LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide fatigue go away? Many patients starting tirzepatide (Mounjaro, Zepbound) wonder about tiredness during treatment. Tirzepatide is a dual GIP and GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management. While fatigue isn't among the most common side effects in clinical trials, some patients experience low energy, particularly during dose escalation. For most people, fatigue improves as the body adapts to the medication, though the timeline varies. Understanding why fatigue occurs and how to manage it effectively can help patients continue therapy successfully while maintaining quality of life.
Quick Answer: Tirzepatide-related fatigue typically improves as the body adapts to the medication, often within several weeks of maintaining a stable dose, though duration varies considerably between individuals.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While fatigue is not among the most frequently reported adverse reactions in clinical trials, some patients do experience tiredness or low energy during treatment.
Fatigue associated with tirzepatide may manifest as generalized weakness, reduced stamina, or difficulty maintaining usual activity levels. It is important to distinguish between fatigue potentially related to the medication and tiredness resulting from related factors such as caloric restriction, rapid weight loss, or metabolic changes. In patients with diabetes, hypoglycemia (particularly when tirzepatide is combined with insulin or sulfonylureas) can also contribute to fatigue symptoms.
Understanding the context of fatigue is essential for appropriate management. Patients initiating tirzepatide often experience significant appetite suppression and reduced caloric intake, which can contribute to energy depletion. Additionally, the medication's effects on gastric emptying and glucose metabolism may influence energy levels, particularly during the dose-escalation phase. Healthcare providers should assess fatigue comprehensively, considering both medication-related and lifestyle factors to provide appropriate guidance.
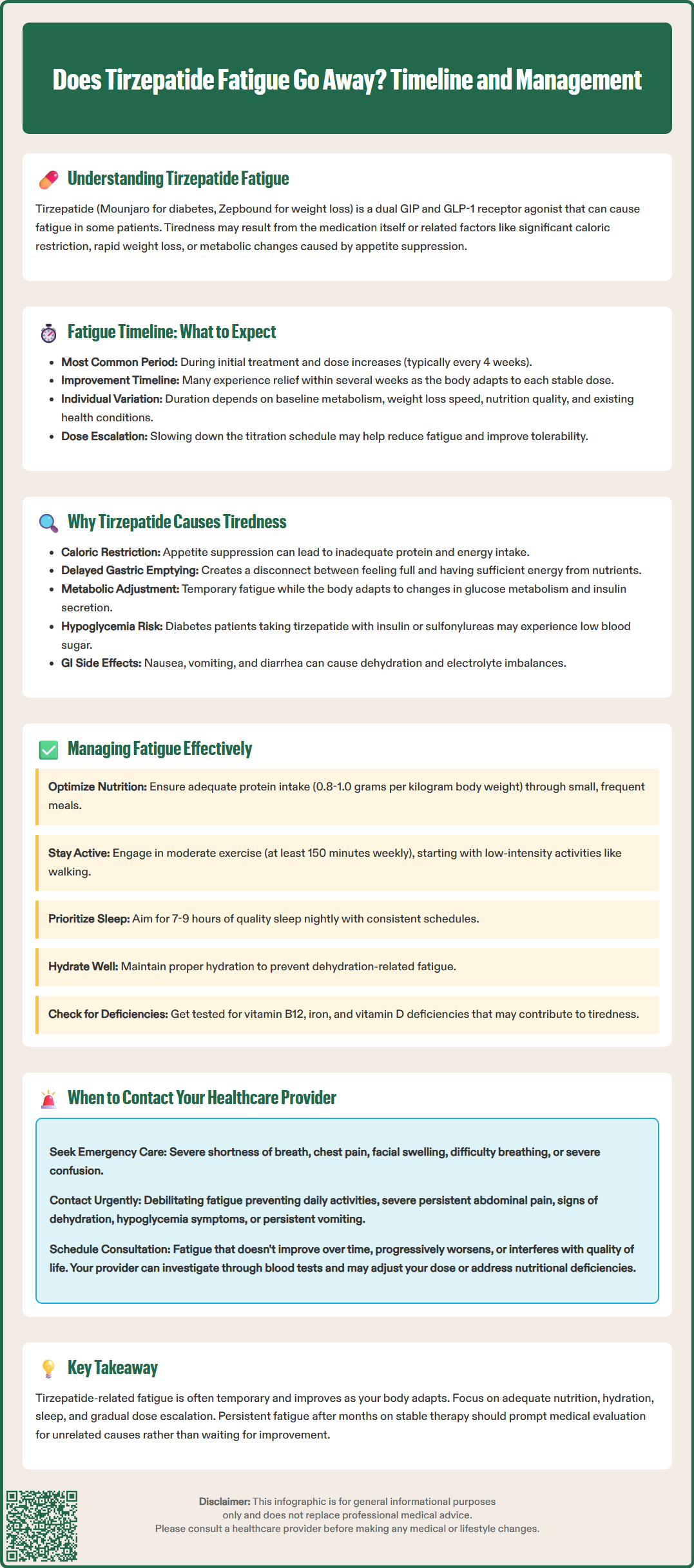
The duration of fatigue with tirzepatide varies considerably between individuals. For many patients who experience fatigue, symptoms may improve as the body adapts to the medication, though the timeline for resolution is highly variable. Fatigue is often most noticeable during the initial dose-escalation period and may recur with each dose increase (typically every 4 weeks per FDA-approved dosing).
Some patients report improvement in energy levels within several weeks of maintaining a stable dose, while others may experience longer periods of adaptation. It's important to note that the FDA-approved titration schedule allows flexibility, and slower dose escalation may help manage side effects including fatigue.
Factors influencing duration include baseline metabolic status, rate of weight loss, nutritional adequacy, concurrent medications, and underlying medical conditions. Patients experiencing persistent or severe fatigue should not wait for spontaneous resolution but should discuss symptoms with their healthcare provider, who may recommend evaluation sooner rather than later.
It is important to note that fatigue occurring after months of stable therapy may not be related to tirzepatide itself. New-onset or worsening fatigue in established users warrants investigation for alternative causes, including thyroid dysfunction, anemia, vitamin deficiencies, or other medical conditions that may have developed independently of the medication.
Several potential mechanisms may contribute to fatigue during tirzepatide treatment, though the exact causes are not fully established. Understanding these possible factors can help address fatigue more effectively.
Caloric Restriction and Rapid Weight Loss: Tirzepatide produces significant appetite suppression through central and peripheral mechanisms. Many patients experience marked reductions in caloric intake, sometimes consuming substantially fewer calories than their metabolic needs. This energy deficit, while promoting weight loss, can result in fatigue, particularly if protein intake is inadequate or weight loss occurs too rapidly.
Delayed Gastric Emptying: Tirzepatide slows gastric emptying, which contributes to satiety but may also affect the timing of nutrient delivery and postprandial energy availability. Some patients report feeling physically full yet energetically depleted.
Metabolic Changes: The medication's effects on glucose metabolism, insulin secretion, and glucagon suppression may temporarily affect energy substrate utilization as the body adjusts to improved glycemic control.
Hypoglycemia Risk: In patients with diabetes, particularly those also taking insulin or sulfonylureas, tirzepatide can increase the risk of hypoglycemia, which manifests with fatigue, weakness, and other symptoms.
Dehydration and Electrolyte Imbalance: Gastrointestinal side effects, particularly nausea, vomiting, and diarrhea, can lead to dehydration and electrolyte disturbances that manifest as fatigue. Maintaining adequate hydration is essential during tirzepatide therapy.
While mild, transient fatigue during tirzepatide initiation is generally not concerning, certain presentations warrant prompt medical evaluation. Patients should contact their healthcare provider if fatigue is severe, persistent, or accompanied by other symptoms that may indicate serious complications.
Call 911 or go to the emergency department immediately for:
Severe shortness of breath, chest pain, or palpitations
Signs of severe allergic reaction: swelling of face, lips, tongue, or throat; hives; difficulty breathing
Severe confusion, loss of consciousness, or inability to stay awake
Contact your healthcare provider urgently for:
Severe, debilitating fatigue that prevents normal daily activities or work
Severe, persistent abdominal pain (especially radiating to the back, with or without vomiting), which may indicate pancreatitis
Signs of dehydration: decreased urination, dark urine, dizziness, dry mouth, or confusion
Symptoms of hypoglycemia: shakiness, sweating, confusion, or rapid heartbeat, particularly in patients taking insulin or sulfonylureas
Persistent nausea or vomiting preventing adequate fluid or food intake
Jaundice, dark urine, or right upper abdominal pain, which may suggest hepatobiliary complications
Routine consultation is appropriate for:
Fatigue that persists without improvement
Progressive worsening of energy levels after initial improvement
Fatigue interfering with medication adherence or quality of life
Concerns about nutritional adequacy or excessive weight loss (>2 pounds per week consistently)
New symptoms developing alongside fatigue, such as cold intolerance, hair loss, or mood changes
Healthcare providers can assess for alternative causes of fatigue through targeted history, physical examination, and laboratory investigations including complete blood count, comprehensive metabolic panel, thyroid function tests, vitamin B12 levels, and iron studies when indicated. Adjusting the tirzepatide dose, optimizing nutritional intake, or addressing concurrent medical conditions may be necessary.
Effective management of tirzepatide-associated fatigue involves a multifaceted approach addressing nutritional, lifestyle, and medical factors. Most patients can successfully continue therapy while implementing strategies to improve energy levels.
Nutritional Optimization: Ensuring adequate caloric and protein intake is fundamental. Caloric needs vary by individual based on height, weight, activity level, and medical conditions. Consultation with a registered dietitian can help develop an appropriate eating plan that provides sufficient energy while supporting weight management goals. Protein needs (generally 0.8-1.0 grams per kilogram body weight, with adjustments for kidney disease) should be prioritized. Small, frequent meals may be better tolerated than large meals given the medication's effects on gastric emptying.
Hydration: Maintaining adequate fluid intake helps prevent dehydration-related fatigue. Fluid needs vary by individual, with factors such as body size, activity level, climate, and medical conditions (particularly heart failure or kidney disease) affecting requirements. Patients experiencing gastrointestinal side effects should pay particular attention to hydration status.
Physical Activity: While counterintuitive, regular moderate exercise often improves energy levels. Starting with low-intensity activities such as walking and gradually increasing duration and intensity can enhance overall stamina without exacerbating fatigue. The American Diabetes Association and U.S. Department of Health and Human Services recommend at least 150 minutes of moderate-intensity activity weekly.
Sleep Hygiene: Ensuring adequate, quality sleep (7 to 9 hours nightly) supports energy restoration. Establishing consistent sleep schedules and addressing sleep disorders if present can significantly impact daytime energy.
Medication Timing: Some patients find that taking tirzepatide at a specific time of day helps minimize fatigue, though this is based on individual preference rather than clinical evidence.
Dose Adjustment: If fatigue is severe or persistent, healthcare providers may consider slowing the dose-escalation schedule (FDA labeling allows for flexible titration with 2.5 mg increments no more frequently than every 4 weeks) or maintaining a lower maintenance dose that balances therapeutic benefit with tolerability.
Monitoring and Supplementation: Regular monitoring of nutritional status may identify deficiencies requiring supplementation. Vitamin B12, iron, and vitamin D deficiencies can contribute to fatigue and should be corrected if identified. However, routine supplementation without documented deficiency is not recommended.
Patients should maintain open communication with their healthcare team throughout treatment, reporting changes in energy levels and discussing concerns about medication tolerability. With appropriate management strategies, most patients can successfully navigate the adjustment period and achieve therapeutic goals while maintaining acceptable energy levels.
Fatigue duration varies between individuals, but many patients experience improvement within several weeks of maintaining a stable dose. Fatigue is often most noticeable during initial dose escalation and may recur with each dose increase, which typically occurs every 4 weeks per FDA-approved dosing schedules.
Tirzepatide-related fatigue may result from several factors including significant caloric restriction due to appetite suppression, delayed gastric emptying affecting nutrient delivery, metabolic changes as the body adjusts to improved glycemic control, potential hypoglycemia (especially when combined with insulin or sulfonylureas), and dehydration from gastrointestinal side effects.
Contact your healthcare provider urgently if fatigue is severe and debilitating, prevents normal activities, persists without improvement, or occurs with warning signs such as severe abdominal pain, dehydration symptoms, hypoglycemia signs, persistent vomiting, or jaundice. Seek emergency care immediately for chest pain, severe shortness of breath, or signs of severe allergic reaction.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.