LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP and GLP-1 receptor agonist that some patients report causes tiredness, particularly during initial treatment weeks. While fatigue is not among the most common adverse reactions in FDA-approved labeling, it may result from reduced caloric intake, gastrointestinal side effects causing dehydration, blood glucose fluctuations, or metabolic adjustments during weight loss. Understanding why tiredness occurs and how to manage it effectively can help patients continue benefiting from tirzepatide's therapeutic effects while maintaining quality of life.
Quick Answer: Tiredness on tirzepatide typically results from reduced caloric intake, dehydration from gastrointestinal side effects, or metabolic adjustments, and usually improves after 4–8 weeks with proper nutrition and hydration.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes (Mounjaro) and chronic weight management (Zepbound). While fatigue is not among the most common adverse reactions in clinical trials, some patients report feeling tired during treatment, particularly in the initial weeks.
Several mechanisms may contribute to tiredness on tirzepatide. The medication slows gastric emptying and reduces appetite, which can lead to significantly decreased caloric intake. When patients consume fewer calories than their body requires for daily activities, fatigue may develop as an adaptive response. Additionally, tirzepatide's effects on blood glucose regulation may cause fluctuations that some individuals perceive as tiredness, especially if glucose levels drop lower than their previous baseline.
Dehydration represents another potential contributor to fatigue. Gastrointestinal side effects such as nausea, vomiting, and diarrhea—which occur in a substantial proportion of patients—can lead to fluid and electrolyte losses. These effects are typically most pronounced during dose escalation periods. Furthermore, rapid weight loss itself can temporarily affect energy levels as the body adjusts to metabolic changes.
It's worth noting that tirzepatide has a low risk of hypoglycemia when used alone, but this risk increases when combined with insulin or sulfonylureas, which could contribute to fatigue symptoms in some patients. The tiredness experienced by some patients likely reflects both direct medication effects and indirect consequences of the medication's therapeutic actions on appetite, food intake, and metabolism.
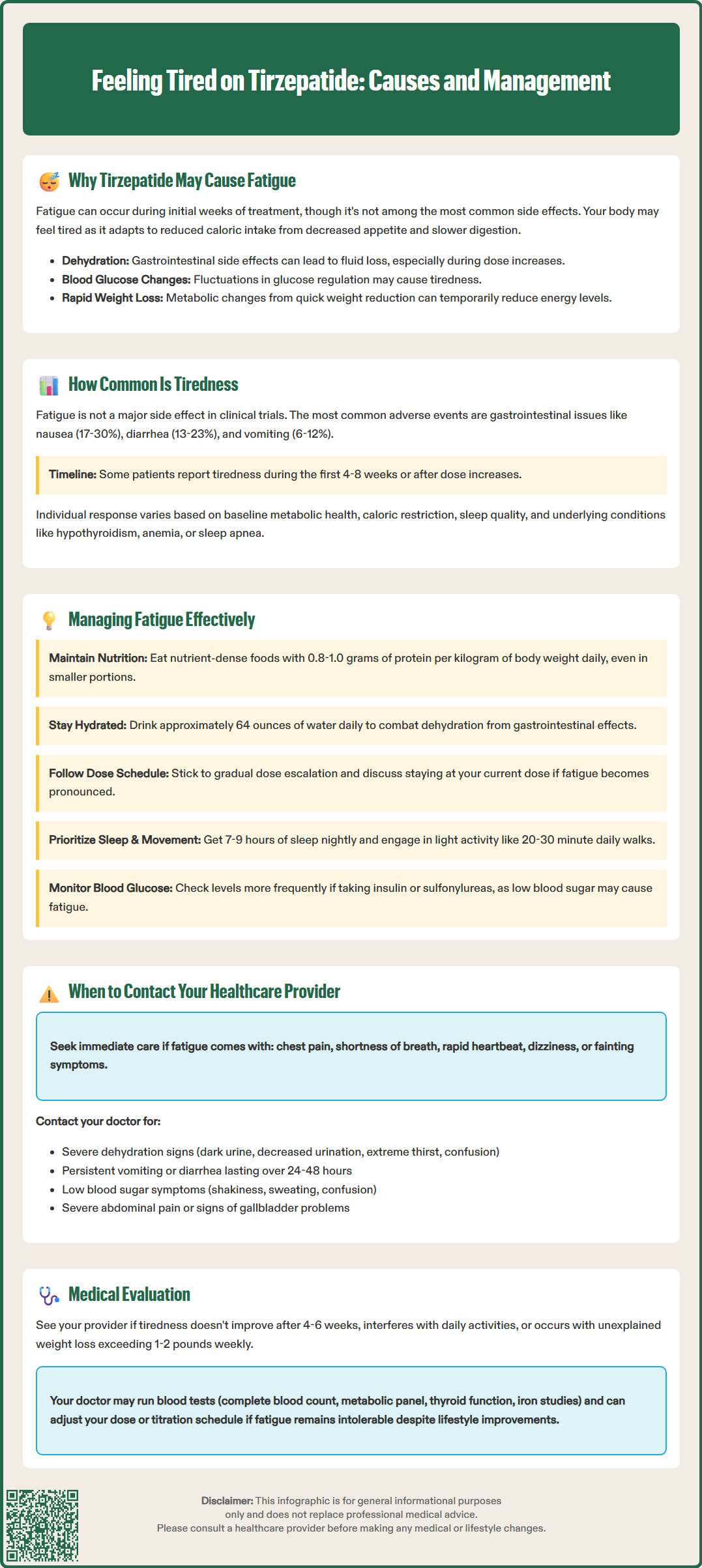
Fatigue is not prominently featured in the adverse event profile reported in tirzepatide's pivotal clinical trials. In the SURPASS clinical trial program for type 2 diabetes, the most frequently reported side effects were gastrointestinal in nature. According to the Mounjaro Prescribing Information, these include nausea (17-22%), diarrhea (13-17%), decreased appetite (10-14%), vomiting (6-10%), constipation (5-7%), and dyspepsia (5-7%).
Similarly, in the SURMOUNT trials for weight management, Zepbound's label reports gastrointestinal events as the most common adverse reactions, with nausea (24-30%), diarrhea (18-23%), vomiting (8-12%), and constipation (11-17%) occurring at somewhat higher rates than in diabetes trials.
While specific fatigue rates are not prominently highlighted in the FDA-approved labeling, post-marketing surveillance and patient-reported experiences suggest that some individuals do experience tiredness, particularly during the first 4–8 weeks of treatment or following dose increases. The prevalence appears to be higher among patients who experience significant gastrointestinal symptoms or those achieving rapid weight loss.
Individual variation in response to tirzepatide is considerable. Factors such as baseline metabolic health, degree of caloric restriction, concurrent medications, sleep quality, and underlying medical conditions all influence whether a patient experiences fatigue. Patients with pre-existing conditions associated with tiredness, such as hypothyroidism, anemia, or sleep apnea, may be more susceptible to experiencing or noticing increased fatigue during tirzepatide treatment.
If you experience tiredness while taking tirzepatide, several practical strategies may help manage this symptom while continuing to benefit from the medication's therapeutic effects.
Nutritional adequacy is paramount. Despite reduced appetite, ensure you consume sufficient calories to meet your body's basic energy requirements. Focus on nutrient-dense foods that provide sustained energy: lean proteins, whole grains, fruits, vegetables, and healthy fats. Aim for balanced meals even if portions are smaller than before starting tirzepatide. Consider consulting a registered dietitian who can develop a meal plan that accommodates your reduced appetite while preventing excessive caloric deficit. Protein intake is particularly important—generally target 0.8–1.0 grams per kilogram of body weight daily (or as recommended by your healthcare provider based on your individual needs, especially if you have kidney disease).
Hydration requires deliberate attention. Most people should aim for about 64 ounces (approximately 2 liters) of water daily, though this should be individualized based on your medical conditions—those with heart failure or kidney disease may need different targets as advised by their healthcare provider. Increase fluid intake if you experience diarrhea or vomiting. Dehydration can significantly contribute to fatigue, and the gastrointestinal effects of tirzepatide increase this risk. Electrolyte-containing beverages may be beneficial if you have persistent gastrointestinal symptoms, though avoid high-sugar options.
Gradual dose escalation as prescribed by your healthcare provider allows your body to adapt to the medication. Do not rush dose increases; the standard titration schedule exists specifically to minimize side effects. If fatigue is pronounced with a dose increase, discuss with your provider whether temporarily remaining at your current dose might be appropriate.
Sleep hygiene and physical activity both play crucial roles. Maintain consistent sleep schedules, aiming for 7–9 hours nightly. Regular physical activity, even light walking for 20–30 minutes daily, can paradoxically improve energy levels and combat fatigue. Start slowly if you're experiencing tiredness, gradually increasing activity as tolerated.
Blood glucose monitoring may be important, especially if you take tirzepatide with insulin or sulfonylureas. More frequent monitoring can help identify if low blood sugar is contributing to fatigue, and your provider may need to adjust doses of these medications to prevent hypoglycemia.
While mild fatigue during the initial weeks of tirzepatide treatment may resolve with supportive measures, certain situations warrant prompt medical evaluation. Understanding when tiredness represents a normal adjustment versus a concerning development is essential for patient safety.
Seek medical attention if you experience:
Severe or worsening fatigue that interferes with daily activities or does not improve after 4–6 weeks of treatment
Fatigue accompanied by other concerning symptoms such as chest pain, shortness of breath, rapid heartbeat, dizziness, or fainting (seek emergency care for these symptoms)
Signs of dehydration including dark urine, decreased urination, extreme thirst, dry mouth, or confusion (severe dehydration requires urgent evaluation)
Symptoms suggesting hypoglycemia (low blood sugar) such as shakiness, sweating, confusion, or irritability, particularly if you take tirzepatide with insulin or sulfonylureas
Persistent vomiting or diarrhea lasting more than 24–48 hours, which increases risk of dehydration and electrolyte imbalances
Severe, persistent abdominal pain (possibly radiating to the back), with or without vomiting, which could indicate pancreatitis
Right upper quadrant abdominal pain, fever, or yellowing of skin/eyes, which may suggest gallbladder problems
Unexplained weight loss exceeding 1-2 pounds per week consistently, suggesting excessive caloric deficit
New or worsening depression or mood changes, as fatigue can sometimes reflect psychological rather than physical causes
Your healthcare provider may evaluate persistent fatigue with appropriate tests based on your specific symptoms and medical history. These might include complete blood count (to assess for anemia), comprehensive metabolic panel (to evaluate electrolytes, kidney function, and glucose levels), thyroid function tests, iron studies including ferritin, and possibly other tests as clinically indicated.
If fatigue proves intolerable despite optimization of nutrition, hydration, and lifestyle factors, your provider may consider adjusting your tirzepatide dose, slowing the titration schedule, or exploring alternative treatment options. However, many patients find that fatigue improves significantly after the first 4–8 weeks as their body adapts to the medication and they establish sustainable eating and hydration patterns. Open communication with your healthcare team ensures that tiredness is appropriately evaluated and managed while maximizing the benefits of tirzepatide therapy.
Most patients experience improvement in fatigue after 4–8 weeks as their body adapts to the medication and they establish sustainable eating and hydration patterns. Tiredness is typically most pronounced during initial treatment or following dose increases.
Tirzepatide has a low risk of hypoglycemia when used alone, but this risk increases when combined with insulin or sulfonylureas, which can contribute to fatigue. Blood glucose monitoring may help identify if low blood sugar is causing tiredness, and medication adjustments may be needed.
Do not stop tirzepatide without consulting your healthcare provider. Contact them if fatigue is severe, interferes with daily activities, persists beyond 4–6 weeks, or occurs with concerning symptoms like chest pain, shortness of breath, or signs of dehydration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.