LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management. While this medication has demonstrated significant efficacy in glycemic control and weight reduction, patients may wonder about potential cardiovascular effects, particularly heart palpitations. Understanding the relationship between tirzepatide and cardiac symptoms is essential for safe medication use. This article examines the clinical evidence on tirzepatide and heart palpitations, reviews cardiovascular safety data from clinical trials, and provides guidance on when to seek medical attention and how to manage potential side effects during treatment.
Quick Answer: Heart palpitations are not listed as a common side effect of tirzepatide in FDA prescribing information, and clinical trials have not established a direct causal link between tirzepatide use and palpitations.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works through a dual mechanism of action that targets two key incretin hormone pathways. By activating GIP receptors, tirzepatide enhances insulin secretion and may influence glucose metabolism in peripheral tissues. Simultaneously, GLP-1 receptor activation stimulates glucose-dependent insulin release from pancreatic beta cells, suppresses inappropriate glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways. This combined approach results in improved glycemic control and significant weight reduction.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on the indication and individual patient response. The medication is initiated at a lower dose and gradually titrated upward to minimize gastrointestinal side effects, which are the most commonly reported adverse reactions. Clinical trials have demonstrated substantial reductions in hemoglobin A1c levels (up to 2.5% reduction at the highest doses) and body weight (up to 20% reduction in patients with obesity without diabetes in the SURMOUNT-1 trial).
The pharmacokinetic profile of tirzepatide includes a half-life of approximately five days, allowing for convenient weekly dosing. The medication is primarily eliminated through proteolytic degradation. No dosage adjustment is recommended for renal or hepatic impairment, though patients should be monitored for dehydration-related acute kidney injury during significant gastrointestinal adverse effects.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity. Tirzepatide is not indicated for type 1 diabetes and should not be used with other GLP-1 receptor agonists.
Heart palpitations are not listed as a common adverse effect in the FDA-approved prescribing information for tirzepatide, and there is no established direct causal link between tirzepatide use and palpitations in the pivotal clinical trial data. The SURPASS clinical trial program, which evaluated tirzepatide in over 10,000 patients with type 2 diabetes, did not identify palpitations as a significant safety signal. The most frequently reported adverse effects were gastrointestinal in nature, including nausea, diarrhea, vomiting, and constipation.
However, cardiovascular effects warrant careful consideration in the context of tirzepatide therapy. According to the FDA prescribing information, tirzepatide is associated with modest increases in heart rate (average 2-4 beats per minute), consistent with the class effect observed with GLP-1 receptor agonists. It's important to note that as of 2024, tirzepatide does not have an FDA-approved cardiovascular risk-reduction indication, and dedicated cardiovascular outcomes trials are still ongoing.
When patients report palpitations while taking tirzepatide, several indirect mechanisms may be responsible. Dehydration secondary to gastrointestinal side effects (vomiting and diarrhea) can cause fluid and electrolyte imbalances that may trigger compensatory tachycardia that patients perceive as palpitations. Additionally, improved glycemic control may alter autonomic nervous system function in patients with longstanding diabetes.
It is important to distinguish between true cardiac arrhythmias and the subjective sensation of palpitations, which may represent heightened awareness of normal heartbeats, anxiety, or other non-cardiac causes. The SURPASS clinical trials included patients with stable cardiovascular disease, though those with unstable or severe cardiovascular conditions were typically excluded. Patients with pre-existing cardiovascular risk factors should be monitored appropriately when initiating tirzepatide therapy, particularly during dose escalation when gastrointestinal effects are most pronounced.
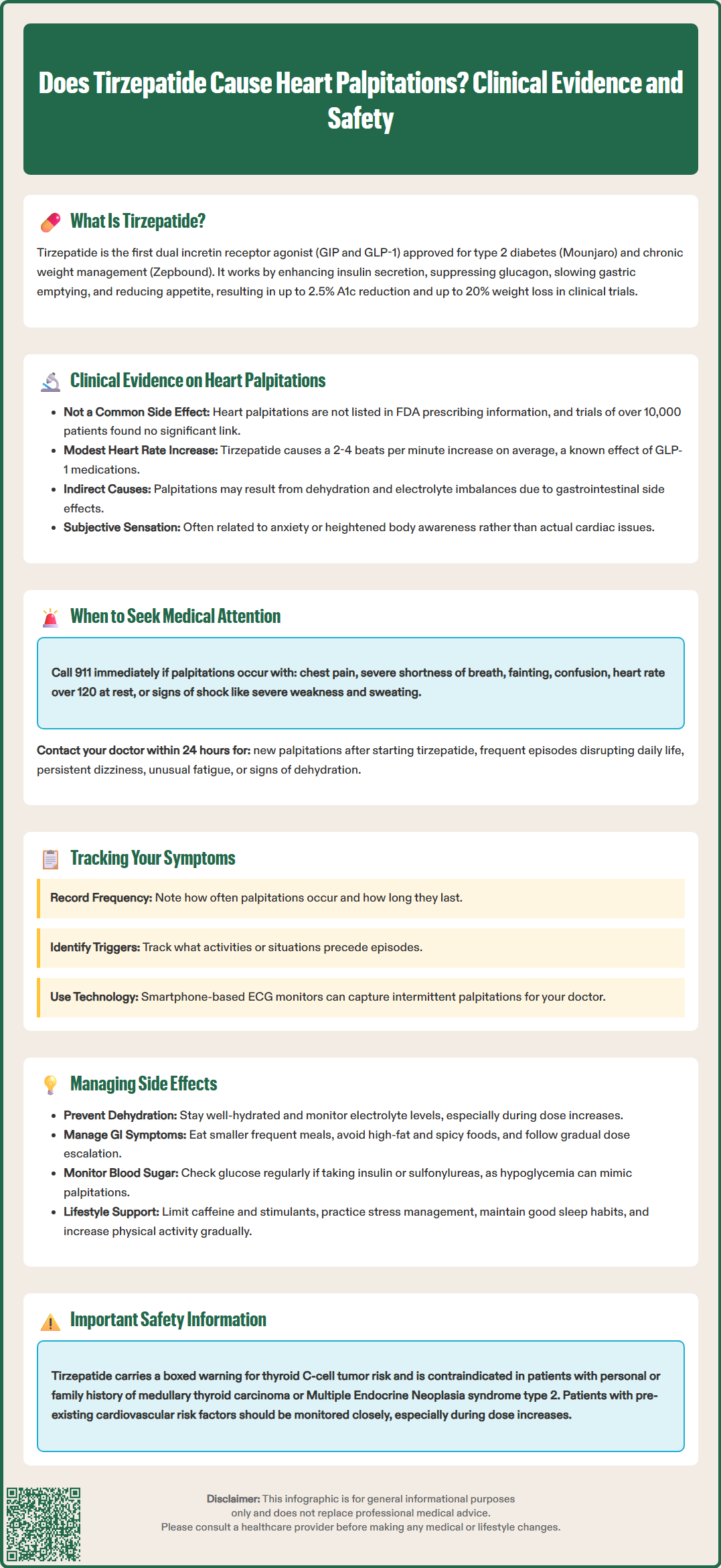
While palpitations are not a recognized common side effect of tirzepatide, patients experiencing this symptom should be evaluated to determine the underlying cause and assess whether urgent medical attention is required. Certain characteristics of palpitations warrant immediate emergency evaluation, and patients should be counseled on these warning signs when initiating tirzepatide therapy.
Seek immediate medical attention (call 911 or go to the emergency department) if palpitations are accompanied by:
Chest pain, pressure, or tightness
Severe shortness of breath or difficulty breathing
Loss of consciousness, syncope, or severe dizziness
Sudden onset of confusion or difficulty speaking
Sustained very rapid heart rate at rest (e.g., >120 beats per minute)
Signs of hemodynamic instability (severe weakness, pallor, sweating)
Contact your healthcare provider within 24 hours if you experience:
New onset of palpitations after starting tirzepatide
Palpitations that are frequent, bothersome, or interfering with daily activities
Associated symptoms such as persistent lightheadedness, unusual fatigue, or exercise intolerance
Palpitations accompanied by excessive thirst, decreased urination, or signs of dehydration
Any palpitations in the context of known structural heart disease or previous arrhythmias
For patients with a history of cardiovascular disease, including coronary artery disease, heart failure, or documented arrhythmias, a lower threshold for evaluation is appropriate. These individuals should maintain close communication with their cardiology and endocrinology providers when initiating or titrating tirzepatide. Baseline electrocardiography may be considered in high-risk populations with pre-existing cardiovascular conditions, though this is not routinely required for all patients.
Documentation of palpitation characteristics can assist healthcare providers in determining appropriate evaluation. Patients should note the frequency, duration, pattern (regular versus irregular), associated activities or triggers, and any accompanying symptoms. Mobile health technologies, including smartphone-based ECG monitors, may provide valuable diagnostic information when palpitations are intermittent and difficult to capture during scheduled appointments.
Effective management of tirzepatide therapy requires a comprehensive approach to minimize adverse effects and optimize therapeutic outcomes. While palpitations are not a typical side effect, addressing common adverse reactions and maintaining overall health can reduce the likelihood of secondary complications that might manifest as cardiac symptoms.
Gastrointestinal side effect management is paramount, as nausea, vomiting, and diarrhea can lead to dehydration and electrolyte imbalances that may contribute to palpitations. Patients should be advised to eat smaller, more frequent meals, avoid high-fat and spicy foods, and stay well-hydrated. Anti-emetic medications may be prescribed for persistent nausea. The gradual dose titration schedule recommended in the prescribing information helps minimize gastrointestinal intolerance.
Hydration and electrolyte monitoring are essential components of safe tirzepatide use. Patients should aim for adequate fluid intake (individualized based on their specific needs and medical conditions) and consume electrolyte-rich foods or beverages, particularly during dose escalation periods. Healthcare providers should consider checking serum electrolytes in patients experiencing significant gastrointestinal side effects or those reporting palpitations. Patients with heart failure or chronic kidney disease may require individualized fluid intake recommendations.
Monitoring for hypoglycemia is important, particularly in patients taking tirzepatide in combination with insulin or sulfonylureas. While tirzepatide itself has a low intrinsic risk of hypoglycemia due to its glucose-dependent mechanism, concurrent medications may require dose adjustments. Symptoms of hypoglycemia, including tremor and palpitations, can be mistaken for primary cardiac symptoms. Blood glucose monitoring and appropriate medication adjustments can prevent these episodes.
Regular follow-up and communication with healthcare providers facilitate early identification and management of adverse effects. Patients should attend scheduled appointments for weight monitoring, metabolic parameter assessment, and medication titration. Patients should be counseled to promptly report symptoms of pancreatitis (severe abdominal pain, sometimes radiating to the back), gallbladder disease, or signs of acute kidney injury. Women of childbearing potential should be advised to use non-oral contraception or add a backup method for 4 weeks after initiation and after each dose escalation due to tirzepatide's effect on gastric emptying.
Lifestyle modifications support successful tirzepatide therapy and overall cardiovascular health. Gradual increases in physical activity, as tolerated during weight loss, should be encouraged with appropriate medical clearance. Patients should be counseled to avoid excessive caffeine and stimulant use, which can exacerbate palpitations. Stress management techniques and adequate sleep hygiene contribute to autonomic nervous system balance and may reduce palpitation frequency in susceptible individuals.
No, heart palpitations are not listed as a common adverse effect in FDA prescribing information for tirzepatide. The SURPASS clinical trials involving over 10,000 patients did not identify palpitations as a significant safety signal, with gastrointestinal effects being the most frequently reported adverse reactions.
Yes, tirzepatide is associated with modest increases in heart rate, averaging 2-4 beats per minute, which is consistent with the class effect observed with GLP-1 receptor agonists. This increase is generally not clinically significant for most patients.
Seek immediate emergency care if palpitations occur with chest pain, severe shortness of breath, loss of consciousness, or sustained rapid heart rate. Contact your healthcare provider within 24 hours for new onset palpitations, frequent episodes, or palpitations accompanied by signs of dehydration or lightheadedness.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.