LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
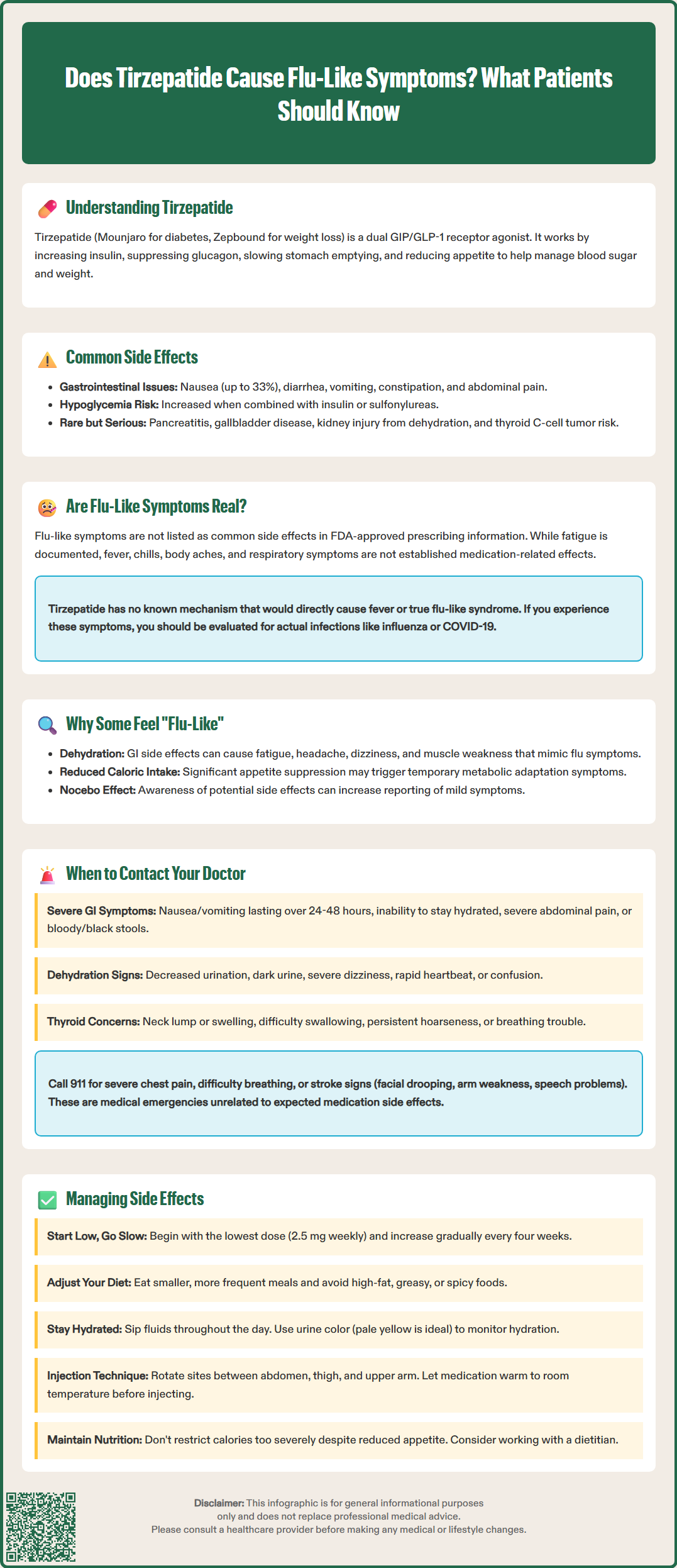
Tirzepatide (Mounjaro, Zepbound) is an FDA-approved dual GIP/GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While gastrointestinal side effects like nausea and diarrhea are well-documented, some patients report flu-like symptoms during treatment. Understanding whether tirzepatide directly causes these symptoms—or if they result from dehydration, metabolic changes, or concurrent illness—is essential for appropriate management. This article examines the evidence regarding flu-like reactions to tirzepatide, explores potential mechanisms, and provides guidance on when to seek medical evaluation and how to manage side effects effectively.
Quick Answer: Flu-like symptoms are not listed as common adverse effects in FDA prescribing information for tirzepatide, though some patients report fatigue and systemic symptoms that may be related to dehydration or metabolic adaptation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound). This medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
The most commonly reported adverse effects of tirzepatide are gastrointestinal in nature. These include nausea, diarrhea, vomiting, constipation, abdominal pain, dyspepsia, and decreased appetite . According to FDA prescribing information, gastrointestinal side effects vary by dose and indication, with nausea occurring in up to approximately 33% of patients taking Zepbound (with somewhat lower rates for Mounjaro). Additional side effects with Zepbound may include GERD, eructation (belching), and alopecia (hair loss). Injection site reactions and fatigue are also commonly reported.
Hypoglycemia is a risk when tirzepatide is used in combination with insulin or insulin secretagogues (such as sulfonylureas); clinicians should consider lowering doses of these medications to reduce this risk. Serious but rare risks include pancreatitis, gallbladder disease, acute kidney injury (usually secondary to dehydration from gastrointestinal losses), and hypersensitivity reactions.
The medication carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. The medication may cause fetal harm and is not recommended during pregnancy; weight loss therapy is generally not recommended during pregnancy or lactation.
Understanding the expected side effect profile helps patients and clinicians distinguish between typical medication responses and symptoms that may warrant further evaluation or intervention.
Flu-like symptoms are not listed as a common or characteristic adverse effect in the FDA-approved prescribing information for tirzepatide. The official product labeling does not identify fever, chills, body aches, or respiratory symptoms as typical reactions to this medication. However, some patients have reported symptoms they describe as "flu-like" when initiating or escalating tirzepatide therapy.
It is important to distinguish between true influenza or viral illness and medication-related symptoms that patients may perceive as flu-like. Fatigue is documented in the FDA labeling (particularly for Zepbound), while other symptoms that can overlap with viral syndromes have been reported with variable frequency in clinical trials but may not be established as causally related to the medication.
The gastrointestinal side effects of tirzepatide, particularly nausea, vomiting, and diarrhea, can sometimes be accompanied by systemic symptoms such as weakness, lightheadedness, or body discomfort. When these occur together, patients may interpret the constellation of symptoms as flu-like, even though they represent medication side effects rather than infectious illness.
There is no established pharmacological mechanism by which tirzepatide would directly cause fever or true flu-like syndrome. If patients develop fever, significant body aches, respiratory symptoms, or other signs consistent with infection while taking tirzepatide, these symptoms should be evaluated as potentially representing an intercurrent illness rather than being attributed solely to the medication. Concurrent viral infections, including influenza or COVID-19, remain possible and should be considered in the differential diagnosis. Following CDC guidance for testing and evaluation of potential infectious symptoms is appropriate in these situations.
Several factors may explain why some patients report flu-like symptoms when taking tirzepatide, even though these are not formally recognized adverse effects. Understanding these mechanisms can help clinicians counsel patients appropriately and manage expectations during treatment initiation.
Dehydration and electrolyte imbalance represent one plausible explanation. The gastrointestinal side effects of tirzepatide—particularly nausea, vomiting, and diarrhea—can lead to fluid and electrolyte losses. Dehydration commonly produces symptoms including fatigue, headache, dizziness, muscle weakness, and general malaise, which patients may interpret as flu-like. This is particularly relevant during dose escalation periods when gastrointestinal symptoms tend to be most pronounced. Orthostatic symptoms (lightheadedness when standing) may be an early sign of dehydration.
Metabolic adaptation associated with caloric restriction and weight loss may also contribute to systemic symptoms. As patients experience significant appetite suppression and reduced food intake, they may experience transient symptoms including fatigue, headache, and body discomfort. These adaptive responses, while generally temporary, can produce systemic symptoms during the initial treatment period.
Nocebo effects and heightened symptom awareness should not be discounted. Patients who are informed about potential side effects or who read about others' experiences may be more likely to notice and report mild systemic symptoms that might otherwise go unrecognized. The timing of symptom onset—often coinciding with medication initiation—can reinforce the perceived association even when causality is uncertain.
While some preclinical research has explored potential immunomodulatory effects of GLP-1 receptor agonists, there is currently insufficient clinical evidence to establish this as a mechanism for systemic symptoms in patients taking tirzepatide. Patients experiencing persistent systemic symptoms should be evaluated for other causes, including intercurrent illness or dehydration.
While many side effects of tirzepatide are self-limited and manageable, certain symptoms warrant prompt medical evaluation. Patients should be counseled to contact their healthcare provider if they experience any of the following:
Severe or persistent gastrointestinal symptoms including intractable nausea or vomiting lasting more than 24-48 hours, inability to maintain adequate oral hydration, severe abdominal pain (particularly if localized to the upper abdomen or radiating to the back), or signs of gastrointestinal bleeding such as bloody or black stools. These may indicate complications such as pancreatitis, gallbladder disease, or severe dehydration requiring intervention.
Signs of dehydration including decreased urine output, dark-colored urine, severe dizziness or lightheadedness (particularly upon standing), rapid heartbeat, confusion, or extreme weakness. Dehydration can lead to acute kidney injury, particularly in patients with pre-existing renal impairment or those taking concurrent medications affecting kidney function.
Fever above 100.4°F (38°C) should prompt evaluation, as this is not an expected side effect of tirzepatide and more likely represents an infectious process requiring diagnosis and treatment. Similarly, respiratory symptoms such as cough, shortness of breath, or chest pain warrant assessment, as these are not attributable to the medication.
Thyroid-related symptoms including a lump or swelling in the neck, difficulty swallowing, persistent hoarseness, or trouble breathing should be promptly evaluated due to the boxed warning regarding thyroid C-cell tumors.
Hypersensitivity reactions including rash, itching, swelling of the face or throat, or difficulty breathing require immediate medical attention. While rare, serious allergic reactions can occur with any medication.
Hypoglycemia symptoms such as shakiness, sweating, confusion, or rapid heartbeat are particularly important in patients taking tirzepatide in combination with insulin or sulfonylureas. Patients should be educated on recognizing and treating low blood sugar appropriately.
Call 911 or emergency services immediately for severe chest pain, difficulty breathing, signs of stroke (facial drooping, arm weakness, speech difficulties), or other severe or life-threatening symptoms.
Patients should also report persistent fatigue, headache, or malaise that significantly impacts daily functioning or does not improve within one to two weeks of medication initiation or dose adjustment.
Effective management of tirzepatide-related side effects can improve treatment adherence and patient outcomes. Evidence-based strategies focus primarily on preventing and managing gastrointestinal symptoms, maintaining hydration, and supporting patients through the adaptation period.
Gradual dose titration is the cornerstone of side effect management. The FDA-approved dosing schedule involves starting at 2.5 mg subcutaneously once weekly and increasing by 2.5 mg increments every four weeks as tolerated, with available strengths of 2.5, 5, 7.5, 10, 12.5, and 15 mg. This gradual escalation allows the body to adapt to the medication's effects. Clinicians may delay dose escalation, maintain a current dose longer than 4 weeks, return to a previously tolerated dose, or temporarily interrupt treatment if patients experience significant side effects.
Dietary modifications can substantially reduce gastrointestinal symptoms. Patients should be advised to eat smaller, more frequent meals rather than large portions; avoid high-fat, greasy, or spicy foods that may exacerbate nausea; choose bland, easily digestible options during periods of increased symptoms; and eat slowly to accommodate delayed gastric emptying. Avoiding lying down immediately after eating can also help reduce nausea and reflux symptoms.
Hydration strategies are critical, particularly for patients experiencing vomiting or diarrhea. Patients should aim for adequate fluid intake throughout the day, using small, frequent sips if large volumes are not tolerated. Sugar-free electrolyte-containing beverages may be beneficial for patients with diabetes who experience significant gastrointestinal losses. Monitoring urine color (aiming for pale yellow) provides a simple assessment of hydration status.
Symptomatic treatment may include antiemetics for nausea, though patients should consult with their healthcare provider before using over-the-counter options, as some products (such as those containing bismuth subsalicylate) may not be appropriate for all patients. Acetaminophen can be used for headache, and adequate rest should be prioritized during the initial adjustment period.
Injection technique optimization may reduce injection site reactions. Patients should rotate injection sites (abdomen, thigh, or upper arm), allow the medication to reach room temperature before injection, and ensure proper technique. The medication should be administered on the same day each week, though the time of day can be adjusted if certain timing reduces side effects.
Patients experiencing persistent fatigue or malaise should ensure adequate caloric intake despite reduced appetite, as excessive caloric restriction can worsen systemic symptoms. Working with a registered dietitian can help patients maintain nutritional adequacy while achieving weight loss goals. Regular follow-up with healthcare providers allows for ongoing assessment and adjustment of management strategies as needed.
No, flu-like symptoms are not listed as common adverse effects in FDA prescribing information for tirzepatide. The most common side effects are gastrointestinal, including nausea, diarrhea, and vomiting, though fatigue is documented in the labeling.
Patients may experience symptoms they interpret as flu-like due to dehydration from gastrointestinal side effects, metabolic adaptation to reduced caloric intake, or heightened symptom awareness. These are distinct from true influenza or viral illness.
Contact your healthcare provider for fever above 100.4°F, severe or persistent vomiting lasting more than 24-48 hours, signs of dehydration (decreased urine output, severe dizziness), severe abdominal pain, or respiratory symptoms, as these may indicate infection or complications requiring evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.