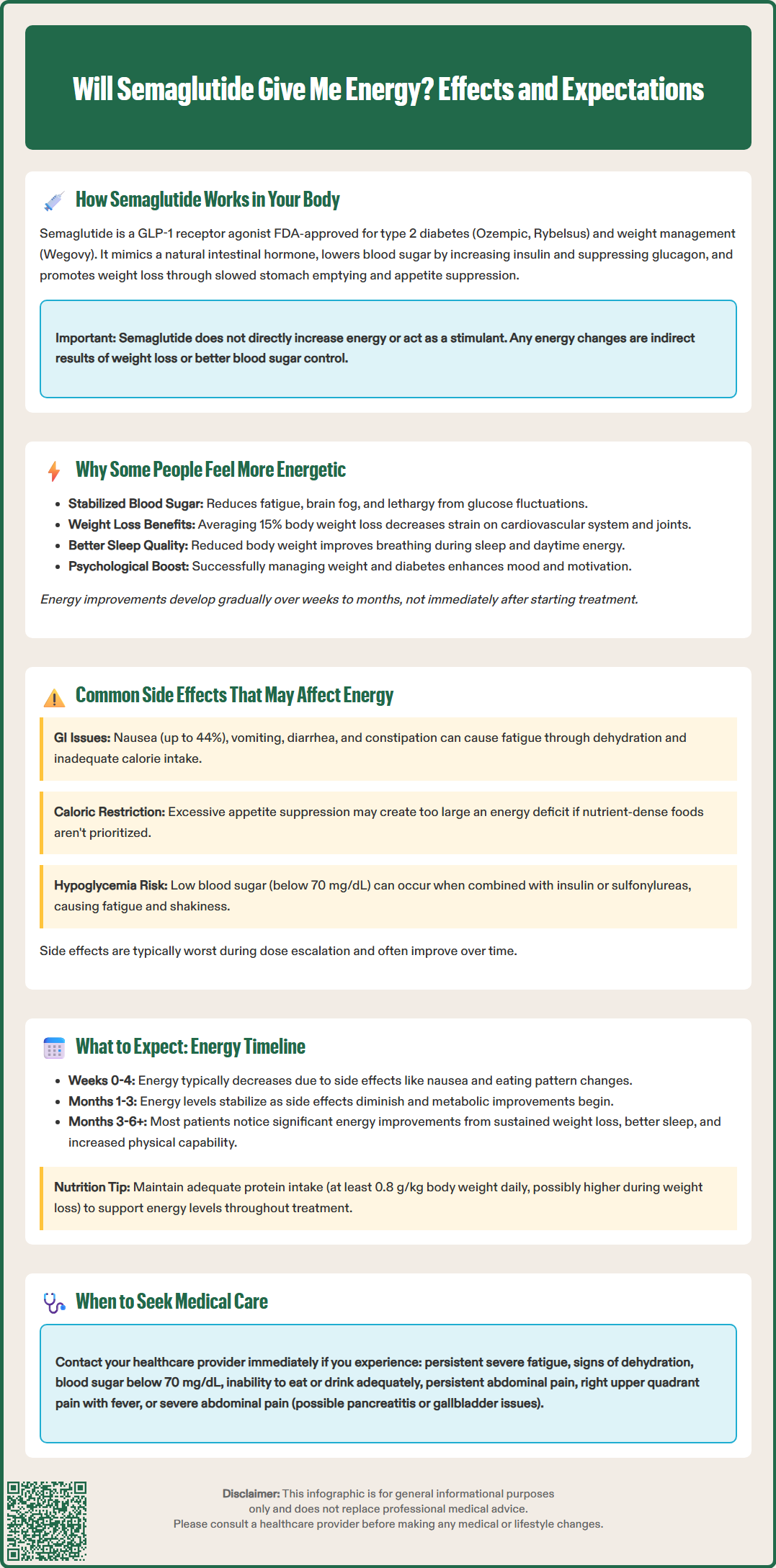
While some patients experience improved energy on semaglutide, others may initially feel more fatigued due to common side effects. Understanding these potential adverse effects helps set realistic expectations during treatment initiation.
Gastrointestinal side effects are the most frequently reported issues with semaglutide and can significantly impact energy levels. According to FDA labeling, nausea occurs in approximately 44% of patients on Wegovy (2.4 mg for weight management) and 15-20% on lower diabetes doses, with vomiting, diarrhea, constipation, and abdominal pain also common. These symptoms are typically most pronounced during dose escalation and often improve over time. However, persistent nausea and reduced food intake can lead to:
Inadequate caloric intake causing fatigue
Dehydration from vomiting or diarrhea
Electrolyte imbalances affecting muscle function
Difficulty maintaining proper nutrition
Patients experiencing severe or persistent gastrointestinal symptoms should contact their healthcare provider, as dose adjustment or slower titration may be necessary. Seek immediate medical attention for severe, persistent abdominal pain (which may indicate pancreatitis), right upper quadrant pain with fever or jaundice (possible gallbladder disease), or signs of severe dehydration.
Reduced caloric intake, while intended for weight loss, can sometimes lead to insufficient energy consumption, particularly if patients are not eating nutrient-dense foods. Some individuals may inadvertently create too large a caloric deficit, resulting in fatigue, weakness, and difficulty concentrating. This is especially relevant for patients who experience significant appetite suppression.
Hypoglycemia can occur, particularly in patients taking semaglutide alongside insulin or sulfonylureas. Low blood sugar (below 70 mg/dL) causes fatigue, shakiness, confusion, and weakness. The American Diabetes Association recommends regular blood glucose monitoring and potential adjustment of insulin or sulfonylurea doses when starting semaglutide to prevent hypoglycemia.
Other side effects that may indirectly affect energy include headache, dizziness, and fatigue itself, which are listed as potential adverse effects in clinical trials. If you experience persistent fatigue, weakness, or other concerning symptoms, medical evaluation is warranted to rule out complications or the need for treatment modification.
Energy levels on semaglutide typically follow a predictable pattern, though individual experiences vary considerably. Understanding this timeline helps patients maintain realistic expectations and recognize when medical consultation is needed.
Initial weeks (0-4 weeks): During treatment initiation, many patients experience decreased energy due to side effects. Nausea, changes in eating patterns, and adjustment to the medication commonly cause temporary fatigue. This is normal and typically improves as your body adapts. Starting at a low dose and gradually increasing, as prescribed, helps minimize these effects. Staying well-hydrated, eating small frequent meals, and avoiding high-fat foods can help manage gastrointestinal symptoms during this period.
Months 1-3: As side effects diminish and metabolic improvements begin, energy levels often stabilize or start improving. Patients with diabetes typically notice better glycemic control, which may translate to reduced fatigue. Weight loss becomes more apparent, though significant improvements in mobility and stamina may not yet be fully realized. This is a critical period for establishing healthy eating patterns that provide adequate nutrition despite reduced appetite.
Months 3-6 and beyond: Most patients who will experience energy improvements notice them during this timeframe. Sustained weight loss, improved metabolic health, better sleep quality, and increased physical capability contribute to enhanced energy levels. However, it is essential to ensure adequate protein intake (the National Academies of Sciences, Engineering, and Medicine recommends 0.8 g/kg body weight daily for adults, though some experts suggest higher amounts during weight loss) and overall nutrition to support energy needs.
When to seek medical advice: Contact your healthcare provider if you experience:
Persistent, severe fatigue that interferes with daily activities
Signs of dehydration (dark urine, dizziness, decreased urination)
Symptoms of hypoglycemia (blood glucose <70 mg/dL, shakiness, confusion, rapid heartbeat)
Inability to maintain adequate nutrition or hydration
Unexplained weakness or muscle pain
Severe, persistent abdominal pain (possible pancreatitis)
Right upper abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Worsening mood, depression, or thoughts of self-harm
Regular follow-up appointments allow monitoring of metabolic parameters, nutritional status, and overall response to treatment, ensuring semaglutide therapy remains safe and effective for your individual needs.
No, semaglutide does not act as a stimulant or directly increase metabolic rate. Any energy improvements result from indirect effects such as better blood sugar control, weight loss, and improved overall metabolic health rather than central nervous system stimulation.
Most patients who experience energy improvements notice them after 3-6 months of treatment as metabolic changes occur, weight decreases, and side effects diminish. Initial weeks may involve decreased energy due to gastrointestinal side effects and adjustment to the medication.
Yes, semaglutide can cause fatigue, particularly during initial treatment due to gastrointestinal side effects, inadequate caloric intake, dehydration, or hypoglycemia when combined with insulin or sulfonylureas. Persistent severe fatigue warrants medical evaluation to rule out complications or need for dose adjustment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.