LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide make you urinate a lot? This common question arises among patients prescribed Ozempic or Wegovy for type 2 diabetes or weight management. Semaglutide, a GLP-1 receptor agonist, does not typically cause increased urination as a direct side effect. The FDA prescribing information does not list urinary frequency among common adverse reactions. However, patients may notice changes in urination patterns due to improved blood sugar control, concurrent medications like SGLT2 inhibitors, or unrelated medical conditions. Understanding the relationship between semaglutide and urinary symptoms helps patients distinguish normal treatment responses from issues requiring medical evaluation.
Quick Answer: Semaglutide does not typically cause increased urination as a direct side effect according to FDA prescribing information.
Semaglutide, marketed under brand names including Ozempic and Wegovy, is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. Increased urination is not listed as a common adverse effect in the official FDA prescribing information for these medications.
While there is limited evidence that GLP-1 receptor activation may influence sodium excretion (natriuresis) in experimental settings, this has not translated to clinically significant urinary frequency in clinical trials or post-marketing surveillance. Semaglutide works primarily by enhancing insulin secretion in response to elevated glucose levels, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
Indirect factors may contribute to perceived changes in urination patterns. Significant weight loss—a common outcome with semaglutide therapy—can lead to improved insulin sensitivity and better glycemic control in patients with type 2 diabetes. As blood glucose levels normalize, the osmotic diuresis associated with uncontrolled hyperglycemia diminishes, which may paradoxically make patients more aware of normal urinary patterns.
Importantly, other medications commonly prescribed alongside semaglutide may cause increased urination, particularly SGLT2 inhibitors (like empagliflozin, dapagliflozin) and diuretics. When evaluating urinary changes, clinicians should distinguish between polyuria (>3 liters of urine output daily) and urinary frequency (>8 voids per day), as these have different causes and implications.
Patients experiencing new or bothersome urinary symptoms while taking semaglutide should not assume the medication is directly responsible. A thorough clinical evaluation is warranted to identify alternative explanations and ensure appropriate management.
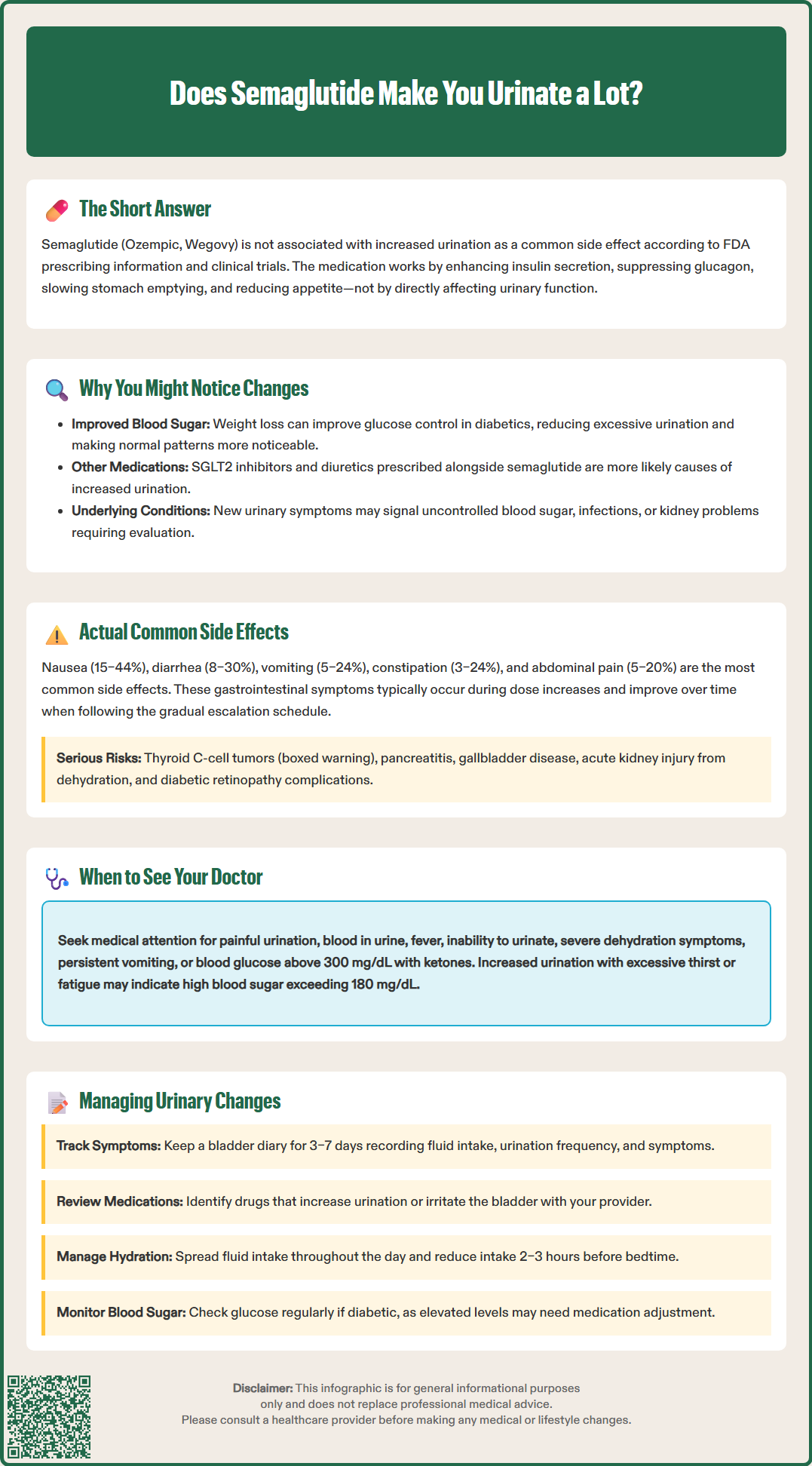
The most frequently reported adverse effects of semaglutide are gastrointestinal in nature, reflecting the medication's mechanism of slowing gastric emptying and its effects on the gastrointestinal tract. According to FDA-approved labeling and clinical trial data, the following side effects occur most commonly:
Gastrointestinal Effects:
Nausea (affecting 15–44% of patients, with higher rates at Wegovy doses)
Diarrhea (reported in 8–30% of patients)
Vomiting (5–24% incidence)
Constipation (occurring in 3–24% of patients)
Abdominal pain (5–20% of patients)
These gastrointestinal symptoms typically emerge during dose escalation and often diminish with continued therapy as physiological adaptation occurs. The FDA-approved dosing schedule includes gradual titration specifically to minimize these effects.
Other Notable Adverse Effects:
Injection site reactions (mild erythema, pruritus, or discomfort)
Fatigue and dizziness
Headache
Hypoglycemia (primarily when combined with insulin or sulfonylureas; rare with semaglutide monotherapy)
Important Warnings and Precautions:
Thyroid C-cell tumors (boxed warning based on animal data; contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2)
Pancreatitis (acute inflammation presenting with severe abdominal pain)
Gallbladder disease (cholecystitis or cholelithiasis)
Acute kidney injury (risk increases with severe gastrointestinal adverse events causing dehydration)
Diabetic retinopathy complications (for Ozempic; patients with history of retinopathy should be monitored)
Suicidal behavior or thinking (for Wegovy; monitor for depression or suicidal thoughts)
Patients should be counseled that gastrointestinal side effects are expected and manageable, while urinary symptoms are not characteristic adverse effects of semaglutide therapy. Any persistent or concerning symptoms warrant medical evaluation to distinguish medication effects from unrelated conditions.
While semaglutide itself does not typically cause increased urination, new or worsening urinary symptoms during treatment may indicate underlying medical conditions requiring prompt evaluation. Clinicians and patients should remain vigilant for the following scenarios:
Uncontrolled Hyperglycemia: In patients with type 2 diabetes, increased urination accompanied by excessive thirst (polydipsia), unexplained weight loss, or fatigue may signal inadequate glycemic control. When blood glucose exceeds the renal threshold (typically around 180 mg/dL, though this varies between individuals), glucose appears in urine, creating an osmotic diuresis that increases urine volume. Patients should check fingerstick glucose levels and contact their healthcare provider if readings consistently exceed target ranges. For blood glucose >250-300 mg/dL with nausea, vomiting, or abdominal pain, patients should check for ketones and seek urgent care per American Diabetes Association sick-day guidance.
Medication Effects: SGLT2 inhibitors (such as empagliflozin, dapagliflozin, canagliflozin) commonly cause increased urination and genital/urinary tract infections as direct pharmacological effects. Diuretics also increase urine output by design. Reviewing the complete medication list is essential when evaluating new urinary symptoms.
Urinary Tract Infection (UTI): Frequent urination accompanied by dysuria (painful urination), urgency, suprapubic discomfort, or cloudy/malodorous urine suggests possible UTI. Patients with diabetes face increased UTI risk due to multiple factors including altered immune function and bladder emptying. Urinalysis and urine culture are indicated, with appropriate antibiotic therapy if infection is confirmed.
Dehydration and Acute Kidney Injury: Severe gastrointestinal side effects from semaglutide can lead to dehydration and potentially acute kidney injury. Warning signs include decreased urine output despite increased frequency attempts, dark urine, dizziness, rapid heartbeat, or confusion. The FDA label for semaglutide products includes a warning to monitor renal function in patients experiencing severe adverse gastrointestinal reactions.
Other Urological Conditions: New urinary symptoms may reflect unrelated conditions such as overactive bladder, benign prostatic hyperplasia in men, interstitial cystitis, or rarely, bladder malignancy. Persistent symptoms lasting beyond initial treatment adaptation warrant urological evaluation, including urinalysis, post-void residual measurement, and potentially cystoscopy or imaging studies depending on clinical presentation.
Patients experiencing urinary changes during semaglutide therapy can implement several practical strategies while working with their healthcare team to identify and address underlying causes:
Monitoring and Documentation: Maintaining a bladder diary for 3–7 days provides valuable clinical information. Patients should record fluid intake volume and timing, urination frequency, approximate urine volume, and any associated symptoms (urgency, discomfort, nocturia). This objective data helps clinicians distinguish between true polyuria (excessive urine production) and urinary frequency with normal total volume, guiding appropriate investigation.
Medication Review: Patients should review all medications with their healthcare provider, particularly identifying those that can increase urination (SGLT2 inhibitors, diuretics) or irritate the bladder (caffeine-containing products). Adjusting the timing or dosage of these medications may help manage symptoms.
Hydration Management: Adequate hydration remains essential, particularly given semaglutide's gastrointestinal effects. However, patients should distribute fluid intake throughout the day rather than consuming large volumes at once, and consider reducing intake 2–3 hours before bedtime to minimize nocturia. Hydration needs should be individualized based on activity level, climate, concurrent medical conditions, and thirst. Patients should avoid excessive fluid intake beyond physiological needs, as this can increase urinary frequency unnecessarily.
Glycemic Monitoring: Patients with diabetes should check blood glucose levels regularly, particularly if urinary symptoms emerge or worsen. Consistent readings above target ranges suggest the need for medication adjustment. The American Diabetes Association recommends A1C testing every 3 months when therapy changes or targets are not met.
Lifestyle Modifications:
Limit bladder irritants: Caffeine, alcohol, artificial sweeteners, and acidic foods may exacerbate urinary frequency
Pelvic floor exercises: Kegel exercises can improve bladder control
Timed voiding: Scheduled bathroom visits every 2–3 hours may reduce urgency
When to Seek Medical Attention: Patients should contact their healthcare provider immediately if they experience:
Painful urination or blood in urine
Fever or signs of infection
Inability to urinate despite urgency
Severe abdominal or flank pain
Signs of dehydration (dizziness, confusion, decreased urine output)
Persistent vomiting or inability to keep fluids down
Blood glucose >300 mg/dL with ketones present
Symptoms of diabetic ketoacidosis (fruity breath, confusion, rapid breathing)
These symptoms require prompt evaluation to exclude serious conditions. Routine follow-up should include discussion of any urinary changes, allowing clinicians to determine whether investigation beyond standard diabetes monitoring is warranted.
The most common side effects of semaglutide are gastrointestinal, including nausea (15–44% of patients), diarrhea (8–30%), vomiting (5–24%), constipation (3–24%), and abdominal pain (5–20%). These symptoms typically occur during dose escalation and often improve with continued therapy.
Semaglutide itself does not directly cause urinary tract infections. However, patients with diabetes have increased UTI risk due to factors like altered immune function. If you experience painful urination, urgency, or cloudy urine while taking semaglutide, contact your healthcare provider for evaluation.
Contact your healthcare provider immediately if you experience painful urination, blood in urine, fever, inability to urinate despite urgency, severe abdominal pain, signs of dehydration, or blood glucose above 300 mg/dL with ketones present. These symptoms require prompt medical evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.